ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Giant Bullous Emphysema
Patient Selection
Bullous emphysema is histologically referred to as the presence of emphysematous areas
with a complete destruction of lung tissue producing an airspace greater than 1 cm in diameter. Bullae must be clearly differentiated from other disorders as lung cysts (developmental anomalies; they are lined by respiratory epithelium) and blebs (small sub pleural collections of air). Most of the outer surface of bullae is made of visceral pleura while the inner layer consists of fibrous tissue formed mainly by the destroyed adjacent lung.
The classification of bullae is useful to evaluate patients as candidates for surgery and to predict the potential functional outcome1,2. One classification scheme is based on the anatomy of the bullae and the quality of the underlying lung:
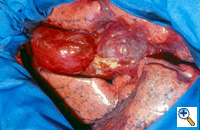
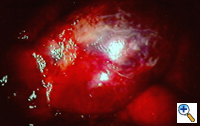
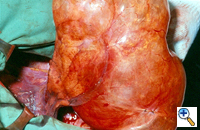
Group I: Single large bulla with normal underlying lung (Figure 1)
Group II: Multiple bullae with underlying normal lung
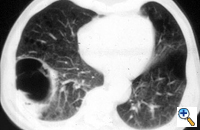
Group III: multiple bullae with underlying lung diffusely emphysematous (Figure 2)
Group IV: Multiple bullae with underlying lung affected by other diseases
 |
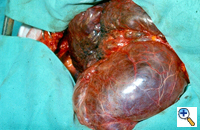 |
| Figure 1: Operative view at thoracotomy of a single bulla with normal underlying lung. | Figure 2: Operative view at thoracotomy of multiple bullae with underlying lung with diffuse emphysema. |
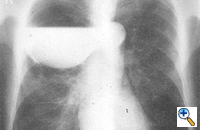 |
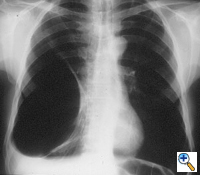
| Figure 3: Chest x-ray of a large bulla with true infection; after the appropriate medical treatment fever, hemptysis and fluid level persisted and the bulla was resected. |
Patients in Group I and II are ideal candidates for surgery with predictably good results. Patients in Group III and IV must be carefully selected; functional results and clinical outcome are less predictable, since the quality and functional impairment of the underlying lung is more difficult to evaluate. Bullous disease may also be associated with a complete destruction of the underlying lung and irreversible respiratory failure; in these cases only lung transplantation can be considered if the selection criteria for this procedure are respected.
Surgery is generally indicated to modify the functional status of the underlying lung by (1) relieving restrictive changes; (2) increasing compliance and airway caliber; (3) improving V/Q ratio; and (4) decreasing the physiologic dead space. These goals are easy to obtain in patients with enlarging bullae and minimal underlying lung disease. These are the best candidates for surgery and optimal results can be expected. Surgery is also indicated to treat complications related to the bullae, such as pneumothorax, true infection (Figure 3), hemoptysis, cancer (Figures 4, 5), and pain.
"Preventive surgery" has been advocated when bullous disease may cause pneumothorax in patients with high risk occupation, independent of the diameter of the bulla and the state of the underlying lung. The choice of surgery is less unequivocal in asymptomatic patients with one or more bullae of moderate size since their natural history is poorly documented. However, a bulla increasing in size on serial chest x-rays as well as lesions occupying more that one third of the hemithorax should be resected even if the patient is asymptomatic.
A second major challenge is represented by dyspneic patients with bullae and diffuse emphysema. In this setting it is of paramount importance to evaluate the actual role of the bulla and the function of the underlying non-bullous emphysematous lung. Selection for surgery in this group of patients is extremely difficult. If bullectomy is considered it should be interpreted as a lung volume reduction procedure and improvement is mainly due to modifications of pulmonary mechanics3.
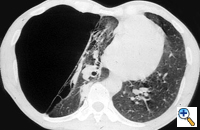
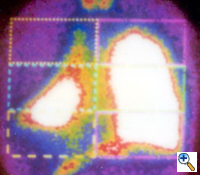
The preoperative work-up should always include clinical and functional evaluation (arterial blood gas analysis and pulmonary function tests with plethysmography), chest x-ray (Figure 6), computed tomography (Figure 7), and V/Q scan (Figure 8). Pulmonary angiography (Figure 9) has been reported to show some advantages in evaluating the underlying lung; however, it is not routinely performed.
Results can be predicted on the base of the clinical presentation, PFTs, and imaging. Better results are anticipated for: (1) younger patients with no comorbidity, no weight loss and rapidly progressing dyspnea; (2) normal or slightly decreased FVC; (3) FEV1 > 40% predicted; and (4) normal DLCO and arterial blood gas analysis. Improved results are also expected when radiologic work up shows large and well localized bullae with evidence of vascular crowding and normal pulmonary density and architecture around the bulla. Angiography and isotope scan should show preserved distal vascular branching and a well localized matching defect with normal uptake and washout from the underlying lung.
Operative Steps
Surgical treatment of bullous emphysema is technically not difficult when the correct indications, technique and postoperative management are respected. However, it can lead to serious complications when performed inappropriately.
Surgical bullectomy is usually performed with videothoracoscopic techniques 4. This approach is ideal both for unilateral and bilateral bullectomy. When a bilateral approach is required, median sternotomy and simultaneous bilateral anterior thoracotomy also could be considered5. In this latter group of patients staged procedures also could be performed. Video assisted thoracoscopy can be immediately converted to open thoracotomy when intraoperative findings require it.
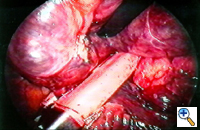
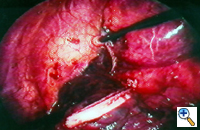
VATS bullectomy is performed under general anesthesia with double lumen endotracheal intubation. After discontinuing ventilation to the operated side, the first incision is usually made at the level of the 6th or 7th intercostal space in the midaxillary line. Careful inspection of the bulla and underlying lung parenchyma may be difficult since large bullae are usually under tension and obliterate the pleural space. The other two incisions are performed to achieve a "triangulation approach" and are used to place graspers and staplers. Pleural adhesions are coagulated and divided to completely mobilize the lung and bulla/bullae. The use of a thoracoscope with a working channel may further help to have an additional port available for instruments. The bulla can be incised and deflated to facilitate gentle manipulation of the lung; it is usually squeezed and twisted ("spaghetti procedure") to identify the base. Traction on the surrounding parenchyma must be carefully performed to avoid injuring the lung surface with consequent prolonged air leaks during the postoperative period. Pedunculated bullae are easily excised with endostapling devices. Broad-based bullae can be removed with multiple applications of endoscopic staplers (Figures 10-12). The bulla is usually excised with a rim of "normal" lung parenchyma to avoid leaving open bronchioles. When removing bullae with underlying emphysematous lung, the stapler line is usually reinforced with commercially available strips6. Additional small bullae and blebs in the residual lung are either excised or coagulated.
At the end of the procedure particular attention is paid to the presence of air leaks. If they are observed, surgical sealants may be applied to cover the holes and reduce or eliminate this complication. Gentle re-expansion of the residual lung is achieved to check how it fills the pleural cavity. If a residual space is anticipated, a pleural tent can be designed thoracoscopically to reduce it7. The pleural cavity is usually drained with two multifenestrated chest tubes in the costovertebral groove and behind the anterior chest wall. Postoperative pain control is usually obtained with intravenous continuous analgesia; epidural analgesia can be considered for bilateral bullectomy.
Other techniques have been described to treat bullous emphysema. Instead of resecting the bulla, it can be rolled or folded and plicated over itself placing a stapler at the base. This technique is better performed through an open approach and has the potential advantage of allowing reinforcement of the staple line with the bulla itself. However, our feeling is that bullae should always be completely resected since the risk of cancer is 36 times higher than in the normal lung parenchyma8. We routinely send the bulla for histology and random routine sampling has demonstrated the potential development of cancer9.
In a selected group of patients a modification of the Monaldi procedure has been proposed by Goldstraw10. CT scanning is used to select the optimal site for surgical incision. A portion of the underlying rib is resected and the pleura is opened to reveal the lateral wall of the dominant bulla. Two concentric purse-string sutures are placed and the bulla is incised. Talc is insufflated to elicit a fibrous reaction and promote a rapid and permanent contraction of the cavity. A 32 Foley catheter is inserted into the cavity and led out thorough the incision. The balloon of the catheter is inflated with 30 - 40 ml of air and the pursue-string sutures are tied around it. Suction is applied to the catheter with the resultant collapse of the bulla. Talc is insufflated around the free pleural space to induce pleurodesis and an intrapleural drainage catheter is placed thorough a basal stab incision. The wound is closed around the Foley catheter, which is secured under traction, apposing the wall of the bulla to the chest wall. The pleural drainage catheter is usually removed within 48 hours and the Foley catheter within 8 days.
Preference Card
- Standard thoracoscopy setup
- Multiple staplers
- Thoracoscopic instruments
- Reinforcement strips (bovine pericardium or PTFE)
- Synthetic sealants
Tips & Pitfalls
- Bullectomy should be performed only when positive results can be reasonably predicted or when complications require it.
- Maximize medical therapy and respiratory physiotherapy before surgery.
- Manipulate the underlying lung carefully. Damage to the surface should be avoided. Completely mobilize the bullae and lung.
- The staple line should be placed on the underlying lung to give more consistency to the resection line.
- In case more than one stapler shot is required to resect the bulla, we recommend careful apposition in sequence to avoid air leaks between the staple lines.
- Avoid excessive upward traction on the bulla during stapler placement to prevent parenchymal damage between two staple lines.
- Check for complete re-expansion of the residual lung. Pleural tent may be useful to reduce postoperative spaces.
- Carefully position the two chest tubes.
- Use moderate or no pleurevac suction in the postoperative course.
- Postoperative air leaks should be managed conservatively: almost all will usually stop. We encourage the use of the Heimlich valve.
- Residual spaces should be carefully drained, even with placement of additional chest tubes.
- Pneumoperitoneum could help to obliterate residual spaces during the postoperative course.
- Employ early mobilization of the patient and vigorous physiotherapy immediately after the operation.
Results
Operative mortality for bullous emphysema in patients with compression of relatively normal underlying lung has been low, ranging from 0% to 8%. Morbidity is primarily related to prolonged air leaks and pulmonary infections.
Early results in carefully selected patients have been excellent, with improvement in symptoms occurring within a few weeks of surgery and sustained for a period of years. The best results are seen in patients with large bullae causing the greatest compression of almost normal underlying lung. Symptomatic improvement, including a reduction of dyspnoea, is usually observed, which reflects both the lessening of breathing efforts and improvement of diaphragmatic motion. However, clinical and symptomatic improvement is sometimes greater than actual spirometric measurements.
Results in patients with bullae and severe underlying emphysema are more difficult to predict and assess. It has been claimed by some authors that bullectomy is not worthwhile in this subset of patients and is associated with a higher morbidity and mortality with a long-term follow-up revealing a more rapid deterioration than in patients with localized disease. The functional decline seems to be similar to that recorded after lung volume reduction surgery in non-bullous emphysema. We postulate that in this subset of patients the effect of bullectomy is related to the reduction of thoracic volumes and the restoration of physiologic diaphragmatic and chest wall mechanics more than to lung re-expansion and recruitment of more functional lung parenchyma. This confirms the impression of other authors who describe bullectomy in patients with severe emphysema as "a special case of lung volume reduction." In fact, in this subset of patients, bullae can be interpreted as a sign of heterogeneous emphysema, that is usually associated to the most favorable clinical outcome after lung volume reduction.
The video-assisted thoracoscopic approach for treatment of giant bullous emphysema is safe and effective. Careful selection of patients is mandatory, as well as a correct intraoperative and postoperative management. Morbidity and mortality are usually low and objective functional improvement can be obtained with the correct indications.
References
- Shamji FM. Classification of cystic and bullous lung disease. Chest Surg Clin N Am 1995;5:701-16.
- Mehran RJ, Deslauriers J. Indications for surgery and patient work up for bullectomy. Chest Surg Clin N Am 1995;5:717-34.
- Snider GL. Reduction pneumoplasty for giant bullous emphysema. Chest 1996:109:540-8.
- De Giacomo T, Venuta F, Rendina EA, et al. Video-assisted thoracoscopic treatment of giant bullae associated with emphysema. Eur J Cardio-Thorac Surg 1999;15:753-7.
- Lima O, Ramos L, Di Biasi PD, et al. Median sternotomy for bilateral resection of emphysematous bullae. J Thorac Cardiovasc Surg 1981;82:892-7.
- Cooper JD. Technique to reduce air leaks after resection of emphysematous lung. Ann Thorac Surg 1994;57:1038-9.
- Venuta F, De Giacomo T, Rendina EA, et al. Thoracoscopic pleural tent. Ann Thorac Surg 1998; 66:1833-4.
- Stoloff IL, Kanofsky P, Magilner L. The risk of lung cancer in males with bullous disease of the lung. Arch Environ Health 1971; 22:163-7.
- Venuta F, Rendina EA, Pescarmona E, et al. Occult lung cancer in patients with bullous emphysema. Thorax 1997;52:289-90.
- Goldstraw P, Petrou M. The surgical treatment of emphysema. The Brompton approach. Chest Surg Clin N Am 1995; 5:777-96.