ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
VATS Extraction of a Migrating Kirschner Wire Into the Mediastinum and Lung
Boasquevisque CH, Lucas G, Santos A, Rocha L. VATS Extraction of a Migrating Kirschner Wire Into the Mediastinum and Lung. January 2019. doi:10.25373/ctsnet.7614059.
Introduction
Kirschner wires (K-wires) and Steinman pins have been used to fix fractures of the thorax, perhaps less frequently nowadays because of the appearance of better devices such as titanium plates and screws. Migration of these metallic wires and pins into different intrathoracic structures has been reported and may lead to catastrophic events. It is very important to follow up with these patients as long as the wires and pins remain in place.
Here the authors report a case of a K-wire transmediastinal migration into the left upper lobe.
Case Report

Figure 1. Chest radiograph showing the migrating K-wire, used to fix a right clavicular fracture 34 years previously, in the mediastinum.
An asymptomatic 46-year-old man fell down at his workplace and sought medical consultation because of the accident. In the emergency department, a chest radiograph revealed that a K-wire used to fix a right clavicular fracture 34 years previously had migrated through the anterior mediastinum and into the left upper lobe (Figure 1).

Figure 2. A) Chest CT (coronal plane) showing the K-wire perforating the left upper lobe. B) Chest CT (axial plane) showing the K-wire perforating the left upper lobe.
A chest computed tomography (CT) showed that the K-wire migrated through the anterior mediastinum into the left upper lobe (Figures 2A and 2B). In addition, a chest CT showed that the K-wire was encroaching on the left brachiocephalic vein, posing a risk to extraction of the foreign body (Figure 3A), and that it was anterior to the aortic arch (Figure 3B).
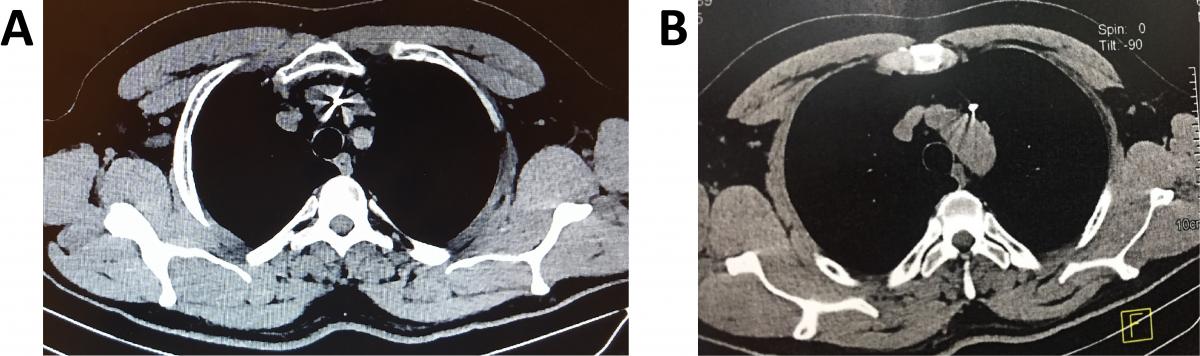
Figure 3. A) Chest CT (axial plane) showing the K-wire encroaching on the left brachiocephalic vein, posing a risk for extraction. B) Chest CT (axial plane) showing the K-wire in the anterior mediastinum in relation to the aortic arch.
Once the diagnosis was made, extraction of the K-wire was planned through a left video-assisted thoracoscopic (VATS) approach as shown in Figures 4-8 and Videos 1 and 2. The patient was intubated with a single lumen endotracheal tube and CO2 insufflation was used (6 – 8 mmHg/4L/min).
The patient’s postoperative recovery was uneventful, and he was discharged on the third postoperative day.
Discussion

Figure 4. VATS approach to remove the K-wire. The authors positioned the ports as for a VATS thymectomy to approach the anterior mediastinum. Patient was placed in the semilateral decubitus position with a roll under the left hemithorax.
The migration of K-wires and Steinman pins used for thoracic osteosynthesis has been reported to occur from the immediate postoperative period to many years after the surgery (1). In the present case, the migration was diagnosed 34 years after the osteosynthesis of a right clavicular fracture. The migration of these metallic foreign bodies has been described to occur to the mediastinum, trachea, lungs, aorta, pulmonary artery, innominate vein, pericardium, heart, esophagus, and spinal cord, leading to fatal complications (1).
The mechanisms of migration are speculative and perhaps multifactorial: a) great freedom of shoulder movements with traction of the muscles on the metallic wires or pins; b) negative intrathoracic pressure; c) respiratory movements; d) gravitational forces; and e) local bone resorption making the wires and pins loose (1, 2).
Video 1. Video showing the left upper lobe adhered to the mediastinal pleura, close to the phrenic nerve.
Video 2. Video demonstrating that the K-wire could be encroaching on the left brachiocephalic vein. At this point no attempt was made to remove the K-wire by traction because of the risk of vascular injury. Urgent sternotomy capability was arranged in case it became necessary.
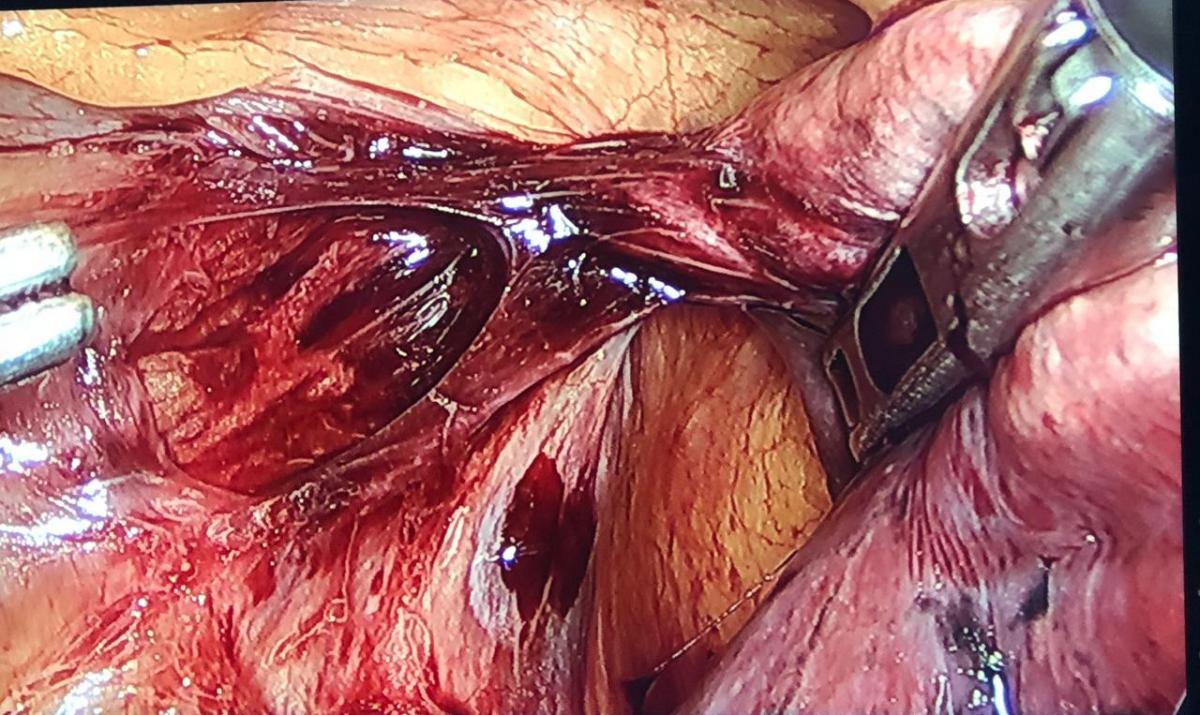
Figure 5. Left upper lobe dissected free from the mediastinal pleura, with care to preserve the left phrenic nerve. The part of the lung still adherent to the mediastinum corresponds to the K-wire penetrating the lung.
Zhang and colleagues (3) reported an interesting case of migration of a K-wire not bent over at the distal end, used to fix a right third rib fracture, into the right ventricle. The patient was asymptomatic and the diagnosis was made during a routine examination. There was no pain or other symptoms or signs, and the echocardiogram did not show pericardial effusion, although it did display the K-wire inside the right ventricle. The foreign body was removed through a median sternotomy on cardiopulmonary bypass. As in this report (3), the authors’ patient was asymptomatic and the diagnosis of the migrating K-wire was incidental. There was no chest pain, cough, or hemoptysis.

Figure 6. K-wire completely dissected from the lung. One can observe the phrenic nerve very close to the K-wire.
Zhang and colleagues mentioned that the most common primary site of fixation from where the migration occurred into the heart was the sternoclavicular joint followed in order by the clavicle, the acromioclavicular joint, and the proximal humerus (3). Intracardiac migration has also been reported from the pelvic bone, the femur, and the finger (3). In the latter scenarios, peripheral intravascular embolization to the heart may be the explanation (4).

Figure 7. With the aid of an energy device, the authors dissected the tissues around the foreign body, in front of the phrenic nerve like in a thymectomy, and the K-wire was easily removed. It was not hooked to the left brachiocephalic vein.
The surgical approach to removing the foreign body depends on its anatomic location. Sternotomy, thoracotomy, or preferably thoracoscopy have been successfully used (4). Martins and colleagues (5) reported a 50-year-old woman who had a left humerus fracture fixed with K-wires. Sixteen years later, a chest CT demonstrated that one of the wires had migrated to the left lung. The K-wire was successfully removed by a VATS approach.

Figure 8. Extracted K-wire with its distal end bent over to avoid migration measuring approximately 5 cm.
In the case discussed here, a left VATS approach with a single lumen endotracheal tube and CO2 insufflation was used. The surgical team was prepared for a sternotomy if necessary. Another surgical strategy discussed was to remove the K-wire through a cervicotomy like in a transcervical thymectomy, using the Cooper’s sternal retractor and simultaneous videothoracoscopic control, which would allow the authors a good visualization of the brachiocephalic trunk and innominate vein, since encroaching on these vascular structures was a concern. In addition, through the cervicotomy, a partial sternotomy could be easily performed if necessary. The final decision was to start with videothoracoscopy with sternotomy capability arranged.
It is important to emphasize that patients who have such orthopedic pins and wires must be followed up with chest radiographs as long as they have these devices in place. They must be removed as soon as any dislocation is detected or when the treatment of the fracture is concluded.
References
- Sharma R, Tam RK. Migrating foreign body in mediastinum – intravascular Steinman pin. Interact Cardiovasc Thorac Surg. 2011;12(5): 883-884.
- Marchi E, Reis MP, Carvalho MV. Transmediastinal migration of Kirschner wire. Interact Cardiovasc Thorac Surg. 2008;7(5):869-870.
- Zhang W, Song F, Yang Y, Tang J. Asymptomatic intracardiac migration of a Kirschner wire from the right rib. Interact Cardiovasc Thorac Surg. 2014;18(4):525-526.
- Reghine ÉL, Cirino CCI, Neto AA, Varallo FR, Évora PRB, de Nadai TR. Clavicle Kirschner wire migration into the left lung: a case report. Am J Case Rep. 2018;19:325-328.
- Martins D, Miranda J, Guerra M. Thoracoscopic removal of an intrathoracic Kirschner wire. Case report. Rev Port Cir Cardiotorac Vasc. 2013;20(2):83-85.



