Pericardial cysts are an uncommon benign congenital anomaly in the middle mediastinum. They represent 6% of mediastinal masses, and 33% of mediastinal cysts. Other cysts in the mediastinum are bronchogenic – 34%, enteric – 12%, thymic and others – 21%[1]. In the middle mediastinum 61% of presenting masses are cysts[1]. Pericardial and bronchogenic cysts share the second most common etiology after lymphomas[1]. The presented case is of a symptomatic pericardial cyst.
Case Presentation
Patient is a 29 year old female, who was diagnosed with a pericardial cyst when she was 17 years old during a work-up of asthma. Recently, the patient presented with a persistent cough, and a repeat CT scan revealed increase in size of the cyst to approximately 6x6cm (Figures 1 and 2). Her past medical history was significant for Wolff-Parkinson-White syndrome. On examination no abnormalities were found. Since the cyst was enlarging, causing significant anxiety, and possibly contributing to her persistent cough, resection was recommended. Her cardiologists felt that her WPW Syndrome was not a contraindication to surgery.
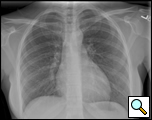 | 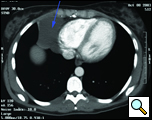 |
| Figure 1. Preoperative Chest x-ray. | Figure 2. Chest CT scan showing right cardiophrenic pericardial cyst. |
In the operating room, under general anesthesia and one lung ventilation, the thoracoscope was introduced at the right midaxillary line and the 7th intercostal space (Video 1 below). The cyst was readily visualized at the anterolateral aspect of the right pericardium, measuring approximately 9x6cm (Figure 3). The phrenic nerve was seen posterior to the cyst. The second incision was made at the anterior axillary line in the 4th intercostal space. A ring clamp was used to grasp the cyst (Figure 4). The third incision was made at the scapula line in the 5th intercostal space. Thoracoscopic scissors and cautery (at a low setting to minimize the chance of cardiac arrhythmias) were used through that port to dissect the cyst from the pericardium (Figure 5). The connection between the cyst and the pericardial space was identified. It was small, and was divided with the scissors. The dissection of the posterior aspect of the cyst completed the removal. The phrenic nerve was clearly visualized at all times. The pathology report confirmed the diagnosis of a benign mesothelial-lined cyst (Figure 6).
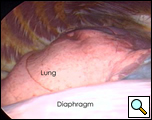 | 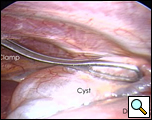 |
| Figure 3.: Intraoperative view of pericardial cyst. | Figure 4. Ring clamp retraction of pericardial cyst. |
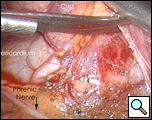 | 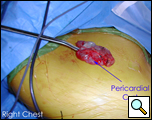 |
| Figure 5. Resection of cyst with view of phrenic nerve. | Figure 6. Resected specimen |
Patient had an uneventful post-surgical course, and was discharged home on post-operative day number two.
Discussion
Pericardial cysts occur at the rate of 1 person per 100,000[2]. They are thought to result from failure of fusion of one of the mesenchymal lacunae that form the pericardial sac. Seventy five percent of them have no associated symptoms, and are usually found incidentally during routine chest x-ray or echocardiography[1,2]. There have been about twenty reported cases of pericardial cysts presenting before the age of eighteen[3]. Seventy percent of them are located at the right cardiophrenic angle, 22% in the left, and the rest are in the posterior or anterior superior mediastinum[1,4]. The size varies from 2 to 28cm2. It is unknown if a particular size or position of the cyst corresponds to a higher rate of complications. If present, symptoms are usually due to compression of adjacent organs and include atypical chest pain, dyspnea, and persistent cough[2]. Cardiac tamponade, obstruction of right main stem bronchus, and sudden death are the life threatening emergencies that have been reported[2]. Cardiac tamponade is usually due to intra-pericardial rupture of the cyst, although tamponade due to spontaneous hemorrhage into the cyst has also been reported[2,4]. Other reported complications include right ventricular outflow obstruction, inflammation and infection, pulmonary stenosis, partial erosion into adjacent structures, atrial fibrillation, and congestive heart failure[2,5,6,7]. A few pericardial cysts resolve spontaneously, likely from rupture into the pleural space. The rates of spontaneous resolution or complications have not been reported.
Contrast CT scan has been the modality of choice to diagnose and to follow pericardial cysts[1,2]. However, no studies have been done to ascertain the superiority of contrast CT over MRI and echocardiography for diagnosis or for follow-up. On CT scan pericardial cysts are thin-walled, sharply defined, oval homogeneous masses . Their attenuation is slightly higher than water density – 30 to 40 HU[8]. They fail to enhance with intravenous contrast[8]. The frequency of follow-up imaging has not been established.
The management of pericardial cysts includes observation, percutaneous drainage, and resection. Observation is possible with repeated CT scans. However, there is little information regarding the safety and appropriate length of observation. For high-risk patients, a non-operative strategy may be followed. The longest reported follow-up lasted twenty five years, and yielded a 2.5L cyst at the time of resection . Aspiration is another therapeutic option. One literature review reported that one third of patients had recurrence after percutaneous drainage at three years . Injection of a sclerosing agent such as alcohol decreases the likelihood of cyst recurrence.
The indications for resection of pericardial cysts include large size, symptoms, patient concern, uncertainty of malignant potential, and prevention of the life threatening emergencies. Before the development of thoracoscopy, thoracotomy was the approach of choice. Currently VATS is the approach most commonly used. The VATS approach has many accepted advantages over open procedures, including cosmesis, improved intra-operative visualization, shorter post-operative recovery, reduced pain, and patient preference.
The infrasternal mediastinoscopic technique is an alternative minimally invasive approach, and may be used for anterior cysts. The advantages of this approach are better cosmesis, minimal pain, and the avoidance of single lung ventilation[13]. The robotic technique using the daVinci™ Surgical System may offer better surgical precision, and shorter operative time, post-operative stay and recovery period over thoracoscopic surgery[12].
While the morbidity and mortality of pericardial cysts are unknown, surgery has been demonstrated as the only definitive cure. Since operative risks of minimally invasive techniques are extremely low, it would seem reasonable to offer resection for all pericardial cysts in otherwise healthy patients for whom the risk of surgery is low.
References
- Lau CL, Davis RD. Chapter 56: The Mediastinum, in Sabiston’s Textbook of Surgery, 17th Ed, Philadelphia, Elsevier, 2004, pp. 1738-1739, 1758.
- Patel J, Park C, Michaels J, Rosen S, Kort S. Pericardial cyst: case reports and a literature review. Echocardiography 2004;21:269-72.
- Noyes BE, Weber T, Vogler C. Pericardial cysts in children: surgical or conservative approach? J Pediat Surg 2003;38:1263-5.
- Borges AC, Gellert K, Dietel M, Baumann G, Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg 1997;63:845-7.
- Komodromos T, Lieb D, Baraboutis J. Unusual presentation of a pericardial cyst. Heart Vessels 2004;19:49-51.
- Shiraishi I, Yamagishi M, Kawakita A, Yamamoto Y, Hamaoka K. Acute cardiac tamponade caused by massive hemorrhage from pericardial cyst. Circulation 2000;101:E196-7.
- Hoque M, Siripurapu S. Methicillin-resistant Staphylococcus aureus-infected pericardial cyst. Mayo Clin Proc 2005;80:1116.
- Demos TC, Budorick NE, Posniak HV. Benign mediastinal cysts: pointed appearance on CT. J Comput Assist Tomog 1989;13:132-3.
- Satur CM, Hsin MK, Dussek JE. Giant pericardial cysts. Ann Thorac Surg 1996;61:208-10.
- Stoller JK, ShawC, Matthay RA. Enlarging, atypically located pericardial cyst: recent experience and literature review. Chest 1986;89:402–406.
- Bacchetta MD, Korst RJ, Altorki NK, Port JL, Isom OW, Mack CA. Resection of a symptomatic pericardial cyst using the computer-enhanced da Vinci Surgical System. Ann Thorac Surg 2003;75:1953-5.
- Uchiyama A, Shimizu S, Murai H, Ohshima A, Konomi H, Ogura Y, Ishikawa N, Yamashita H, Matsumoto S, Kuroki S, Tanaka M. Infrasternal mediastinoscopic surgery for anterior mediastinal masses. Surg Endosc 2004;18:843-6.





Comments