ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
"Sutureless" Pulmonary Vein Stenosis Repair
Patient Selection
The “sutureless” neoatrium technique was initially described for anastomotic stenosis occurring after repair of total anomalous pulmonary venous connection (post-repair pulmonary vein stenosis, PRPVS). The procedure is also helpful in patients with congenital pulmonary vein stenosis and has been used in selected patients on the initial presentation of total anomalous pulmonary venous connection. Most of these patients will have a preoperative evaluation with transthoracic echocardiography, cardiac catheterization (to assess pulmonary artery pressure), and magnetic resonance imaging, if available.
Operative Steps
After initiation of standard cardiopulmonary bypass with bicaval cannulation and antegrade cold blood cardioplegia, hypothermic blood cardioplegic arrest is induced. Alternatively, uniatrial venous cannulation and deep hypothermic circulatory arrest strategies can be employed.
For patients with PRPVS, the initial approach is through the right atrium and across the atrial septum to allow visualization of the pulmonary vein ostia and clear definition of the location and extent of stenosis. Often the stenosis is localized to the anastomotic region, but occasionally it may extend diffusely through the pulmonary veins in a retrograde direction.
For patients in whom this technique is to be used at the initial presentation of total anomalous pulmonary venous connection (as pictured below), the initial approach is through the left atrium after retraction of the heart to the right. The incision in the left atrium is extended transversely across the back of the left atrium to the edge of the interatrial septum. The pulmonary vein confluence is then incised transversely across its entire length. The incision can be carried into each pulmonary vein out to the second order branches if necessary. Placement of a blade of a Potts scissors in the lumen with the other blade out of the lumen and cutting distally into the lung facilitates this maneuver. The incision should be carried as far into the lung as necessary to get beyond any stenotic regions. Care must be taken to leave the adventitia intact when pulmonary vein incisions are made because the adventitia will contain the pulmonary venous effluent in a “controlled bleed” into the left atrium.
The divided edge of the atrial wall is then sutured to the pericardium (not the pulmonary vein) in a suture line remote from the divided edge of the pulmonary veins using a running fine absorbable suture. This suture line contains the pulmonary venous effluent in a “controlled bleed” while avoiding any direct suturing of the pulmonary veins. The suture line is relatively easy to sew because it connects the left atrial edge to the pericardium in a circle around the pulmonary veins. Consequently, the suture line ignores the complex shapes of the pulmonary vein incisions and simply maintains hemostasis by direct anastomosis of the left atrium to the pericardium.
In cases of isolated left or right pulmonary vein stenosis, the technique can be used in a unilateral fashion. The divided edge of the left atrium is then sewn to the pericardial reflection over the incised pulmonary veins. This suture line is then routed inwards to the confluence of the pulmonary veins to complete hemostasis in the central portion of the anastomosis.
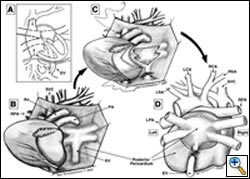 |
| Schematic Illustration of Type III TAPVC |
- Schematic illustration of Type III TAPVC – all four pulmonary veins connect to a common pulmonary vein that drains into a vertical vein that penetrates the diaphragm and empties into the inferior vena cava.
- The apex of the heart has been tilted to the right, exposing the left atrium and the TAPVC.
- The vertical vein has been tied off and the common pulmonary vein opened with incisions carried into all four pulmonary veins. The left atrium was been incised. The “sutureless” repair has been started by suturing the left atrium to the adventitia of the pericardium adjacent to the pulmonary veins, staying away from the actual edge of the pulmonary veins.
- Posterior view of the completed anastomosis with the vertical vein divided and the suturing of the left atrium to the pericardium completed.
Preference Card
Equipment/Instruments
- “Drop-in” suction cannula
- Fine Castro Potts scissors
- Dilators to check pulmonary vein size
- Transesophageal echocardiography
Suture
- Fine absorbable suture e.g., 5-0 or 6-0 PDS (Ethicon, Somerville, NJ)
- Alternatively, 7-0 Prolene (Ethicon, Somerville, NJ)
Tips & Pitfalls
- The use of “drop-in” suction cannula facilitates visualization of the pulmonary veins.
- Circulatory arrest is typically unnecessary, but hypothermia is helpful to allow temporary reduction in perfusion rates to assist with visualization of the pulmonary veins.
- Suturing of the atrium to the pericardium over the pulmonary veins puts the phrenic nerve at risk. Sutures should be superficial in this area.
- Remember that the anastomosis will contain a very low pressure chamber and, therefore, the strength of the sutures will be far less important than obtaining hemostasis through meticulous attention to detail.
- Bleeding after completion of the anastomosis can be visualized after weaning from cardiopulmonary bypass (to fill the neo-left atrium). Aggressive incision of the pulmonary veins can lead to violation of the pleural cavity in the hilar region, leading to uncontrolled hemorrhage into the pleural cavity (n=4). A technique of intrapleural hilar reapproximation was developed. Using this technique, the pericardium is incised at the level of the diaphragm posteriorly to the level of the phrenic nerve. The pericardium is then retracted to the midline to expose the anterior hilum. The defect in the pleura is then reapproximated with a fine running suture with care taken to avoid injury to the phrenic nerve.
- Access to the inferior and lateral suture line can be obtained by gently tipping the heart upwards using techniques commonly employed in off-pump myocardial revascularization.
- Access to the superior portion of the suture line can be obtained through the transverse sinus via the space between the aorta and superior vena cava.
- Division of inferior vena cave: We liberally use division of the inferior vena cava to improve surgical exposure (n=12). This leaves the heart tethered by the aorta and pulmonary artery. Consequently, retraction of the heart out of the mediastinum is possible, providing ample exposure as the anastomosis is constructed.
Results
At the Hospital for Sick Children in Toronto, this technique was originally described for two patients with bilateral pulmonary vein stenosis following TAPVC repair. Both were surviving at 1.8 years postoperatively [3]. In the Discussion of that paper, at least seven other successful cases were noted. Lacour-Gayet later reported success in five of seven patients (all reoperations). Several other centers have now reported success with this technique. Updated results with the sutureless technique in nearly 40 patients operated on at the Hospital for Sick Children were presented at the 2004 Annual Meeting of The American Association for Thoracic Surgery held in Toronto. Ten patients had PRPVS and 26 patients had no prior operation but were at high risk of stenosis. As compared to conventional management, the sutureless technique was associated with decreased risk of reoperation or death (mean follow-up 3 years) [7].
References
- Lacour-Gayet F, Rey C, Planche C. [Pulmonary vein stenosis. Description of a sutureless surgical procedure using the pericardium in situ]. Arch Mal Coeur Vaiss, 1996;89:633-636.
- Najm HK, Caldarone CA, Smallhorn J, Coles JG. A sutureless technique for the relief of pulmonary vein stenosis with the use of in situ pericardium. J Thorac Cardiovasc Surg, 1998;115:468-470.
- Caldarone CA, Najm HK, Kadletz M, Smallhorn JF, Freedom RM, Williams WG, Coles JG. Relentless pulmonary vein stenosis after repair of total anomalous pulmonary venous drainage. Ann Thorac Surg, 1998;66:1514-1520.
- Lacour-Gayet F, Zoghbi J, Serraf AE, Belli E, Piot D, Rey C, Marcon F, Bruniaux J, Planche C. Surgical management of progressive pulmonary venous obstruction after repair of total anomalous pulmonary venous connection. J Thorac Cardiovasc Surg, 1999;117:679-687.
- Spray TL, Bridges ND. Surgical management of congenital and acquired pulmonary vein stenosis. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu, 1999;2:177-188.
- Ricci M, Elliott M, Cohen GA, Catalan G, Stark J, de Leval MR, Tsang VT. Management of pulmonary venous obstruction after correction of TAPVC: risk factors for adverse outcome. Eur J Cardiothorac Surg, 2003;24:28-36.
- Yun T-J, Coles JG, Rachel WM, et al. The sutureless technique for repair of pulmonary veins: extension from post-repair pulmonary vein stenosis to primary repair of pulmonary venous anomalies. Presented, 84th Annual Meeting, The American Association for Thoracic Surgery, Toronto, Ontario, April 25-28, 2004.



