ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Ectopic Thyroid in the Anterior Mediastinum Resected Through a Video-Assisted Transcervical Approach: Case Report
Boasquevisque CH. Ectopic Thyroid in the Anterior Mediastinum Resected Through a Video-Assisted Transcervical Approach: Case Report. July 2019. doi:10.25373/ctsnet.8326949.
Introduction
The most frequent tumors in the anterior mediastinum are thymomas/thymic lesions (40%), lymphomas (25%), and germ cell tumors (20%). Substernal or retrosternal goiters/ectopic thyroid comprise 15% of anterior mediastinal masses (1).
Ectopic thyroid is a rare entity with an estimated prevalence of 1:100,000-300,000 (2) and 1:4,000-8,000 in patients with thyroid diseases (2). Ectopic thyroid tissue (ETT) can coexist with an orthotopic thyroid, although in the majority of the cases it is the sole existing thyroid tissue (1). Lingual thyroid is the most frequent type, corresponding to 47% to 90% of the reported cases (3, 4). ETT in the mediastinum comprises 1% of all cases (3, 5). In autopsy series, its incidence is reported to be 7% to 10% (5). Thullier and colleagues, in 2012, mentioned that only 7 cases had been described in the literature during the previous 30 years (4).
Surgical approaches used for resection of mediastinal ETT are median sternotomy, posterolateral thoracotomy, video thoracoscopy, robotic surgery, and transcervical and subxiphoid approaches. Localization in the mediastinum and size are important features to decide the surgical approach.
Herein, the authors report a case of an ectopic thyroid in the anterior mediastinum—initially judged to be a small thymoma—that was resected through a video-assisted transcervical approach.
Case Report
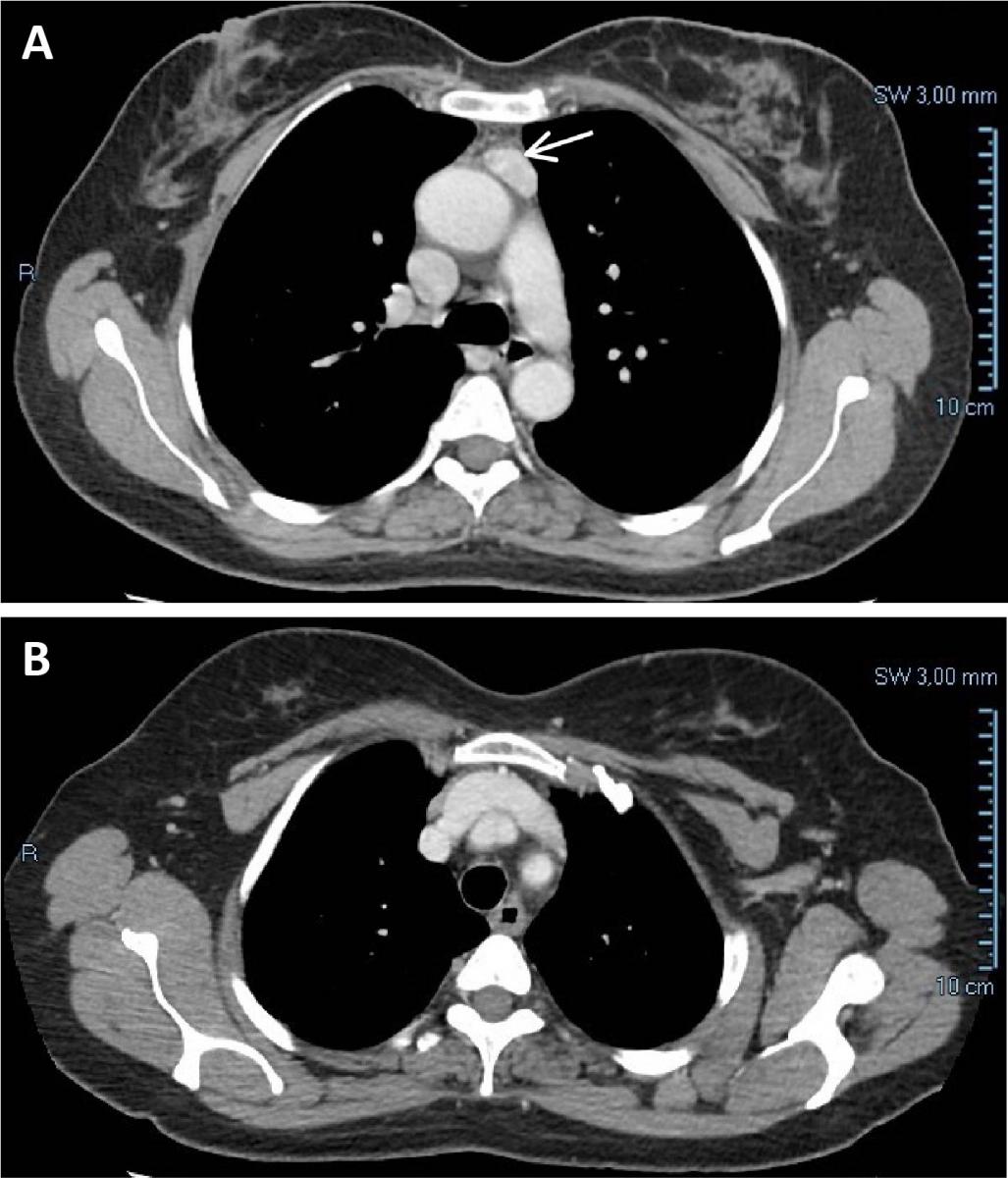
Figure 1. (A) Chest CT showing a tumor measuring 24 x 12 mm in the anterior mediastinum, suggestive of a small thymoma. The tumor showed a high contrast enhancement. There is a clear plane between the mass and the aorta and no compression of any mediastinal structures. (B) No connection with the cervical thyroid was observed. In retrospect, this is one of the features of mediastinal ectopic thyroid.
A 58-year-old woman sought medical treatment because of abdominal pain. Previously, she had been diagnosed with colonic diverticular disease. At the emergency department, an abdominal computed tomography (CT) was performed and no abdominal abnormality was seen. A 6 mm pulmonary nodule was detected in the left inferior lobe and a follow-up chest CT revealed an anterior mediastinum density below the level of the aortic arch, measuring 24 x 12 mm and showing high contrast enhancement (Figure 1). Lymphadenopathy, thymoma, ectopic thyroid, and parathyroid adenoma were the diagnostic hypotheses in the radiology department.
The patient was aware of bearing a nontoxic multinodular goiter and had sought consultation with two head and neck surgeons. Thyroid hormones levels were in the normal range (TSH: 1.29 mcUI/ml, normal range: 0.4-4.3 mcUI/ml; free T4: 1.0 ng/dl, normal range: 0.7-1.9 ng/dl). Thyroid ultrasound with Doppler showed a multinodular goiter with no signs of malignancy. One nodule in the right lobe underwent fine needle aspiration and was benign (Class II, Bethesda). Thyroid surgery was not considered by the two consulting surgeons at that time.
The patient reported muscle weakness, but myasthenia gravis was not present. Anti-acetylcholine receptor antibody detection was negative (0.23 nmmol/L; reference: negative < 0.45 nmol/L, positive > 0.45 nmol/L). Electroneuromyography was also negative for myasthenia gravis. Thyroid scintigraphy was not performed, as the patient had undergone CT scan with iodine contrast and nuclear imaging could not be done for at least four weeks. In addition, the main consideration was a small thymoma, and surgery for diagnosis and treatment had been decided.
Surgery
During surgical evaluation, the patient was judged to be a good candidate for video-assisted transcervical resection of the thymus and tumor.

Figure 2. Patient positioned supine, arms placed at the sides, neck hyperextended. A transverse cervicotomy was performed and superior and inferior subplatysmal flaps were raised.
The patient was intubated with a double-lumen tube, but orotracheal intubation with a single-lumen tube is also feasible to perform this operation in close collaboration with the anesthetist. Two peripheral veins were punctured and a left radial artery catheter installed for monitoring. A roll was placed under the shoulders to aid in hyperextension of the neck, and her arms were placed at her sides.
A transverse cervicotomy was performed 2 cm above the sternal notch from sternocleidomastoid to sternocleidomastoid muscles, and superior and inferior subplatysmal flaps were raised (Figure 2). The neck was dissected through the midline, and the thyrothymic ligaments were ligated with 0-silk ties.
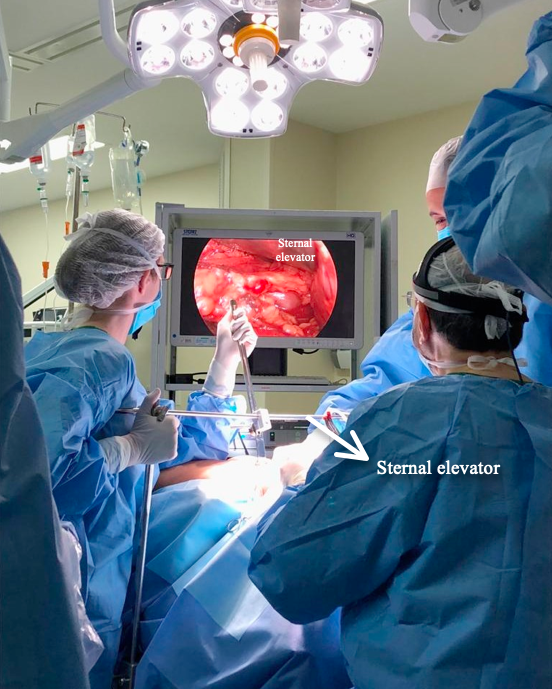
Figure 3. A sternal elevator is used to improve the surgical field at the level of the thoracic inlet. The assistant on the right holds the 30⁰ 10 mm thoracoscope. A 5 mm thoracoscope can also be used.
The cervical thymus was fully dissected and through blunt dissection of the retrosternal space, room was created to insert the sternal elevator, which improves the surgical exposure at the thoracic inlet. Then, the innominate vein was identified, the thymus was dissected free, and the thymic veins were managed with bipolar energy or clips. After dissecting the thymus off of the innominate vein, the thymus and the mediastinal tumor were dissected from the pericardium and both mediastinal pleurae, mostly using bipolar energy under video thoracoscopic control (Figures 3 and 4). A multifenestrated large suction drain was left in the anterior mediastinum entering the left pleural cavity and removed on the first postoperative day.
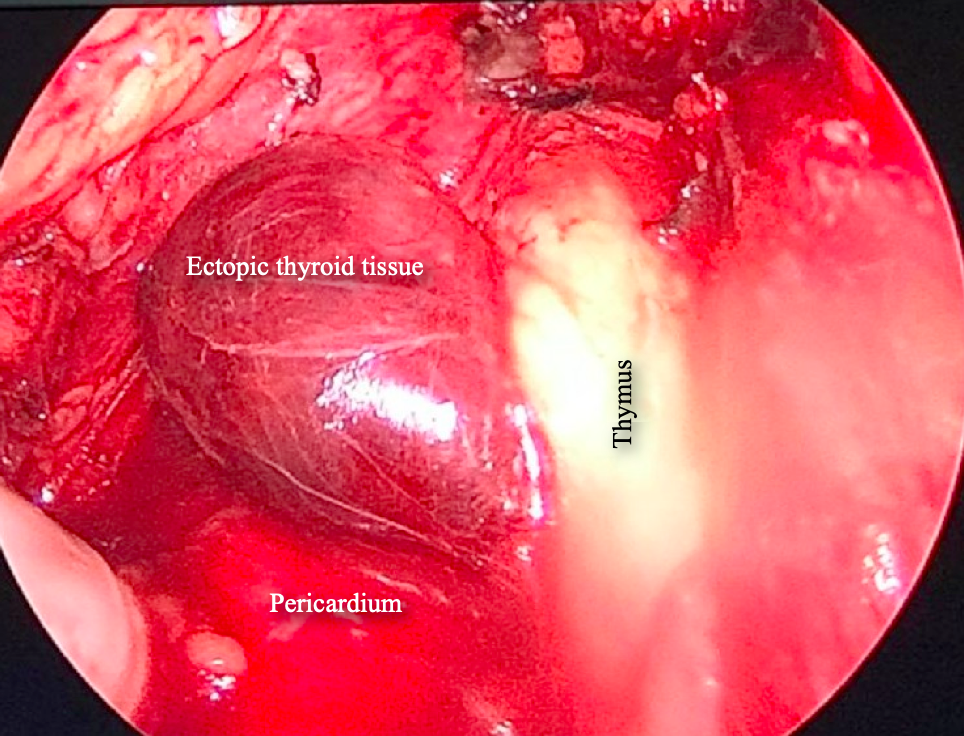
Figure 4. Videothoracoscopic view of the anterior mediastinum showing the dark red mass on the left side. No major feeding vessel was identified.
Intraoperative frozen section showed that the mediastinal lesion was not a thymoma but an ectopic thyroid gland (Figure 6A). Hematoxylin and eosin staining confirmed the diagnosis and depicted a normal thyroid tissue, no features of malignancy were identified. No thyroid tissue was found in the involuted thymus (Figure 6B).
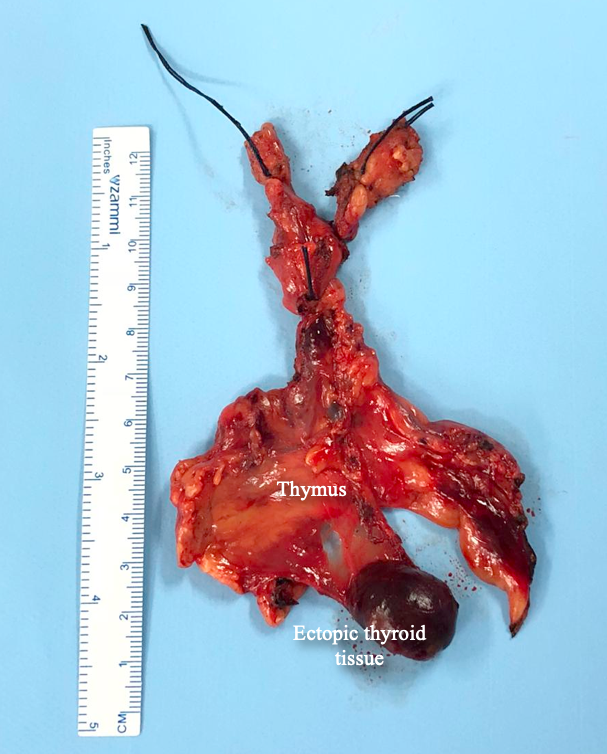
Figure 5. Specimen removed through the cervical approach. The thymectomy was performed on the assumption that the tumor was a thymoma. One can see the close relation of the lesion with the thymus. The thyrothymic ligaments were tied with 0-silk ties. Traction on the ligatures assists in the mediastinal dissection. The lesion showed no infiltration of surrounding structures.
The postoperative recovery was uneventful. Pain control was achieved with intravenous analgesics in the first postoperative day and oral analgesics afterwards. The patient was discharged from the hospital on the second postoperative day.
Discussion
The thyroid is the first endocrine gland to develop in the body during the third and fourth weeks of gestation (6). There are two types of endocrine cells in the thyroid: follicular and parafollicular, also called C cells. The follicular cells derive from the endodermal diverticulum at the foramen caecum in the tongue (median anlage) that descends in the midline together with the lateral anlages from the bilateral fourth pharyngeal pouches, which form the lateral thyroid. These follicular cells secrete triiodothyronine (T3) and thyroxine (T4).
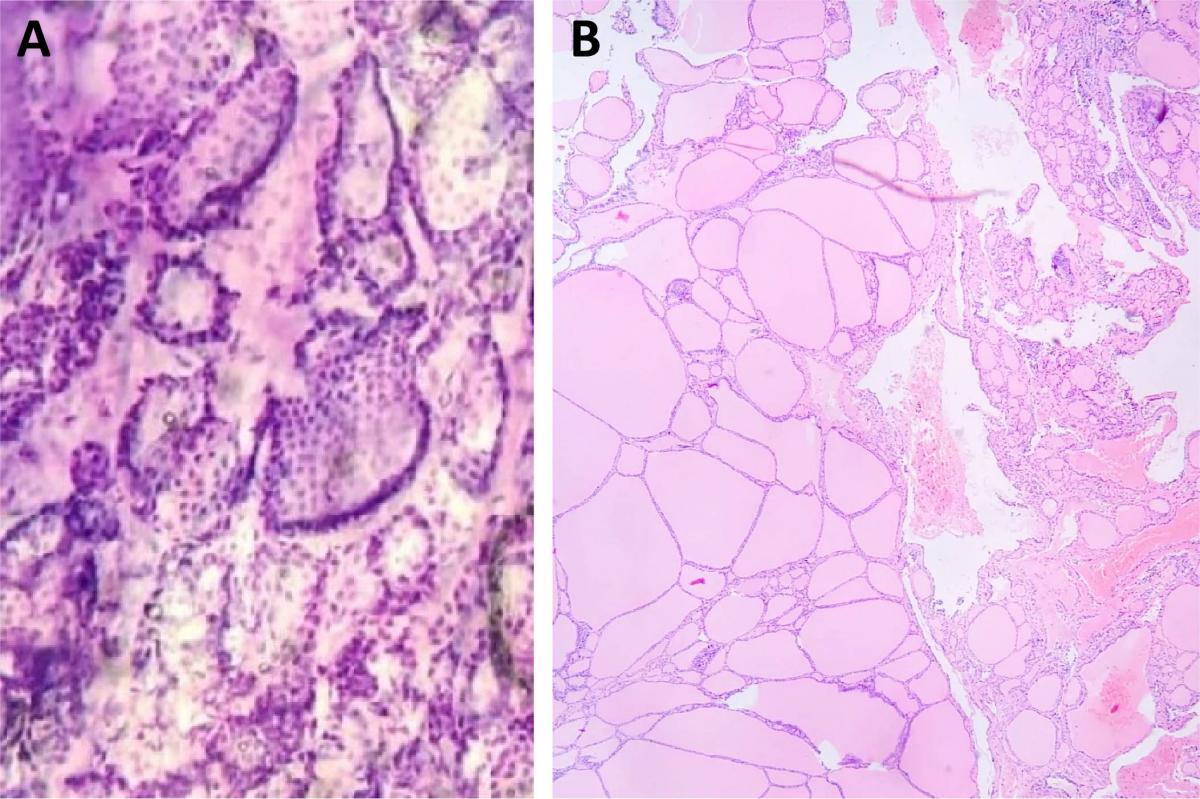
Figure 6. (A) Intraoperative frozen section of the mediastinal mass suggesting ectopic thyroid tissue, as thyroid follicles were observed. (B) Hematoxylin & Eosin stained section showing that the mediastinal mass was an ectopic thyroid. One can observe the normal thyroid follicles with colloid. No malignancy was detected.
The parafollicular cells produce calcitonin and derive from the ultimobranchial bodies in the fourth pharyngeal pouch, where cells from the neural crest migrate to (2). As stated, the thyroid primordium originates at the foramen cecum in the tongue and descends in the midline to the front of the first four tracheal rings in a well-established pathway known as the thyroglossal tract or duct, which undergoes atrophy after migration is completed (Figure 10).
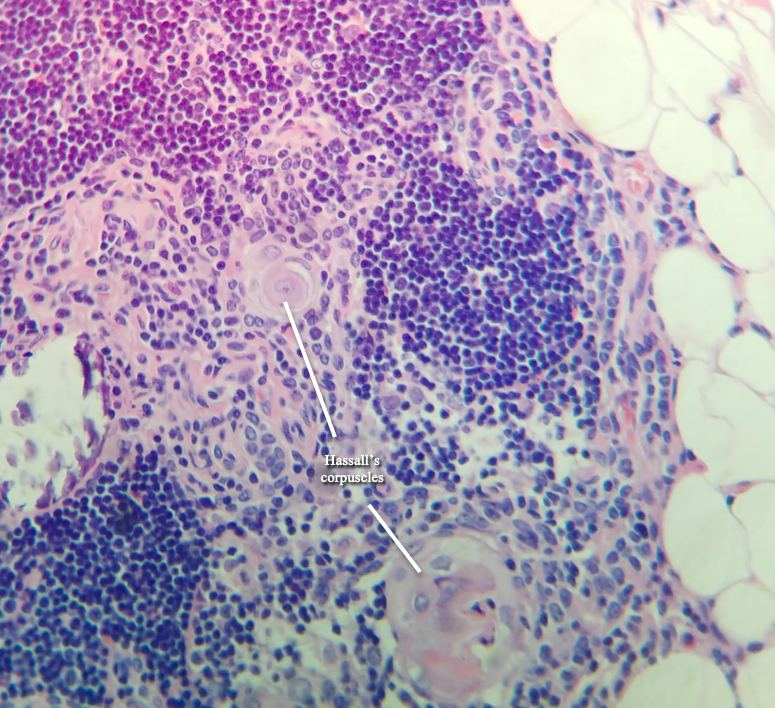
Figure 7. Hematoxylin & Eosin stained section of the thymus, showing thymic involution. No thyroid or parathyroid tissue was found in the thymus. Hassall’s corpuscles are evident in the picture.
The molecular mechanisms involved in thyroid dysgenesis are not fully known. Mutations in thyroid transcription factors such as TITF1/NKX2-1, which is responsible for thyroid-specific expression of thyroglobulin and thyroperoxidase, and others such as PAX8, HHEX, and FOXE1 in the developing thyroid might be an explanation (2, 7). FOXE 1 has a role in thyroid migration and it has been demonstrated that mice that are homozygous for mutations in FOXE 1 develop lingual thyroid (2), although this mutation has not been described in humans.
Ectopic thyroid tissue may be found at the walls of a persistent thyroglossal duct or thyroglossal cyst and in the lateral areas of the neck. The embryological development of the thyroid gland is closely related to the embryogenesis of the aortic sac and the heart. When the heart descends into the mediastinum, it can drag the thyroid down, which causes the development of an ectopic thyroid (2).
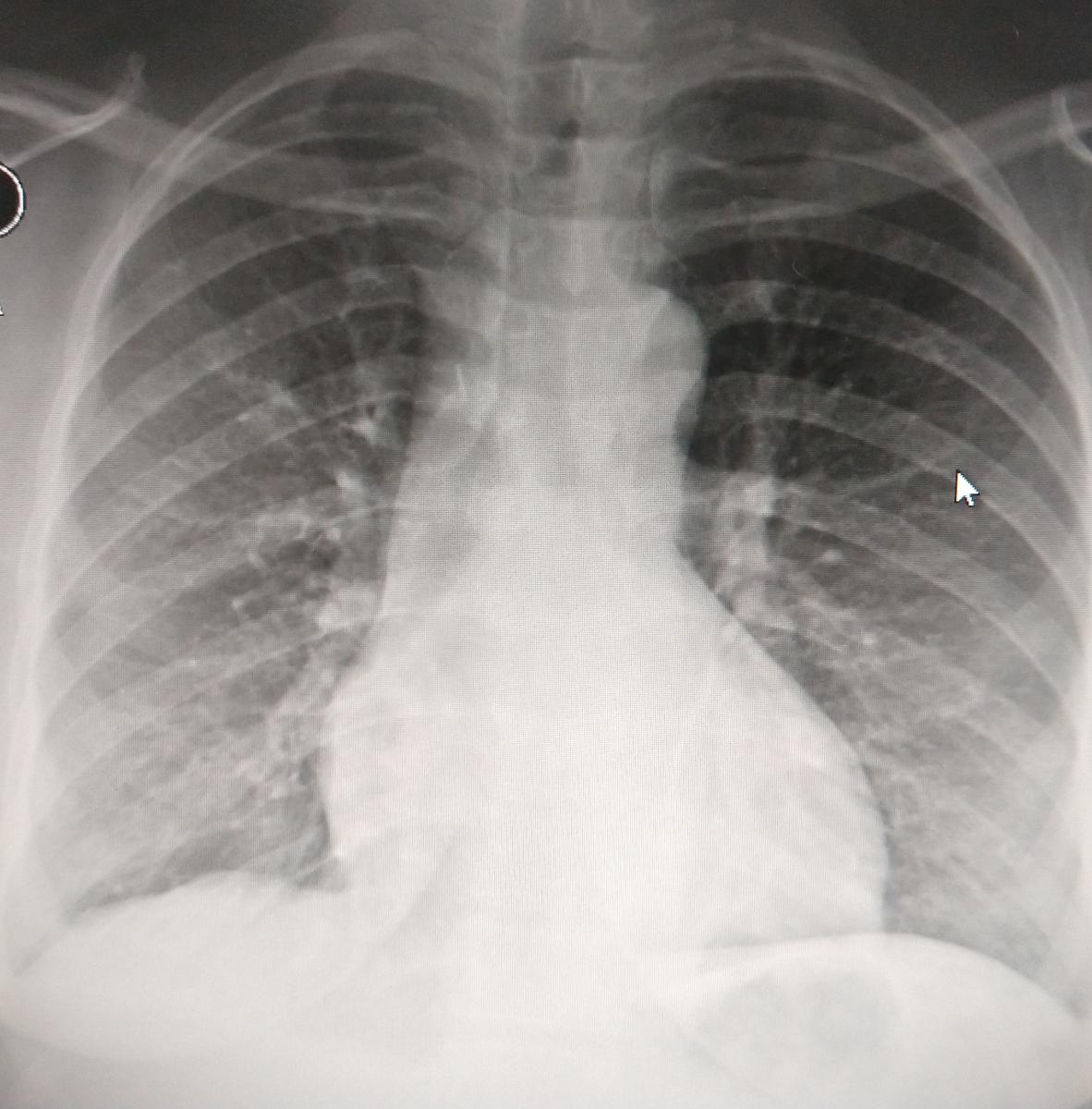
Figure 9. Chest x-ray on the second postoperative day when the patient was discharged. Lungs are fully expanded and no gross abnormality was observed in the operated anterior mediastinum.
Thyrothymic thyroid rests are deposits of ectopic thyroid tissue below the thyroid gland in the thyrothymic area; they can be of variable size but most of them are very small. They may present as separate nodules in 20% of the cases or they may have attachments to the thyroid consisting of thin sheets of thyroid or fibrous tissue. Because of the action of negative intrathoracic pressure or the weight of the nodules, they might migrate to the mediastinum and present as mediastinal ectopic thyroid (2). The thyrothymic thyroid rests may also be an additional explanation for the recurrence of intrathoracic goiter after total thyroidectomy.
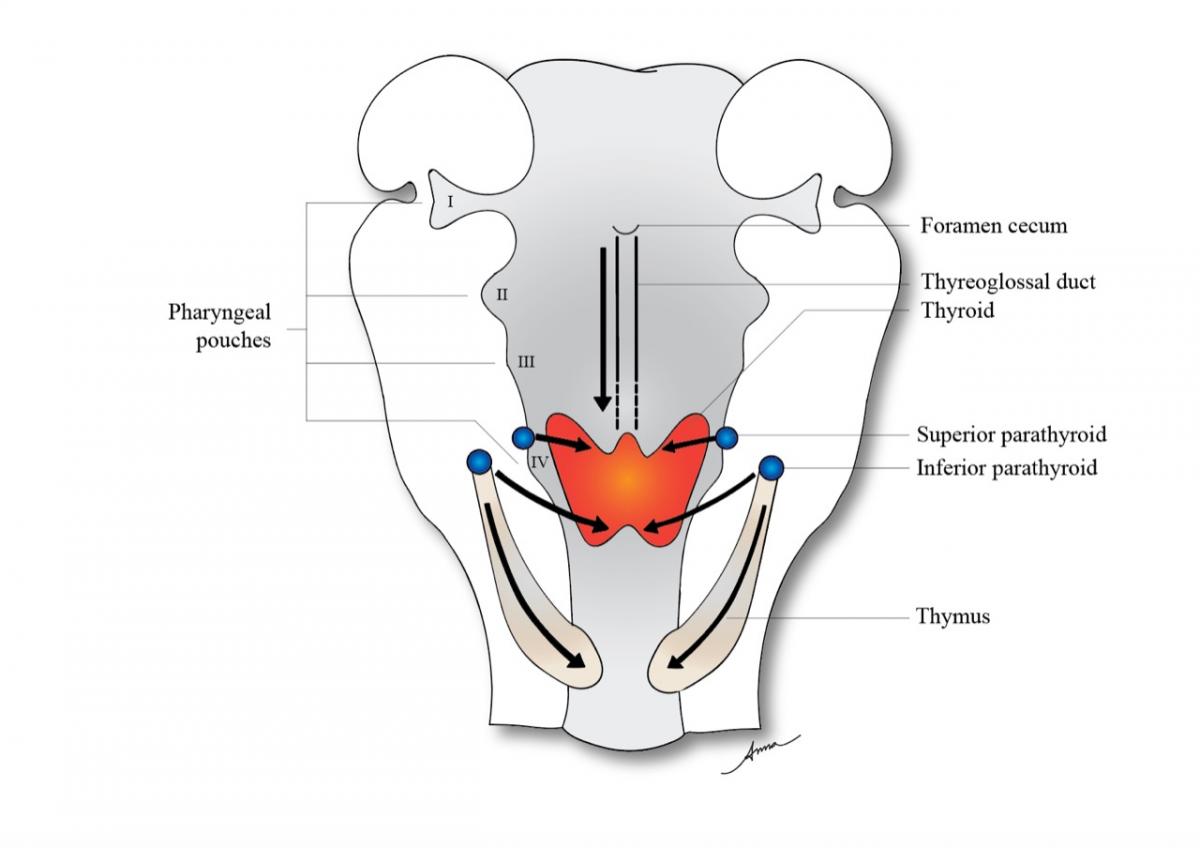
Figure 10. The thyroid primordium originates at the foramen cecum in the tongue and descends in the midline to the front of the first four tracheal rings in a well-established pathway known as the thyroglossal tract or duct. The embryogenesis of the thyroid, thymus, and parathyroid glands are closely related.
A substernal, retrosternal, or intrathoracic goiter is an enlarged cervical thyroid with an intrathoracic extension (Figures 11A and 11B). The vascular supply is in the neck, coming chiefly from the inferior thyroid arteries. Some authors refer to this as a secondary substernal goiter, and this is the most common type (5, 9). A mediastinal ectopic thyroid is defined as thyroid tissue outside the normal thyroid pretracheal location site with no connection to the cervical thyroid and having an independent intrathoracic vascular supply. It is also called a primary substernal goiter by some authors, corresponding to 1% of cases of ectopic thyroid (5, 9).
Santangelo and colleagues (9), analyzing 3,092 patients who underwent thyroidectomy between 2000 and 2013, found an incidence of ETT of 0.9% in this surgical population (1). In this same study, in 28 cases reported, only in 4 cases of ETT showed normal thyroid tissue (1).
ETT is more common in women at a male to female ratio of 1:4, and it can occur at any age (2, 10). The mean age of presentation is at 40.5 years of age. Only 1% of the ectopic thyroid occurs in the mediastinum and 90% are located at the base of the tongue, the so called lingual thyroid (1) (Figure 12). ETT has also been identified in trachea, esophagus, lung, heart (struma cordis), posterior mediastinum, and in subdiaphragmatic organs such as the stomach, duodenum, pancreas, porta hepatis, small intestine mesentery, adrenal glands, uterus, and ovary (struma ovarii) (2). It is important to bear in mind that in 70% to 90% of the cases, the ectopic thyroid is the only functioning thyroid tissue in the body (2).
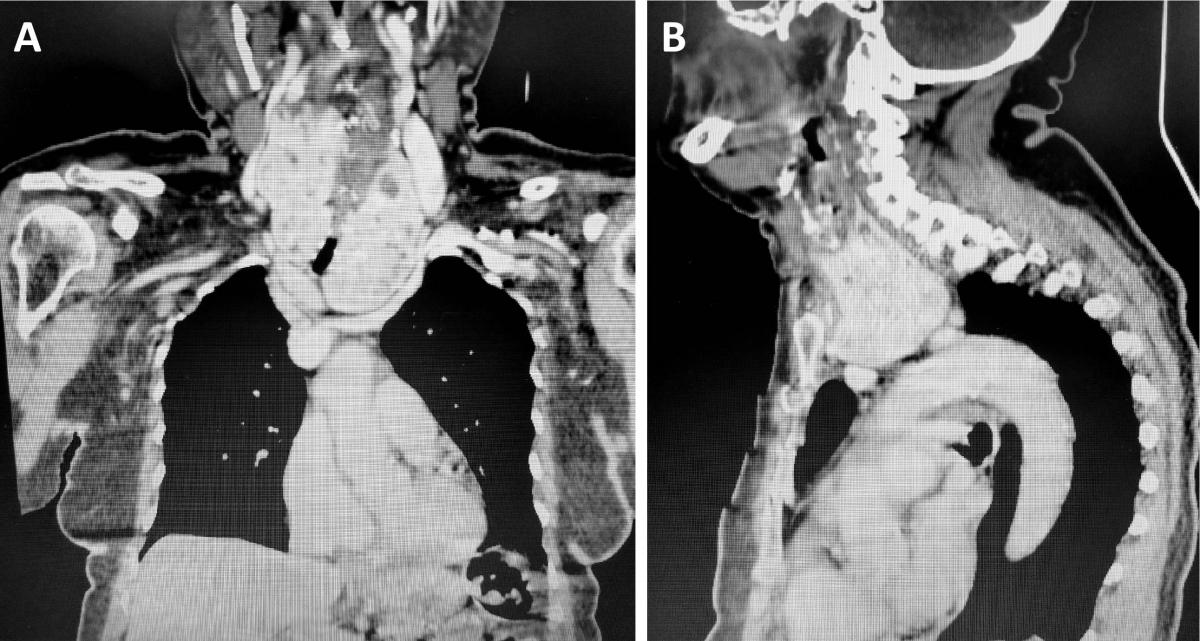
Figure 11. (A) Computed tomography of the neck and thorax (coronal plane) of a patient with a substernal goiter causing dysphagia and compression of aortic arch branches. One can see the enlarged cervical thyroid plunging into the mediastinum, the so called “plunging” or “diving” goiter. This is the most common type of mediastinal thyroid, also called secondary substernal goiter. The vascular supply is in the neck, chiefly from the inferior thyroid arteries. It is different from the mediastinal ectopic thyroid, which has no connection with the cervical gland and possess a distinct vascular supply that comes from intrathoracic vessels. (B) CT of the neck and chest (sagittal plane) of the same patient shown in panel A, with a substernal goiter (“diving goiter”). The enlarged cervical thyroid plunges into the mediastinum, “sitting” on the aortic arch branches. This patient had a history of cerebral vascular accident.
An interesting report is the one by Tiberti and colleagues (7) who reported a case of ectopic thyroid tissue in the iris of a 15-year-old boy. The tumor was discovered during a routine eye examination. After resection, histopathology revealed thyroid follicles with colloidal material. The patient had a normally located and well-functioning thyroid. The authors hypothesized that the intraocular thyroid could not be explained by embryogenesis and it could be the result of aberrant differentiation of local tissues by heteroplasia or metaplasia. Thyroid tumor was investigated and no abnormality detected.
Scintigraphy using Tc-99m, I-123, or I-131 is the most important diagnostic tool to detect ETT and shows the absence or presence of an orthotopic thyroid. Thyroid scintigraphy can also unmask additional sites of thyroid tissue. It is sensitive and specific for thyroid tissue in the differential diagnosis of midline neck masses. A false positive result must also been taken into account, since physiological uptake of the nuclear contrast can occur in the nasal mucosa, salivary glands, intestine, liver, and urinary bladder. Pathological uptake can occur in meningiomas, dacryocystitis, sinusitis, prosthetic eye and dental disease (2). In the case herein reported by the authors, a thyroid scintigraphy was not performed. The tumor was highly suggestive to be a small thymoma and because of this, the patient underwent investigation for myasthenia gravis. In addition, scintigraphy with I-123, I-131, or Tc-99m pertechnetate can be diagnostic but a negative scan cannot rule out this diagnosis. Resection for diagnosis and treatment had been decided. Finally, the patient underwent CT scan with iodinated contrast media, hampering a nuclear thyroid scan for several weeks.
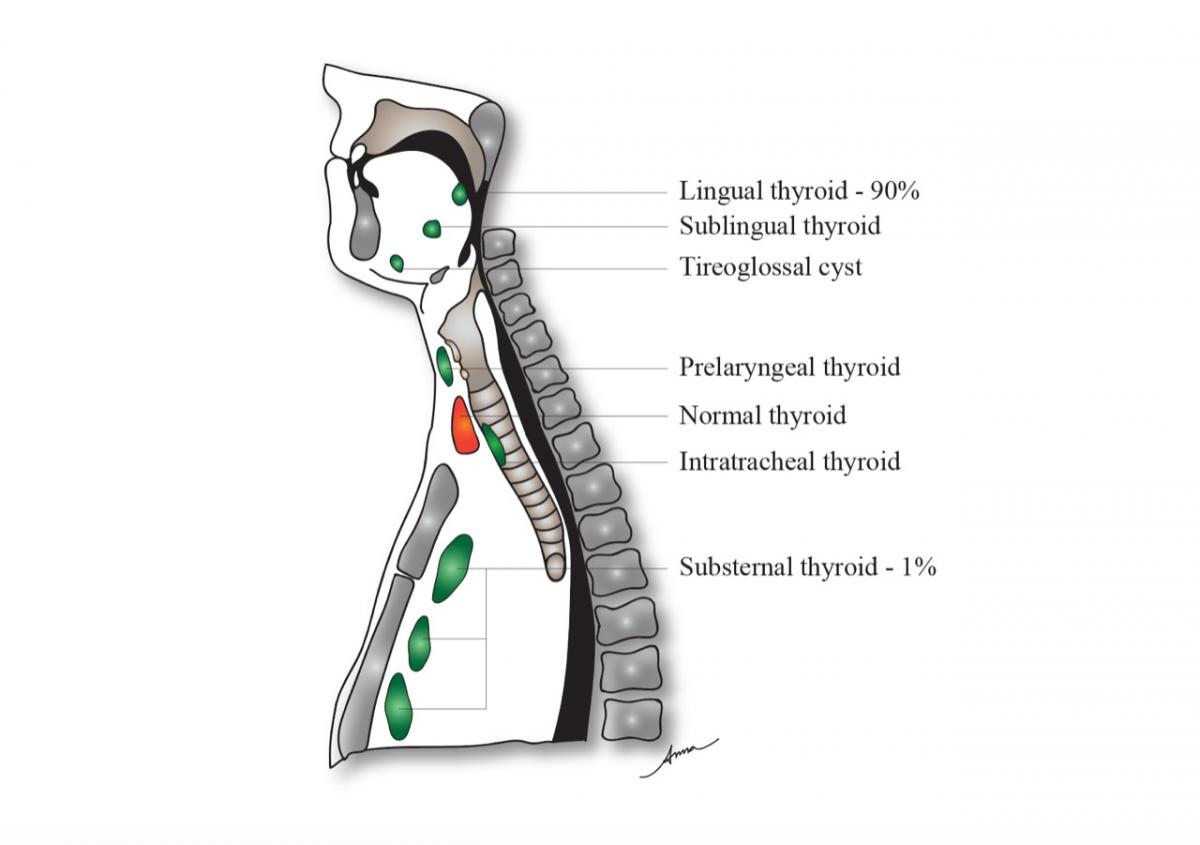
Figure 12. Different types of ectopic thyroid accordingly to its location established during the thyroid migration. Lingual thyroid is the most common type, corresponding to 90% of the cases. Mediastinal ectopic thyroid makes 1% of the cases.
Contrast-enhanced CT of ectopic thyroid demonstrated an intensely enhanced mass like in the case reported here. Noncontrast CT usually shows a high attenuation due to the iodine content (3). The relation with contiguous structures and compression of these structures can be analyzed as well. The same information can be gathered with nuclear magnetic resonance. It also assists in choosing the most adequate surgical approach.
ETT is commonly asymptomatic. Hypothyroidism was reported in approximately 33% of ETT cases in one study (1). Oguz and colleagues (10) reported an incidence of euthyroidism in 76.8% of cases, 13.1% of hypothyroidism and 10.1% of hyperthyroidism (3). In the case reported by the authors, the thyroid function was normal. When the ectopic thyroid causes any embarrassment to adjacent structures, chiefly compression, surgery is the treatment of choice. In the case reported, the ectopic thyroid was an incidental finding and small (24 x 12 mm), causing no symptoms.
In the case reported, although ectopic thyroid was one of the possible diagnoses, the author considered that the probability of a thymoma was much higher (40% to 50%), a thyroid scan could be negative, the patient was young and with excellent performance status, and because of the size and location of the mass the resection could be achieved through a less invasive approach such as the transcervical approach. The patient was discharged on the second postoperative day with an uneventful recovery.
The video-assisted transcervical approach is very appealing, chiefly because it avoids injury to the intercostal nerves, an important source of postoperative pain in thoracic procedures. Another efficient option to avoid surgical manipulation of the intercostal spaces is the subxiphoid approach, which allows the resection of larger masses. The size of the mass can be a contraindication for the transcervical resection.
Considering that the diagnosis of ectopic thyroid tissue could have been confirmed with a preoperative thyroid scintigraphy, observation of this mass could also be an acceptable approach instead of the surgical approach, as discussed by Raji and colleagues (3). Malignant transformation is reported to be an indication to resect an ectopic thyroid tissue even if the lesion is small and the patient is asymptomatic, as in this case. On the other hand, malignant transformation seems to be no higher than in the orthotopic thyroid tissue (8, 10), so one could state that surgical resection based on this premise is at least controversial. Santangelo and colleagues (9) reported an incidence of less than 1% of malignant degeneration in ectopic thyroid tissue, although one must always consider and investigate the possibility of thyroid tumor metastasis in cases of ectopic thyroid tissue (2).
It could be argued that thymectomy was not necessary in this situation, but the author could not see any harm to the patient using this video-assisted minimally invasive approach as proven by the prompt and uneventful postoperative recovery; the patient was discharged on the second postoperative day and required minimal analgesics at home. Also, the author could speculate that the possibility of thyroid rests in the thymus could support the thymectomy in these cases of anterior mediastinal ectopic thyroid. To date, there is very little research on the existence and incidence of normal thyroid tissue in cervical and mediastinal thymus (2). Dual ectopy and triple ectopy, although uncommon, have been reported (2). In most cases, the first lesion is lingual or sublingual and the second is subhyoid (the majority of the cases), infrahyoid, or suprahyoid.
Finally, the author would like to stress the importance, at least in his point of view, for the thoracic surgeon to master the video-assisted transcervical and subxiphoid approaches to resect lesions of the anterior mediastinum such small thymomas and anterior mediastinum ectopic thyroid and lymphadenectomy of the anterior mediastinum, when feasible, avoiding manipulation of the intercostal spaces.
References
- Ahmad U, Huang J. Tumors of the Thymus. In: LoCicero J III, Colson Y, Rocco G, eds. Shield’s General Thoracic Surgery. 8th edition. Philadelphia: Wolters Kluwer; 2019: 2144-2159.
- Noussios G, Anagnostis P, Goulis GD, Lappas D, Natsis K. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165(3):375-382.
- Raji Y, Gupta S, Pucar D, Keshavamurthy JH. Ectopic thyroid: the great mimicker. Lung India. 2018;35(3):248-250.
- Thuillier F, Venot J. Ectopic thyroid tissue in the anterior mediastinum with a normally located gland: a case report. Ann Endocrinol (Paris). 2012;73(1):34-36.
- Uludag M, Isgor A, Yetkin G, Citgez B. Ectopic mediastinal thyroid tissue: cervical or mediastinum originated? BMJ Case Rep. 2009;2009:pii:bcr09.2008.1004.
- Rajabi P, Eftekhari SM, Rouhani E, Baradaran A. Ectopic thyroid in stomach; a case report. Iran J Pathol. 2018 Winter;13(1):103-105.
- Tiberti A, Damato B, Hiscott P, Vora J. Iris ectopic thyroid tissue: report of a case. Arch Ophthalmol. 2006;124(10):1497-1500.
- To H, Karmakar A, Farrell S, Manolas S. Trans-cervical resection of a separate substernal goitre. Int J Surg Case Rep. 2017;41:373-376.
- Santangelo G, Pellino G, De Falco N, et al. Prevalence, diagnosis and management of ectopic thyroid glands. Int J Surg. 2016;28(Suppl 1):S1-S6.
- Oguz A, Tuzun D, Ozdemir E, Ersoy R, Yazgan AK, Cakir B. Importance of ectopic thyroid tissue detected in the midline of the neck: single center experience. Arch Endocrinol Metab. 2015;60(3):231-235.




