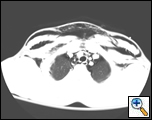
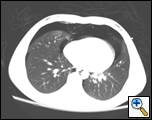
The patient is a 16-year-old male who was a restrained passenger in a car that collided with a guardrail at high speed. He was initially admitted to the referring hospital with no respiratory symptoms and with oxygen saturations over 90%. CT scan revealed a posterior membranous tracheal tear approximately 4 cm above the tracheal bifurcation, pneumomediastinum, and bilateral pneumothoraces. Upon arrival to our Level One Trauma Center, the patient was found to be hemodynamically stable, breathing spontaneously with oxygen saturations of 100% on 2L nasal cannula. His exam was remarkable for subcutaneous emphysema extending from his upper chest to his head, neck and throat. He had a seatbelt bruise across the front of his chest (Figure 1). The remainder of his exam was significant only for a left ankle injury. Review of his CT scan showed extensive mediastinal and subcutaneous emphysema, bilateral pneumothoraces and a posterior linear membranous tracheal tear starting from 2.5cm below the thoracic inlet and extending down 5cm above the carina (Figures 2a and b). Bronchoscopic intubation was performed confirming the CT scan findings and revealing no evidence of distal airway injury. The endotracheal tube was advanced across the area of injury under direct visualization.
The patient was emergently taken to the operating room where a left chest tube was placed and then a right posterolateral thoracotomy was performed under total intravenous anesthesia. Bronchoscopy was then used to direct the endotracheal tube into the left mainstem bronchus to obtain single lung
 |
| Figure 3: Posterolateral Thoracotomy with Rib Excision: Intercostal Muscle flap for buttressing of the posterior tracheal repair |
ventilation. A 5th rib excision was performed at thoracotomy to facilitate the takedown of an intercostal muscle flap pedicle for buttressing of the tracheal repair (Figure 3). Upon entry into the chest, there was extensive mediastinal emphysema obliterating tissue planes. Dissection of the posterior mediastinal pleural was commenced from the level below the carina, anterior to the esophagus, and posterior to the right mainstem bronchus. This dissection was continued around the azygous vein and then up to the thoracic inlet, after division of the azygous vein. The esophagus was dissected anteriorly, mobilizing it away from the trachea while maintaining visualization of the carina and the both mainstem bronchi. A nasogastric tube placed in the esophagus was used to administer methylene blue, which revealed no evidence of esophageal perforation. The dissection was continued superiorly, identifying the vagus and protecting the right recurrent laryngeal nerve. Local hemorrhage and emphysematous changes to the tissue planes made the dissection difficult. Further mobilization of the posterior portion of the trachea up to the thoracic inlet provided visualization of the superior extent of the injury (Figure 4). This was a longitudinal tear in the membranous portion of the trachea starting from 5cm above the carina extending to 2.5cm below the thoracic inlet. The endotracheal tube balloon
 |
| Figure 4: Laceration of the trachea can be clearly seen with the endotracheal tube visible through the tear |
 |
| Figure 5: Repair of laceration. |
was deflated to allow adequate visualization of the tear. The edges of the trachea were debrided and the tear was repaired with two running 4-0 vicryl sutures starting at either end of the tear and meeting in the middle (Figure 5). At the conclusion of the repair, there was no air leak from the suture line at 30 cm water. Next the intercostal muscle flap was inspected and found to be viable. The flap was then positioned anterior to the esophagus and posterior to the trachea, extending from 5cm above the carina and passing superiorly to the thoracic inlet. Interrupted figure-of-eight sutures of 4-0 vicryl were used to anchor the flap to the cartilaginous portion of the trachea. This provided a well-vascularized buttress for the linear repair in the membranous portion of the trachea. (The pleural surface of the flap was placed against the trachea.) Stay sutures of 4-0 vicryl were placed to anchor the muscle flap to the mediastinal pleural just distal to its origin. Lastly, the mediastinal pleural previously reflected was then loosely approximated over the muscle flap. The endotracheal tube was then returned to a standard position and the right lung inflated. The balloon of the endotracheal tube was deflated and no air leak was seen from the site of the repair. The chest was closed and bronchoscopy was performed to clear the airway of secretions, inspect the repair, which was intact, and to position the balloon of the endotracheal tube above the carina but below the injury.
The patient was taken to the intensive care unit still intubated. A few hours later, he underwent bronchoscopy to clear secretions and was extubated. His postoperative stay was uneventful. A follow up flexible bronchoscopy was performed on postoperative day (POD) # 6 revealing a healing suture line on the membranous region of the trachea (Figure 6). The patient’s chest tube demonstrated a small air leak on POD # 7 and he was discharged with the tube connected to a minipleurovac on POD # 8. He underwent bronchoscopy one week later, which revealed a healed suture line with minimum granulation tissue (Figure 7); furthermore, there was no evidence of air leak and the chest tube was removed.
 |
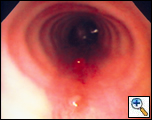 |
| Figure 6: Bronchoscopic view of repair on post-operative day #6. | Figure 7: Bronchoscopic view of the repair at 2 weeks. |
DISCUSSION
Blunt traumatic tracheal laceration is a rare injury that requires surgical intervention in nearly all cases [1]. While small lacerations can be managed non-operatively, large tears require definitive surgical repair [2]. The natural history of these lacerations is that the injury heals itself with severe scarring and ultimately stenosis of the trachea. In carinal and subcarinal tears, this leads to collapse of the distal lung. Thus, early surgical intervention is essential to prevent long-term complications of this injury. Ninety percent of these injuries if primarily repaired heal without any sequelae [2-5]. There is no consensus whether this injury is associated with thoracic other injuries [6, 7] however; there is no association with seatbelt bruising over the chest [8]. In most tracheal injuries, the injury occurs around the carina, which is relatively fixed. Our patient sustained a proximal tracheal injury 5 cm above the carina, which is a very unusual location. Possible mechanisms are a hyperextension injury of the trachea against the vertebral column or a sudden increase in intratracheal pressure due to compression of the chest with a closed glottis.
Bronchoscopic visualization is necessary to determine the extent of the injury and also facilitates endotracheal tube positioning, avoiding further injury. Endotracheal tubes can be used to stent across the lesion with bronchoscopic guidance. Alternatively in more distal injuries, jet ventilation through the endotracheal tube or a simple catheter can provide adequate ventilation. We recommend the use of single lumen 7.5 OR 8.0 MM endotracheal tubes as compared to double lumen tubes as the size of the tube may worsen the injury.
Primary repair of these injuries is considered the best treatment; with a buttressed repair to prevent fistula formation to the esophagus or dehiscence leading to recurrent pneumothorax, pneumomediastinum, or stenosis of the airway. A right posterolateral thoracotomy provides good exposure to the trachea, carina, and mainstem bronchi. A rib excision will facilitate harvesting an adequate pedicled intercostal muscle flap. Wide dissection of the trachea provides excellent exposure of the laceration. To repair the injury a limited debridement of the edges should be performed followed by primary repair with interrupted or continuous absorbable sutures. With circumferential tears it is important to minimize debridement that may lead to reduction in length of the overall trachea. These tears should be repaired with interrupted sutures to maintain the size of the tracheal lumen. With longitudinal tears, there is no literature to support either form of suturing. All repairs should be buttressed with a well-vascularized muscle or pericardial fat pad flap to ensure healing of the suture line, limit air leaks or fistula formation [9]. At the completion of the repair, bronchoscopic visualization is performed to insure the repair is adequate. Placement of two chest tubes is standard, with the posterior tube placed near the repair.
Postoperative management of these patients involves early extubation. Patients should undergo bronchoscopy prior to extubation to clear secretions. Bronchoscopy should be performed two weeks after surgery to evaluate the healing of these injuries and assess possible stenosis of the airway.
In conclusion, blunt traumatic tracheal lacerations are rare. Bronchoscopy prior to surgery should be performed to evaluate the lesion. Primary repair of the lesion with tissue buttressing with a pedicled tissue flap should be performed urgently. Postoperatively, bronchoscopy is necessary to follow tracheal healing and possible stenosis.
References
- Tcherveniakov A, Tchalakov P, and Tcherveniakov P. Traumatic and iatrogenic lesions of the trachea and bronchi. Eur J Cardiothorac Surg 2001;19:19-24.
- Mussi A, Ambrogi Mc, Menconi G, Ribechini A, and Angeletti C. Surgical approaches to membranous tracheal wall lacerations. J Thorac Cardiovasc Surg 2000;120:115-8.
- Massard G, Rouge C, Dabbagh A, et al. Tracheobronchial lacerations after intubation and tracheostomy. Ann Thorac Surg 1996;61:1483-7.
- D'odemont Jp, Pringot J, Goncette L, Goenen M, and Rodenstein D. Spontaneous favorable outcome of tracheal laceration. Chest 1991;99:1290-2.
- Orta D, Cousar J, 3rd, Yergin B, and Olsen G. Tracheal laceration with massive subcutaneous emphysema: a rare complication of endotracheal intubation. Thorax 1979;34:665-9.
- Swan K Jr., Swan B, and Swan K Decelerational thoracic injury. J Trauma 2001;51:970-4.
- Baumgartner F, Sheppard B, De Virgilio C, et al. Tracheal and main bronchial disruptions after blunt chest trauma: presentation and management. Ann Thorac Surg 1990;50:569-74.
- Arajarvi E and Santavirta S. Chest injuries sustained in severe traffic accidents by seatbelt wearers. J Trauma 1989;29:37-41.
- Kouerinis I, Loutsidis A, Hountis P, Apostolakis E, and Bellenis I. Treatment of iatrogenic injury of membranous trachea with intercostal muscle flap. Ann Thorac Surg 2004;78:e85-6.