ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Video Assisted Thoracoscopic Surgery (VATS) Excision of Midthoracic Esophageal Diverticula
Patient Selection
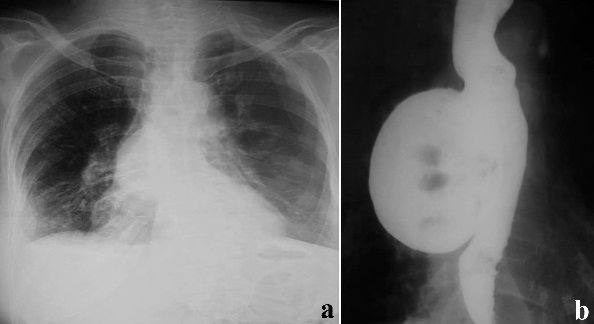
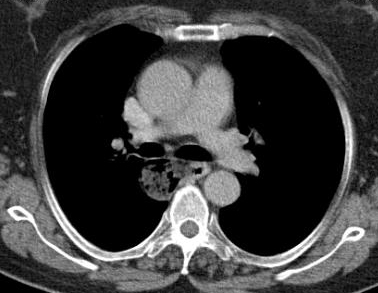
Esophageal diverticula are acquired conditions almost always occurring in adults where the epithelium-lined blind pouch arises from the esophagus. They are categorized primarily by anatomic location and etiology into pulsion and traction diverticula. Zenker and epiphrenic diverticula are false diverticula, while midthoracic diverticula are usually traction diverticula that occur secondary to mediastinal inflammation and fibrosis in adjacent lymph nodes and are true diverticula [1, 2]. Traction type is more common in developing countries [3]. Most esophageal diverticula are found incidentally. The diagnosis is usually made on barium swallow (Figures 1a, 1b). Esophageal endoscopy by an experienced endoscopist is recommended to exclude other etiologies for dysphagia. Chest CT is helpful in the differential diagnosis and identifying the extent of the diverticula (Figure 2). Esophageal manometry typically shows motility disorder, however it is very difficult to advance the pressure probe through the esophagus. Indications for surgery are large sized (>4-5 cm), moderate to severe esophageal symptoms and complicated diverticula [3, 4]. Our patient selection for VATS approach was large midthoracic diverticula and severe esophageal symptoms.


- Figure 1a. A large midthoracic diverticulum in a 60 yr female with history of rheumatoid arthritis. The diverticulum is visible in chest X-ray.
- Figure 1b. 7-8 cm mid thoracic diverticulum with significant retention of contrast material inside the diverticulum, a sign of improper drainage. This patient had difficulty in controlling her rheumatoid symptoms and hypertension despite strict medical compliance due to retention of medications within the diverticulum.
- Figure 2. CT scan of a patient with midthoracic diverticulum. The diverticulum fails to drain properly and has food particles in it.
Indications
- Diverticula larger than 4-5 cm with drainage problems.
- Complaints of dysphagia and regurgitation.
Relative Contraindications for VATS management of diverticula
- Heavily calcified mediastinal lymph nodes and diffuse pleural adhesions.
Operative Steps
Traditionally, thoracotomy was the preferred approach for surgical therapy of midthoracic diverticula. Recently, minimally invasive therapies have been described with success including VATS approach in the prone position [2, 3, 4].
VATS approach has been our preference for the treatment of midthoracic diverticula. We describe our procedure as follows:
The patient is positioned on the operating table initially in the supine position. Under general anesthesia and single lumen intubation, bronchoscopy is performed to access the airway. The entire esophagus is visualized under a rigid esophagoscopy (or flexible) where the food materials and remnants in the diverticula are aspirated. The wide view of the rigid esophagus makes it more advantageous in aspirating the contents of the diverticula than with the flexible endoscope. A guide wire is inserted into the stomach under the fluoroscope and direct view through the esophagoscope, making sure the guide is correctly in place. The esophagoscope is removed leaving the guide wire in place and the patient is re-intubated with a double lumen endotracheal tube. Some authors have stated that in prone position, it is not essential for selective lung ventilation, as creating a pneumothorax with CO2 insufflated to a pressure of 6 to 8mm Hg provided sufficient view and exposure [3]. We perform the procedure in lateral decubitus position, thus double lumen intubation is more favorable.
The patient is then positioned in the left lateral decubitus position. Single lung ventilation is established and the camera port is placed at the sixth or seventh interspace in the anterior axillary line. The thoracic cavity is explored. The second incision is placed at the fourth interspace in the anterior axillary line. Adhesions can be dissected with peanut dissectors, electrocautery, scissors, bipolar thermal sealers or ultrasonic shears. The esophagus, paravertebral sulcus and the azygos vein is visualized at this stage. The third incision is then placed at the fifth interspace posterior to the tip of the scapula and a fourth incision at the eighth interspace in the posterior axillary line (Figure 3).

The mediastinal pleura over the esophagus is divided longitudinally over the esophagus allowing the esophagus to be gently mobilized. The pulmonary ligament is divided with bipolar sealers, electrocautery or ultrasonic shears. The diverticulum is easily visualized at this stage (Video 1). Careful dissection at the subcarinal region is required because of frequent antrachotic and scarred lymph nodes adherent to the bronchus, esophageal wall and diverticulum. The diverticulum is most often noticed between the subcarinal region and the inferior pulmonary ligament. The diverticulum and its base are carefully dissected from the adjacent esophagus (Video 2). Both vagus nerves are clearly identified and preserved during this maneuver.
Video 1
Video 2
Once the diverticulum base is defined, a bougie (usually 50-54 Fr) is introduced across the gastroesophageal junction over the guide wire that was inserted initially under the fluoroscope. As the bougie is advanced in the esophagus the surgeon closely monitors the safe passage of the bougie as well.
The diverticulum is then stapled at its base with an Endo GIA (45-60mm) blue load stapler (Video 3). The diverticulectomy is done with the staple line kept parallel to the long axis of the esophagus to avoid tension and decrease the risk of leak. At this stage, a nasogastric tube may be advanced to the stomach under direct vision. We then close the muscle layer over the staple line with interrupted 4–0 silk sutures.
Video 3
An electrocautery hook is used to perform a long extramucosal esophagomyotomy. We prefer performing a long esophagomyotomy (5cm inferior and 3-4 cm superior to the diverticulum) on the opposite side of the diverticula regardless of the etiology. The myotomy will prevent suture-line leak at the diverticulectomy site by relieving distal obstruction, in addition to decreasing diverticular recurrence and relieve symptoms of the underlying motility condition.
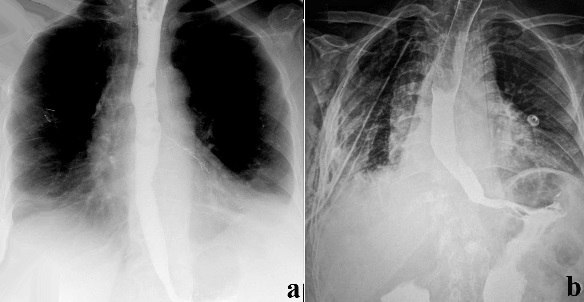
Some authors advocate only diverticulectomy in midthoracic diverticula. Even with myotomy the leak rate and recurrence is high and hence adequate myotomy should be done. There is considerable debate over the addition of an antireflux procedure after the completion of the myotomy [3, 4, 5]. We do not perform fundoplication during the VATS procedure. Once hemostasis is achieved, a single pleural drain is left into the chest cavity along the side of the esophagus and the incisions closed in layers. Patients are not allowed to take oral feeding usually for 3 - 4 days after which a clear liquid diet is initiated. A control barium swallow is recommended (Figures 4a, 4b). The pleural tube is removed postoperatively if the drainage is less than 200cc per day.
Patients are discharged on a semi-solid diet and are advanced to solid diet after 2 weeks.

- Figure 4a. Postoperative barium swallow. These patients have motility problems and the thin line of barium in the left main bronchus is a result of microaspiration and not leakage.
- Figure 4b. The patient with tuberculosis needed bronchoscopic clearance of secretions due to atelectasis. A barium swallow was performed to rule out any leak.
Preference Card
- Double lumen endotracheal tube
- Endo GIA (45-60 mm) blue load stapler
- Bougie (50-54 Fr)
- Rigid esophagoscope
- Ultrasonic shears or bipolar thermal sealers
- Electrocautery hook
- Thoracoscopic needle holders
Tips & Pitfalls
- Initial rigid esophagoscopy to aspirate food particles and remnants and thus clean the mucosa of the esophagus for better mucosal approximation.
- Right lateral decubitus position.Precise placement of the port incisions.
- Extra port incisions may be necessary.
- CO2 insufflation assist in better exposure when deflation of ipsilateral lung not sufficient.
- Mobilization of the entire diverticula.
- Carefully dissect the neck of the diverticulum down to esophagus.
- Delicately dissect the esophagus from the subcarinal region to the inferior pulmonary ligament, avoiding injury to the vessels and the bronchus due to the inflamed esophagus and lymph nodes.
- 54Fr bougie should be passed just before the division of the stalk of the diverticula. If the bougie is held in place for a long time together with a double-lumen endotracheal tube, it might exert too much pressure on the tongue and uvula.
- Place the diverticulectomy staple line along the long axis of the esophagus and not perpendicular, which can increase the risk of esophageal leak.
- Suspicion of mucosal damage should be checked instantly with air insufflation through the nasogastric catheter.
- Long (8-10 cm) esophagomyotomy.
- Postoperative aspiration is common due to the presence of esophageal motility disorder.
Results
The optimal treatment of diverticula remains controversial. In the past, operative treatment was favored for symptomatic patients only, although some authors have advocated operative intervention in all patients with thoracic diverticula regardless of symptoms. Surgical treatment should be reserved for large diverticula and symptomatic patients because of the high morbidity and mortality risk rate associated with surgery (Table 1) [4]. Little has been reported of midthoracic diverticula. The largest series of minimal invasive approach for esophageal diverticula was reported by Hiran and colleagues. In their report there were 4 patients with midthoracic diverticula operated by video assisted thoracoscopic surgery (VATS) and 2 had leakage. The most common procedure they used was diverticulectomy and esophagomyotomy with laparoscopy, VATS or a combination of both. Their complication rate was 45%, with a 20% leak rate and a mortality of 5%. Similar results have been reported by previous authors [4, 5, 7]. Poor surgical results are often attributed to inadequate myotomy [6]. So far we have performed 3 cases of midthoracic diverticula with no leaks. Two of the patients had prior history of tuberculosis and one had rheumatoid arthritis. Patients with tuberculosis had postoperative atelectasis necessitating flexible bronchoscopy (Figure 4b). All of the patients were discharged within 10 days with no recurrence of symptoms reported at 2 years follow-up. Midthoracic diverticula are rare clinical conditions which can be managed safely with VATS, however proper techniques should be utilized to prevent complications.
Table
Table 1. Results of thoracoscopic surgery in esophageal diverticula.
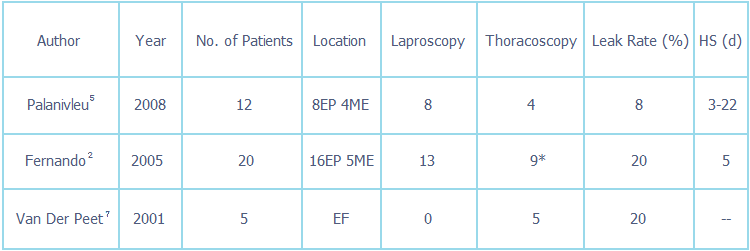
HS, hospital stay; EF, epiphrenic; ME, midesophageal; d, days.
* In 2 of the patients laparoscopy and thoracoscopy was simultaneously used.

.
References
- Cassivi SD, Nichols FC and Deschamps C. Esophageal diverticula. In: Shields TW, LoCicero J, Reed CE, Feins RH, ed. General Thoracic Surgery, seventh edition. Lippincott Williams & Wilkins, 2009:1961-1971.
- Sohn HJ, DeMeester SR. Resection of Esophageal Diverticula. Sugarbaker DJ, Bueno R, Krasna MJ, Mentzer SJ, Zellos L: Adult Chest Surgery. 2009:231-8.
- Palanivelu C, Rangarajan M, Maheshkumaar GS, Senthilkumar R. Minimally invasive surgery combined with peroperative endoscopy for symptomatic middle and lower esophageal diverticula: a single institute's experience. Surg Laparosc Endosc Percutan Tech. 2008Apr;18(2):133-8.
- Fernando HC, Luketich JD, Samphire J, Alvelo-Rivera M, Christie NA, Buenaventura PO, Landreneau RJ. Minimally Invasive Operation for Esophageal Diverticula. Ann Thor Surg 2005;80:2076-81.
- Benacci JC, Deschamps C, Trastek VF, Allen MS, Daly RC, Pairolero PC. Epiphrenic diverticulum: Results of surgical treatment. Ann Thorac Surg 1993;55:1109-14.
- Deb SJ, Dechamps C. Surgical Management Of Epiphrenic Diverticula. 2007. http://www.ctsnet.org/sections/clinicalresources/thoracic/expert_tech-36.
- Van der Peet DL, Klinkenberg-Knol EC, Berends FJ, Cuesta MA. Epiphrenic diverticula: minimal invasive approach and repair in five patients. Dis Esophagus 2001;14(1):60-2.