Introduction
Transhiatal esophagectomy is an effective surgical approach to end-stage benign and malignant esophageal disease, which classically involves replacement of the esophagus with a gastric conduit placed in the posterior mediastinum. We present a patient who underwent transhiatal esophagectomy with a gastric conduit placed in the anterior mediastinum, and subsequently developed dysphagia from compression of her conduit by the left sternoclavicular joint, underscoring the need for prophylactic widening of the thoracic inlet for esophageal replacement via a sub-sternal approach.
Case Presentation
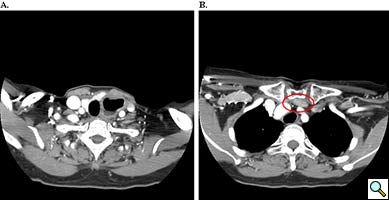
A 67 year old patient with a history of transhiatal esophagectomy (THE) and sub-sternal gastric pull-up ten years prior, at another institution, for early stage esophageal cancer presented with progressive dysphagia to solids. An initial esophagogastroduodenoscopy (EGD) found a large retained food bolus as well as tortuosity and dilatation of the cervical esophagus proximal to the esophagogastric anastomosis. No evidence of intrinsic anastomotic stricture or fibrosis was noted, but there was extrinsic compression. A barium esophagogram revealed significant extrinsic compression of the upper esophagus in the area of the anastomosis at the left clavicular head, with associated narrowing of the lumen and minimal transit of oral contrast (Figure 1). A computed tomography scan of the neck confirmed the sub-sternal location of the gastric pull-up within the anterior mediastinum, and revealed dilatation of the esophagus proximal to the anastomosis, with no associated masses or disease recurrence (Figure 2). The left sternoclavicular joint (SCJ) appeared to be compressing the conduit and was the point of obstruction.
To rule out anastomotic malignant recurrence, a flexible EGD was again performed with fluoroscopic guidance and four quadrant biopsies were taken off the distal cervical esophagus and the proximal gastric conduit. Fluoroscopy confirmed the intraluminal narrowing corresponded to the anatomic location of the left SCJ. The esophageal biopsies revealed squamous epithelium with no evidence of metaplastic, dysplastic, or neoplastic changes and the gastric conduit biopsies were benign as well. Given the absence of recurrent malignancy, the source of the extrinsic compression seen in the imaging of the patient’s cervical esophagogastric anastomosis was secondary to compression by her left SCJ. The patient elected to have the left SCJ resected due to ongoing worsening dysphagia.
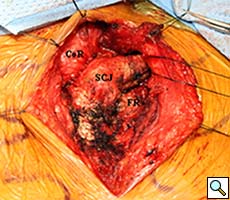
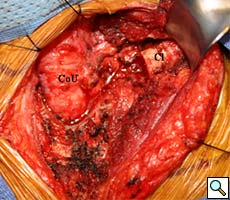
Intraoperatively, the gastric conduit was noted to be intimately compressed by the left SCJ (Figure 3A). The insertion of the sternocleidomastoid and other strap muscles were divided using electrocautery and the conduit was carefully bluntly dissected off the posterior sternum and left SCJ. The manubrial and clavicular segments of the SCJ were then resected, revealing the conduit underneath in good condition (Figure 3B). Care was taken to preserve the left internal mammary artery. Intraoperative EGD confirmed easy passage of the scope through the cervical anastomosis and into the gastric conduit with reduced extrinsic compression. Saline irrigation into the field and air insufflation of the conduit was used to confirm conduit integrity. A Savary-Gilliard guidewire was endoscopically passed and the anastomosis was carefully dilated using 42, 48, and 54 French (Fr) Savary-Gilliard bougie dilators (Cook Medical, Bloomington, IN) with minimal resistance. After removal of the guidewire, a 52 Fr Maloney dilator (Medovations, Milwaukee, WI) was also passed through the conduit without difficulty.
 |
| Figure 4. One year postoperative esophagram showing residual proximal dilatation, but improved transit of contrast through the cervical esophagogastric anastomosis. |
Postoperatively, the patient experienced immediate improvement in the ability to swallow liquids and solids. The patient was discharged on post-operative day two after demonstrating tolerance of a soft mechanical diet. On outpatient follow-up, the patient required an additional bougie dilation. After 1 year, the patient is able to tolerate a solid diet and an esophagram demonstrated improved transit of contrast, with reduced anastomotic narrowing (Figure 4).
Discussion
Esophagectomy without thoracotomy, or transhiatal esophagectomy is an effective surgical approach to malignant and end-stage benign esophageal disease. The advantages of a THE include low morbidity and mortality rates (1). As previously described, THE involves mobilization of the stomach and esophagus through an upper midline abdominal incision and manual positioning of the stomach conduit through the posterior mediastinum. (2) A cervical esophagogastric anastomosis is then performed through a standard left cervical incision.
In this report, we describe the unusual case of a patient who had transhiatal resection of her esophageal cancer with a gastric conduit positioned in the anterior mediastinum by a sub-sternal approach, complicated by eventual extrinsic obstruction of the gastric conduit by the left SCJ. While the sub-sternal route for re-establishing enteric continuity can be valuable when the posterior mediastinum is unavailable, use of the sub-sternal route requires widening of the thoracic inlet. This is accomplished by prophylactic resection of the left sternoclavicular joint, including the left half of the manubrium and clavicular head, in order to enlarge the superior thoracic aperture into the superior mediastinum and prevent proximal graft compression (3-6). Sub-sternal placement of any esophageal replacement also creates anterior angulation at the pericardium which makes subsequent dilations and endoscopies of any conduit more difficult (4).
The clinical example presented in this report illustrates not only the long term success of transhiatal esophagectomy in treating esophageal cancer but also the inherent drawbacks to using a sub-sternal position for the gastric conduit. Although the patient achieved an excellent oncologic outcome, failure to open the thoracic inlet during the patient’s original esophageal resection eventually resulted in conduit compression that later caused severe and intolerable dysphagia. This case demonstrates the importance of performing prophylactic left SCJ resection in operations where a sub-sternal conduit is necessary.
References
- Chang AC, Ji H, Birkmeyer NJ, Orringer MB, Birkmeyer JD. Outcomes after transhiatal and transthoracic esophagectomy for cancer. Ann Thorac Surg. 2008; 85(2):424-9.
- Orringer MB. Transhiatal esophagectomy without thoracotomy. Op Tech Thorac Cardiovasc Surg. 2005; 10(1):63-83.
- Maish MS, DeMeester SR. Indications and technique of colon and jejunal interpositions for esophageal disease. Surg Clin North Am. 2005; 85(3):505-14.
- Orringer MB. Esophageal mythology. J Am Coll Surg. 2008; 207(2):151-63.
- Orringer MB. Sloan H. Substernal gastric bypass of the excluded thoracic esophagus for palliation of esophageal carcinoma. J Thorac Cardiovasc Surg. 1975; 70(5):836-51.
- Orringer MB. Substernal gastric bypass of the excluded esophagus--results of an ill-advised operation. Surgery. 1984; 96(3): 467-70.