Introduction
Chordomas are rare, slow-growing neoplasms derived from notochord remnants which form the early spine in fetal development. Most of the notochord is replaced by spine during the first six months of maturity, but small areas can remain and form chordomas accounting for 1-4% of all skeletal tumors [1]. These occur in the mid-line of the axial skeleton, the majority occurring between the ages of 40-70 years (average 55 yr), with a male to female ratio of 2:1 and occasionally in children. They are most often found arising from the sacrococcygeal area (50%) or base of skull (40%) [2, 3]. We present an unusual case of a metastatic sacrococcygeal chordoma involving the chest wall with discussion of surgical management.
Case Presentation
The patient is a 62 year old male who was initially diagnosed with a sacral chordoma in 2001 and was resected through a posterior sacral midline incision with positive margins followed by radiation to this area with delayed healing of the surgical wound. Two years later, he presented with a new painful mass and tingling and weakness in both lower extremities. Fine needle aspiration was consistent with sacral chordoma and he underwent resection of recurrent chordoma and advancement of local musculofascial and fasciocutaneous flaps for coverage. Six months later a CT scan of the chest demonstrated multiple peripheral pulmonary nodules consistent with metastatic disease.
Subsequently the patient underwent left VATS wedge resection of a lower lobe nodule to confirm the diagnosis of metastatic chordoma. At that time he was referred to medical oncology for consideration of chemotherapy with Gleevec but not considered a candidate as he was asymptomatic.
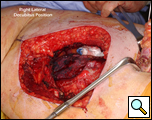
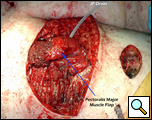
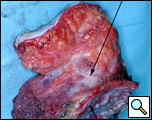
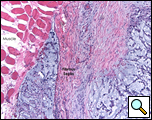
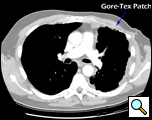
Eleven months later, he presented with a several month history of a painful fixed, firm mass over the pectoral area of the left chest and a smaller mass inferior to this (Figure 1). CT scan demonstrated a new 2 cm nodule in the left upper lobe associated with an anterior chest wall mass six centimeters in size in addition to bilateral new pulmonary nodules (Figure 2). The mass was tethered to the skin and in danger of eroding through it. The patient underwent en-bloc resection of the chest wall and adjacent lung (Figures 3a-c). The resulting defect (Figure 4a) was reconstructed with 2 mm Gore-Tex patch (Figure 4b) and pectoralis major muscle flap (Figure 4c) with primary skin closure (Figure 4d). The pathology revealed metastatic chordoma (Figures 5a-d). The patient recovered well, leaving the hospital on the sixth postoperative day.
Twelve months postoperatively, the patient experienced recurrence of his disease in the chest wall, but has had good palliation from the initial chest wall involvement. He has otherwise felt well and has good use of his left upper extremity (Figure 6a, 6b, 7).
Discussion
Most chordomas are slow-growing lesions, with a tendency to recur locally. This case demonstrates that extensive metastases to the lungs and chest wall may occur. The treatment for the primary tumor is surgical excision with postoperative radiation therapy. However, there is a high incidence of recurrence (25-64%) due to an inability to achieve either an adequate surgical or radiation margin. These tumors can be life-threatening by direct extension or metastasizing to other organs, including the lungs (20-30%) and posterior mediastinum [4, 5]. The five year survival rate for metastatic disease is approximately 50%. Chordomas may also involve the skin (chordoma cutis) by direct extension or distant metastases [3, 6]. However, metastases to the chest wall are extremely rare, there being only one other reported case in the literature [6].
When chordomas present within the mediastinum they should be resected, and whether treatment with adjuvant radiation is helpful is unknown [4]. Pulmonary metastases should be resected if considered technically possible, as this may prolong survival and achieve local control of the disease.
The appropriate treatment for chest wall metastases for chordoma is not known due to the rarity of this occurrence. Indications for chest wall metastasectomy include resection for diagnosis, local control, and palliation / prevention of skin ulceration and rarely for cure or as part of a multidisciplinary approach [7]. While radiation therapy is another option for local control, its ability to prevent progression of disease is unpredictable and unknown in the case of chordoma. Once the area of the chest wall has been irradiated, subsequent resection and reconstruction is more difficult and prone to failure [8, 9]. In the presented case, resection was performed for local control, pain relief and to prevent the complications of ulceration, necrotizing infection and bleeding from a tumor eroding through the anterior chest wall. The principles of chest wall resection were adhered to by performing a full thickness en-bloc resection of the mass, reconstruction with a two mm Gore-Tex patch and coverage with a well-vascularized myocutaneous flap.
As demonstrated by this case surgical therapy offers excellent palliation of symptoms and improves quality of life by preventing local complications.
References
- Baratti D, Gronchi A, Pennacchioli E, et al. Chordoma: natural history and results in 28 patients treated at a single institution. Ann Surg Oncol 2003;10:291-6.
- Selvaraj A, Wood AJ. Superior mediastinal chordoma presenting as a bilobed paravertebral mass. Eur J Cardiothorac Surg 2003;23:248-50.
- Ruiz HA, Goldberg LH, Humphreys TR, Blacklock JB. Cutaneous metastasis of chordoma. Dermatol Surg 2000;26:259-62.
- Rahman AM, Farahat IG, Ali WA, Mansour KA. Giant mediastinal chordoma. Ann Thorac Surg 2002;73:1952-4.
- Suster S, Moran CA. Chordomas of the mediastinum: clinicopathologic, immunohistochemical, and ultrastructural study of six cases presenting as posterior mediastinal masses. Hum Pathol 1995;26:1354-62.
- Jones B, Ghosh BC, Skelton HG. Chordoma with cutaneous metastasis. Cutis 1994;54:250-2.
- Pfannschmidt J, Geisbusch P, Muley T, Hoffmann H, Dienemann H. Surgical resection of secondary chest wall tumors. Thorac Cardiovasc Surg 2005;53:234-9.
- Rouanet P, Jozwik M, Pujol H. Divided latissimus dorsi musculocutaneous flap for chest wall radionecrosis. Ann Plast Surg 1994;33:418-20.
- Rouanet P, Fabre JM, Tica V, Anaf V, Jozwick M, Pujol H. Chest wall reconstruction for radionecrosis after breast carcinoma therapy. Ann Plast Surg 1995;34:465-70.