Introduction
The current generation of endovascular stent-grafts are approved exclusively for the treatment of atherosclerotic aneurysms of the descending thoracic aorta. The regulatory process (both in Europe and the United States) through which these devices achieved clinical approval focused on the clear clinical benefit to patients with degenerative aneurysms. In an effort to extend the potential treatment options for these devices, patients with a variety of other diseases of the descending thoracic aorta have been treated in an off-label fashion. Rigorous review of this data has suggested potential clinical benefit in patients with acute Type B aortic dissections with malperfusion along with select other aortic diseases. [1] Additional study and follow-up is needed before additional treatment indications for endovascular stent-grafts can be extended.
Aneurysms associated with chronic type B aortic dissections are fundamentally a different clinical situation compared to degenerative atherosclerotic aneurysms. [2, 3] Fundamentally, the purpose of treating aneurysms of the descending thoracic aorta associated with chronic type B aortic dissections is to prevent continued degeneration of the false lumen by preventing pressurized blood to communicate with the false lumen. In general, this means landing the distal aspect of the stent graft in dissected aorta which means that a complete 360 degree seal is impossible but thrombosis of the false lumen can still occur. The long-term effects and success of this approach are yet to be determined. We describe the successful treatment and mid-term follow-up of a patient with a 5 cm aneurysm of the descending thoracic aorta associated with a chronic type B aortic dissection with endovascular stent graft.
Case Report
A 52-year-old female with a history of untreated hypertension presented with an acute type A aortic dissection. The dissection started just above the aortic root and extended distally through the aortic arch and into the abdominal aorta. She had no signs of malperfusion. She underwent successful surgical replacement of her ascending aorta with an interposition tube graft. At the time of her presentation, there were no signs of aneurismal dilation of the aortic arch or descending thoracic aorta and the aortic dissection distal to the ascending aorta was managed medically. The patient had an uneventful postoperative recovery.
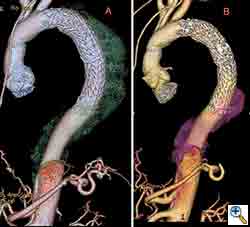
Six months following surgical repair of her acute Type A ascending aortic dissection, a computed tomography (CT) scan of the chest and abdomen demonstrated a new 5cm aneurysm of the proximal descending thoracic aorta. (Figure 1A) The dissection in the aortic arch had stabilized while the false lumen in the proximal descending thoracic aorta beyond the left subclavian artery had degenerated. Distal to the descending thoracic aorta the dissection continued into the abdomen without significant aneurysm formation. Because the aneurysm developed in such a rapid fashion, she was felt to require treatment and was considered a candidate for endovascular repair. The intent of this approach was to seal off the communication to the false lumen proximally and allow the distal false lumen to thrombose over time which would stabilize the false lumen and prevent further expansion.
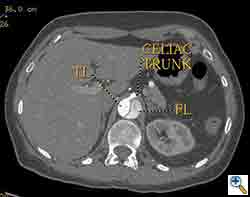
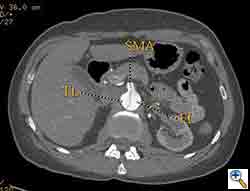
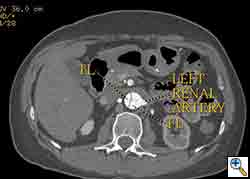
The patient was taken to the hybrid operating suite and a thoracic aortogram was performed. The aortogram confirmed the chronic Type B aortic dissection with a patent false lumen and a fenestration just beyond the left subclavian artery. An intravascular ultrasound (IVUS) was also performed of the entire aortic arch and descending thoracic and abdominal aorta. The IVUS also confirmed that there was an adequate proximal landing zone beyond the left subclavian artery consisting of normal aorta where we would be able to achieve adequate seal of the endovascular stent graft. The septal fenestration began approximately 1.5 cm distal to the left subclavian artery. The true lumen was compressed distally. (Figure 2) The celiac artery appeared to come off the true lumen. (Figure 3) The dissection extended into the superior mesenteric artery and the artery was perfused from both the true and false lumen. (Figure 4) The left renal artery came off the false lumen. (Figure 5) The right renal artery came off the true lumen.
After performing a right groin cutdown and exposing the right common femoral artery, we exchanged our regular .035” guidewire for a stiff .035” guidewire. We used IVUS to confirm that the wire was entirely in the true lumen. We then inserted a 37 mm x 20 cm Gore TAG endoluminal graft over the guidewire and deployed it just beyond the left subclavian artery. We sized the diameter of the endoluminal graft based off of the diameter of the aorta just beyond the left subclavian artery. We allowed a 10% over sizing of the endoluminal graft to permit adequate proximal seal and fixation. Distally this would mean a significant oversizing of the endoluminal graft because the true lumen was significantly compressed. A completion aortogram demonstrated excellent seal proximally with no evidence of filling of the false lumen proximally. Distally there was some retrograde filling of the false lumen which is to be expected. The true lumen was also slightly expanded due to the oversizing of the endograft distally. With IVUS and aortography, we carefully inspected the septum distal to the stent graft above the celiac artery and there were no other signs of active communication between the two lumens.
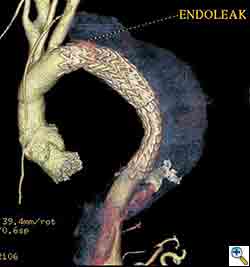
Post-operatively, the patient was extubated in the operating room and managed in the intensive care unit. In order to augment spinal cord perfusion, the patient’s systolic blood pressure was maintained greater than 150 mmHg for 48 hours and the patient experience no post-operative complications. The patient was discharged home on post-operative day 4 and a CT scan of the chest performed 1 month post-operatively showed a small proximal Type I endoleak. (Figure 1B) The rest of the false lumen was thrombosed and the endoleak was localized. (Figure 6) The endoleak was managed medically and a follow-up CT scan of the chest 6 months post-operatively showed improvement of the Type I endoleak and continued thrombosis of the false lumen. (Figure 7) A CT scan of the chest as 12 months and 24 months post-operatively demonstrated complete resolution of the proximal Type I endoleak and the retrograde Type I endoleak. The false lumen distal to the endoluminal graft was also thrombosed distally to the level of the celiac artery. (Figure 8) In addition, the aneurysm was stable and had not changed in size.
Discussion
Endovascular repair of patients with chronic Type B aortic dissection with associated aneurysm of the false lumen is a controversial subject. The most significant concern is gaining proximal seal and preventing continued expansion of the aneurysm. This case demonstrates the fundamental principles involved in choosing a stent-graft. The optimal diameter of the stent-graft should be matched to the diameter of the normal aorta proximal to the dissection. Minimal oversizing of the graft is necessary. At most there should be 10% oversizing. This minimizes the chance for graft infolding and for causing damage to the normal aorta from radial force of the stent-graft. The graft is secured by the dissection septum and unlike an aneurysm there is more contact of graft to aortic tissue. There is no need to taper the graft distally and the size of the graft is irrespective of the distal true lumen size. [4,5,6] In summary, the graft diameter should be sized to the proximal normal aorta and that diameter should be carried distally in the stent-graft despite the diameter of the distal true lumen.
Second, retrograde filling of the false lumen from a distal fenestration in the abdominal aorta is acceptable and should not be considered a failure of the therapy. The purpose of the therapy is to seal all significant fenestrations in the thoracic aorta. Frequently, this is only the proximal entry tear. [7] Sometimes there are no other fenestrations in the thoracic aorta in this scenario no additional coverage of the thoracic aorta is needed other than the proximal stent-graft. When there are other fenestrations, they should be covered. [8] If the true lumen distal to the stent-graft is still significantly compressed, then an additional stent-graft component can be added to the proximal stent-graft. [9]
This case also demonstrates the expected evolution of the aortic lumen and septum. Having 2-year follow-up in this case demonstrates the natural progression of thrombosis which the false lumen can undergo. Careful surveillance is important in these patients. We recommend CT scans every 6 months for the first 3 years following treatment. Reintervention is indicated in patients which don’t thrombose the false lumen after 2 years or who have continued expansion of the false lumen.
Long-term follow-up is essential in these patients. It is unclear whether thrombosis of the false lumen and stabilization of the aortic diameter translates into long-term prevention of aortic rupture. Mid-term results suggest that there is adequate prevention of aneurysm rupture, but larger numbers of treated patients will be needed in order to assess for statistical success. [10] In the meantime, endovascular repair should be considered in high-risk surgical patients with chronic Type B aortic dissections with associated aneurysms of the false lumen. Optimal outcomes are achieved by following a set of endovascular principles which are different than those used for degenerative aneurysm repair.
References
- Akin I, Kische S, Rehders TC, et al. Thoracic endovascular stent-graft therapy in aortic dissection. Curr Opin Cardiol. 2010; epub.
- Czerny M, Roedler S, Fakhimi S, et al. Midterm results of thoracic endovascular aortic repair in patients with aneurysms involving the descending aorta originating from chronic type B dissections. Ann Thorac Surg. 2010;90:90-4.
- Zoli S, Etz CD, Roder F, et al. Long-term survival after open repair of chronic distal aortic dissection. Ann Thorac Surg. 2010;89:1458-66.
- Parsa CJ, Schroder JN, Daneshmand MA, et al. Midterm results for endovascular repair of complicated acute and chronic type B aortic dissection. Ann Thorac Surg. 2010;89:97-102.
- Xu SD, Huang FJ, Yang JF, et al. Early and midterm results of thoracic endovascular aortic repair of chronic type B aortic dissection.J Thorac Cardiovasc Surg. 2010;139:1548-53.
- Manning BJ, Dias N, Ohrlander T, et al. Endovascular treatment for chronic type B dissection: limitations of short stent-grafts revealed at midterm follow-up. J Endovasc Ther. 2009;16:590-7.
- Blount KJ, Hagspiel KD. Aortic diameter, true lumen, and false lumen growth rates in chronic type B aortic dissection. AJR Am J Roentgenol. 2009;192:W222-9.
- Rodriguez JA, Olsen DM, Lucas L, et al. Aortic remodeling after endografting of thoracoabdominal aortic dissection. J Vasc Surg. 2008;47:1188-94.
- Hager E, Moudgill N, Lipman A, et al. Coil-assisted false lumen thrombosis in complicated chronic type B dissection. J Vasc Surg. 2008;48:465-8.
- Czerny M, Zimpfer D, Rodler S, et al. Endovascular stent-graft placement of aneurysms involving the descending aorta originating from chronic type B dissections. Ann Thorac Surg. 2007;83:1635-9.