ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Percutaneous Catheter for Spontaneous Pneumothorax
McKay T, Franklin P, Steliga MA, Betzold RD, Kalkwarf KJ. Percutaneous Catheter for Spontaneous Pneumothorax. October 2022. doi:10.25373/ctsnet.21397425
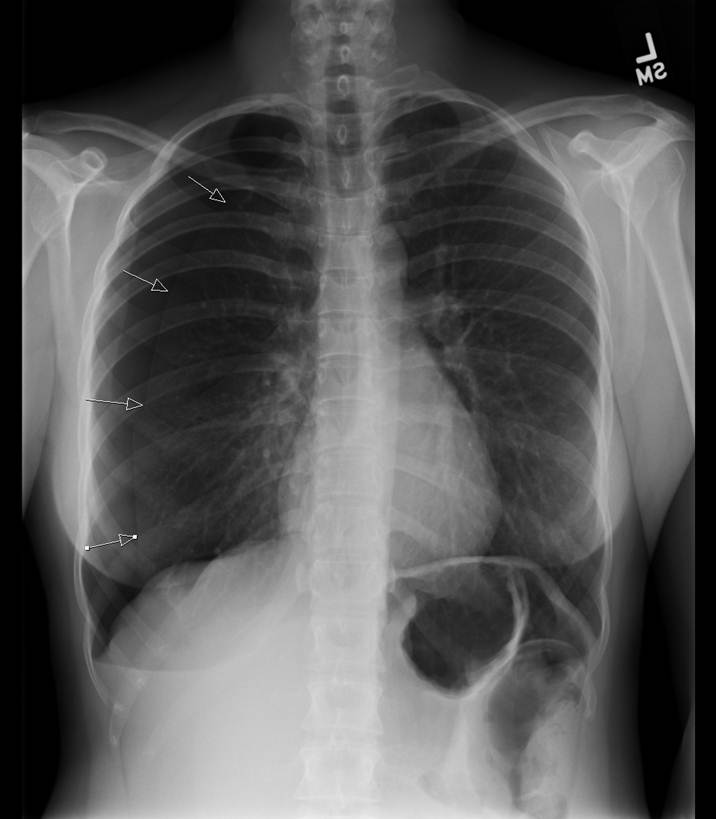
Spontaneous pneumothorax is defined as a pneumothorax without preceding trauma or iatrogenic causes. Primary or secondary spontaneous pneumothoraces are based on the absence or presence of underlying pulmonary disease. Though various treatment options exist, large bore tube thoracostomy is still widely utilized, as evident in the 2010 CTSNet survey with 63.9% reporting chest tube as initial therapy (1). At the University of Arkansas for Medical Science, the authors have changed the initial treatment of primary spontaneous pneumothoraces from large bore chest tubes to chest drainage via a percutaneous pigtail catheter and Pneumostat valve (Atrium Medical Corp., Hudson, NH). The authors have developed the following institutional algorithm for training residents and standardizing the procedure.
Patient Selection
Patients presenting with spontaneous pneumothorax without loculations are considered for this procedure. Exclusion criteria includes trauma, such as hemopneumothorax, and previous surgery. The typical patient presented to the emergency department is young, thin, and tall, with spontaneous pneumothorax.
Operative Steps
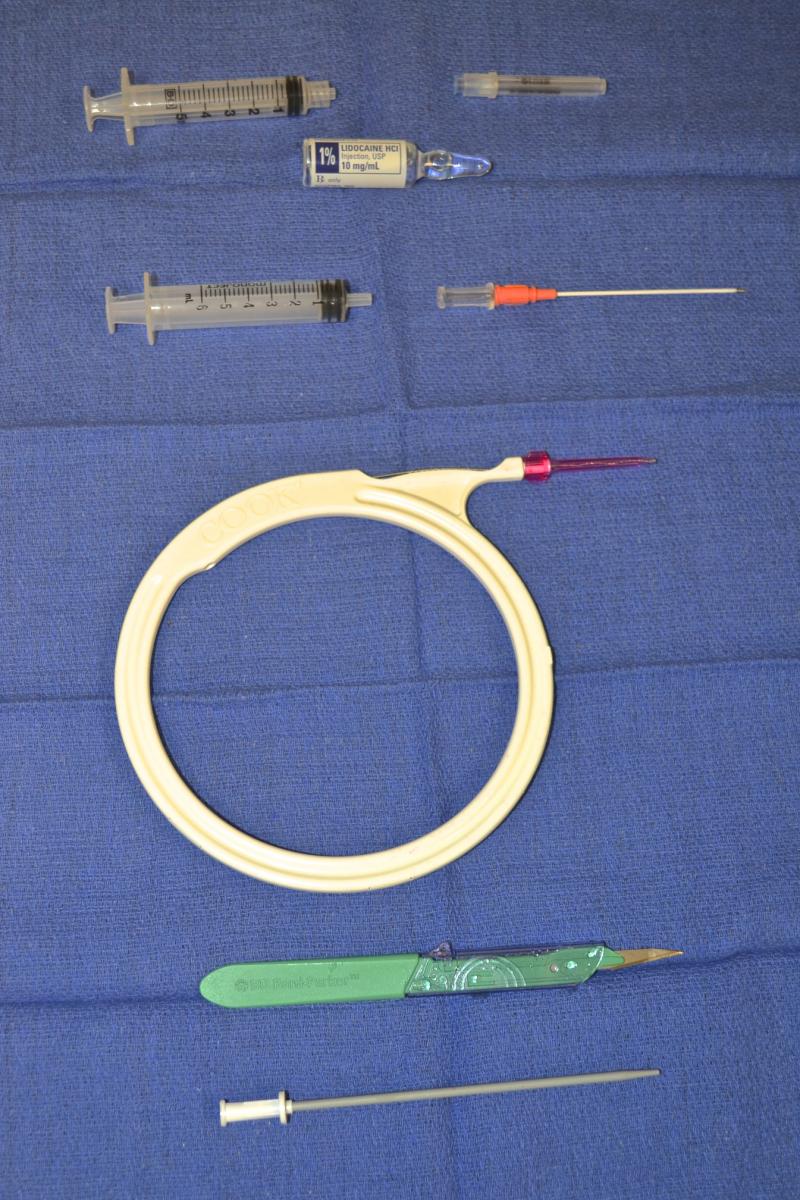
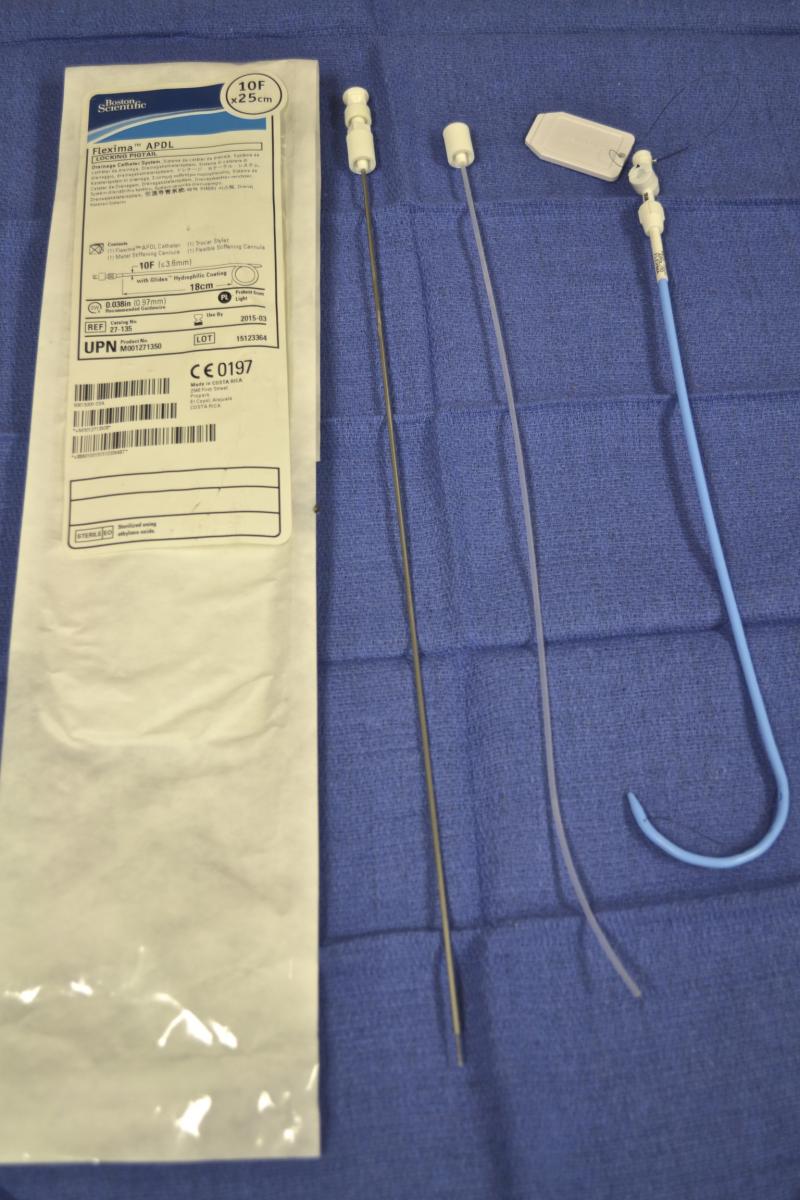
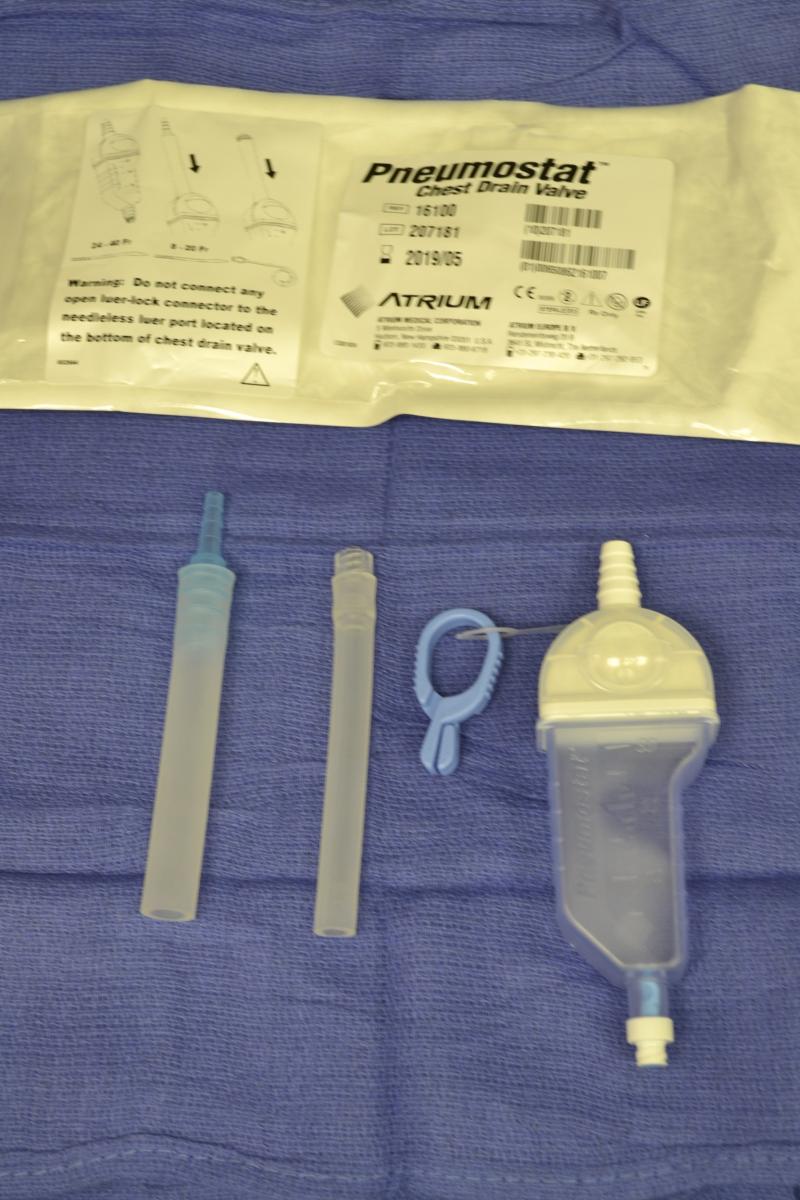
As with any procedure, informed consent is obtained and time-out conducted, including confirmation of identity and laterality with imaging studies (Figure 1). The site of insertion is the anterior chest wall, mid-clavicular line at the second intercostal space. A routine prep and drape is conducted (Figure 2). Next, local anesthetic (1% lidocaine) is infiltrated into the anterior 2nd intercostal space, staying just on the superior aspect of the rib. Typically, the authors have done this with local anesthetic (with minimal to no intravenous narcotics), and it is well tolerated (Figure 3). Once local anesthetic has been infiltrated, the introducer needle and catheter are used to aspirate air as the needle and catheter are advanced into pleural cavity (Figure 4). Once in the pleural cavity, a flexible guidewire is advanced into the pleural space (Figure 5). A small skin incision with a #11 scalpel facilitates passage of the dilator and subsequently the drain (Figure 6). The dilator is slowly advanced over the guidewire just enough to enter the pleural cavity. It is important to always maintain control of the end of the guidewire (Figure 7). Following dilation, the dilator is removed, and the percutaneous drain is advanced over the guidewire until the holes are all in the pleural cavity (Figure 8). Once the catheter is in the pleural cavity, tension on the drawstring locks the pigtail catheter. Finally, the pigtail catheter is connected to a Pneumostat valve or other water seal/collection device (Figures 9 & 10).
Institutional protocols and surgeon preferences may vary; our typical patient care flow is illustrated in the algorithm in (Figure 11). Once the percutaneous drain is placed, a plain chest radiograph is done. Failure of percutaneous drain placement is corrected with a standard thoracostomy tube. If there is improvement or resolution of the pneumothorax with the percutaneous drain, the patient is discharged home (typically within 12-24 hours). Lung re-expansion and air leak is checked as an outpatient. Successful treatment, defined as re-expansion and no air leak, leads to tube removal in clinic. A persistent pneumothorax or air leak is treated with an additional percutaneous chest drain, or the patient is scheduled for thoracoscopy.
 |
 |
| Figure 2. | Figure 3. |
 |
 |
| Figure 4. | Figure 5. |
 |
 |
| Figure 6. | Figure 7. |
 |
 |
| Figure 8. | Figure 9. |
 |
 |
| Figure 10. | Figure 11. |
Preference Card
- Components from triple lumen central line kit (Figure 12).
- Lidocaine
- Syringes
- 22g needle
- Introducer needle
- 0.032 in guidewire spring tip 60cm length
- #11 blade scalpel
- Dilator
- Suture - Flexima APDL Locking Pigtail 10F x25cm (Boston Scientific Corp., Marlborough, MA) (Figure 13).
- Vinyl Connecting Tube 30cm (Cook Medical Inc., Bloomington, IN) (Figure 14).
- Pneumostat Valve (Atrium Medical Corp., Hudson, NH) (Figure 15).
 |
 |
 |
 |
| Figure 12. | Figure 13. | Figure 14. | Figure 15. |
Tips and Pitfalls
- Bundling all necessary components and keeping them in a known place may facilitate use in an emergency department setting.
- Advance the needle only enough to enter the pleural cavity. Advancing the needle deeper into the thoracic cavity should not be done.
- If air is not found with the needle, try a different location, change to a standard thoracostomy tube, or use an image-guided technique. Do not probe deeper.
- Avoid sharp angulation of the pigtail catheter as kinks may render it ineffective.
- The product names listed are representative of what the authors use at their institution and can be adapted to similar products depending upon institutional preferences, availability, suppliers, etc.
- The pigtail drain listed is supplied with two stylets: a flexible inner plastic stylet (for placement over a guidewire) and a stiff sharp metal stylet (for trocar technique placement). The authors use only the guidewire technique discussed and discard the metal stylet, as the trocar technique is not used.
- At the authors’ institution, it was simpler to use multiple components of a triple lumen kit with a Pneumostat valve. Specifically designated kits or bundles can be built for this. However, since the authors have found that the case load for this procedure is fairly limited (<10/ year), this was a more easily achievable option.
Results
This technique is quite similar to central line placement with a few important adaptations. It has been easily learned and performed by residents at the authors’ institution, first in a simulation lab and also in the emergency department.
The use of small bore catheters for pneumothorax is not a new concept, since first described by Sargent in 1970 (2). While more data is needed (3), it is established that pigtail catheters are effective (74-100%), safe, less invasive, and allow the benefits of outpatient management (4, 5). The Pneumostat valve was also reviewed as a practical, safe drainage system, allowing increased ambulation and patient satisfaction (6). Not only have small bore catheters proved useful for primary spontaneous pneumothoraces, they have also been reported as effective for secondary spontaneous and iatrogenic pneumothoraces (7).
References
- 2010 CTSNet Result Summary for Survey: Management of Initial Spontaneous Pneumothorax.
- Sargent N, Turner F. Emergency treatment of pneumothorax: A simple catheter technique for use in the radiology department. AJR 1970;109:531-5.
- Brims FJH, Maskell NA. Ambulatory treatment in the management of pneumothorax: a systematic review of the literature. Thorax 2013;68:664-9
- Kelly AM. Review of management of primary spontaneous pneumothorax: Is the best evidence clearer fifteen years on? Emerg Med Australasia 2007;19:303-8.
- Kuo HC, Lin YJ, Huang CF, et al. Small-bore pigtail catheters for the treatment of primary spontaneous pneumothorax in young adolescents. Emerg Med J 2013;30:e17.
- Abdul Rahman MR, Min Joanna OS, Fikri AM, Adeeb SM, Zamrin DM. Pocket-Sized Heimlich Valve (Pneumostat) after bullae resection: a 5-year review. Ann Thorac Surg 2009;88:979- 81.
- Chen CH, Liao WC, Liu YH, et al. Secondary spontaneous pneumothorax: which associated conditions benefit from pigtail catheter treatment? Am J Emerg Med 2012;30:45-50.





Comments