ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Endobronchial Ultrasound (EBUS) Biopsy of Mediastinal Lymph Nodes
Rice D. Endobronchial Ultrasound (EBUS) Biopsy of Mediastinal Lymph Nodes. October 2022. doi:10.25373/ctsnet.21357426

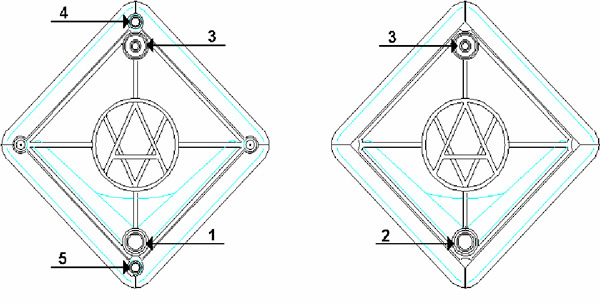
Figure 1: Olympus BF-UC160F-OL8 endobronchial ultrasound bronchoscope. Saline filled syringe attached to balloon inflation port.
Mediastinoscopy is the ‘gold standard’ method for determining the presence of nodal metastases in the mediastinum. Generally performed as an outpatient surgical procedure, it is associated with a low rate of serious adverse effects (<1%) and the procedure is highly accurate, with false negative rates reported to be between 6% and 9%. Endobronchial ultrasound (EBUS) guided fine needle aspiration biopsy of mediastinal nodes offers a less invasive alternative for histologic sampling of the mediastinal nodes. The procedure has been widely adopted by pulmonologists and is poised to replace mediastinoscopy in the future. For thoracic surgeons, the technique can be easily learned and it may be important to do so if our specialty is to maintain its traditional and important role in the diagnosis and staging of thoracic malignancies.
The EBUS bronchoscope (BF-UC160F-OL8; Olympus America Inc., Center Valley, PA) is similar in dimensions to a standard adult fiber optic bronchoscope. The 6 mm diameter scope has a curvilinear ultrasound (US) probe at its distal end which provides a 50 degrees linear continuous B-mode ultrasound image, with color Doppler capability to aid identification of vascular structures (Figure 1). Proximal to the US probe, and at 30 degrees to the long axis of the bronchoscope, are a fiber optic lens and a biopsy channel, through which a 22-G biopsy needle can be passed (NA-201SX-4022; Olympus America Inc., Center Valley, PA) (Figure 2). A disposable latex balloon is placed over the US probe, which is inflated with sterile water to provide a fluid interface between the probe and the tracheal wall.
Operative Steps
Scope Set-up
A 20 cc syringe filled with sterile water is attached to the balloon channel of the scope using an arterial line with a stopcock, and the channel filled with water (Figure 1). A disposable latex balloon is then carefully placed over the ultrasound probe, using the provided applicator and then inflated with saline. All air bubbles should be evacuated from the balloon prior to sealing it in place, which is easily done by applying pressure to the distal circular lip of the balloon with the tip of a gloved finger. Silicone spray should then be used to lubricate the scope.
Imaging Procedure
In the United States EBUS is usually performed under general anesthesia with use of a laryngeal mask airway and intravenous anesthesia [1] (Figure 3). This permits evaluation of the upper paratracheal nodes which may not be accessible if an endotracheal tube is used. A standard fiber optic bronchoscope is first used to determine anatomy, clear secretions and ensure absence of endobrochial disease that might make EBUS superfluous. The EBUS scope is then advanced into the trachea. When manipulating the bronchoscope through the vocal cords it is important to note that the visualized image is at 30 degrees to the long axis of the bronchoscope. The balloon is then inflated so that a small crescent of it may be seen at the bottom of the fiber optic image (Figure 4). The image is inferior to that of a standard bronchoscope because of the smaller diameter of the fiber optic system required to accommodate the biopsy channel and ultrasound. The [US-EXT] button on the ultrasound processor (EU-C60; Olympus America Inc., Center Valley, PA) toggles between the fiber optic and ultrasound views (Figure 5). Use of 2 monitors or a single monitor with picture-in-picture display is useful.

Figure 3: EBUS being performed under general intravenous anesthesia with use of laryngeal mask airway. The CV-180 video processor enables picture-in-picture display, which allows easy correlation between visualized anatomy and the ultrasonic image.
The easiest place to start ultrasound imaging is generally the right main bronchus and subcarinal areas. Pass the scope to the right side of the carina with the probe facing anteriorly and apply to the anterior wall of the RMB. This will bring into view the right main pulmonary artery. Vascular structures appear hypoechoic and pulsatile, and are usually readily discernable without using the color Doppler. If doubt persists flow within can be confirmed by switching to the Doppler overlay (B/CPD; Figures 5 and 6). Turn the scope 90 degrees counter-clockwise. This allows visualization of the subcarinal area from the right side. By moving the scope in and out the level 7 subcarinal node can usually be identified. If not, repeat this procedure in the LMB turning the scope 90 degrees clockwise instead. Once the subcarinal nodes are visualized it is relatively easy to identify other landmarks, by correlating anatomical location with the ultrasound image. It is useful to attempt to map out all nodes that you wish to biopsy first, before needle tract bleeding confounds the fiber optic image. The size of the node can be measured by freezing the US image [Freeze] and using the [Measure/Select] button and cursor scroll ball (Figures 5 and 7).

Figure 6a: Ultrasound image of R main pulmonary artery with (right) and without (left) color Doppler.

Figure 6b: Biopsy of right paratracheal node (arrow) with superior vena cava visualized in its long axis anteriorly.
Biopsy Procedure
The biopsy needle consists of a 22-guage needle with inner stylet housed in a flexible sheath, both of which may move independently of one another relative to the bronchoscope. The biopsy needle is passed through the biopsy channel and the housing secured to the bronchoscope by a flange (Figure 8). There are two main techniques to perform transbronchial puncture. The ‘quick jab’ technique is easiest and most useful for the subcarinal nodes or nodes along the main stem bronchi where the cartilage is thinner (Figures 8 and 9). With the node visualized by US, the sheath is advanced out of the end of the scope until the top right corner of the ultrasound image becomes slightly indented. This indicates that the end of the sheath is in contact with the wall of the bronchus and it is therefore safe to advance the needle. The guard for the needle is then released and using a quick jab the needle is plunged into the lymph node. If the needle is more slowly advanced there is a tendency for it to push the wall of the bronchus away from the scope, thus losing contact with the balloon and resulting in image loss. Once the needle is visualized within the lymph node, the stylet is moved in an out a few times to dislodge any bronchial epithelium that may have entered the needle, and then withdrawn. Suction is applied to the biopsy needle (typically negative 20 cc of air using a Vac-Loc syringe) and the needle passed in and out of the node approximately 10 times under US visualization. Suction is then released and the entire biopsy needle withdrawn. Smears are prepared by advancing the needle out of the sheath, reinserting the stylet and applying a drop of the aspirate to frosted glass slides. Air is used to ‘flush’ remaining aspirate material either onto additional slides or into RPMI medium for cell block analysis. Ideally 3 separate passes should be made into each nodal station to maximize yield (Video 1).

Figure 8a: Biopsy needle (NA-201SX-4022; Olympus America Inc., Center Valley, PA) secured to biopsy port of EBUS scope. The sheath screw is first released to allow the sheath to approximate the tracheobronchial wall. When the sheath is in contact with the bronchial wall a slight distorting effect can be seen at the upper right corner of the US image.
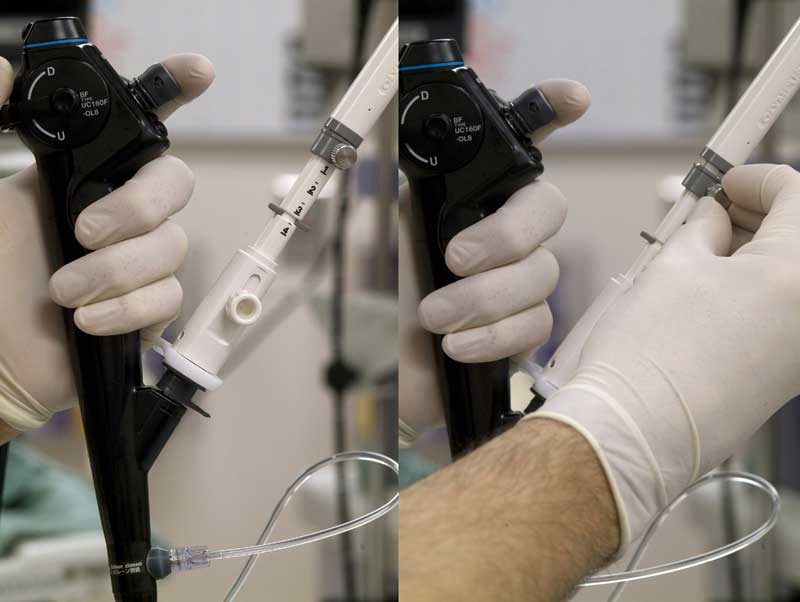
Figure 8b: With the sheath appropriately advanced and secured by retightening the screw, the biopsy screw is then released. This will allow the biopsy guard to slide out of the way in preparation for needle advancement.
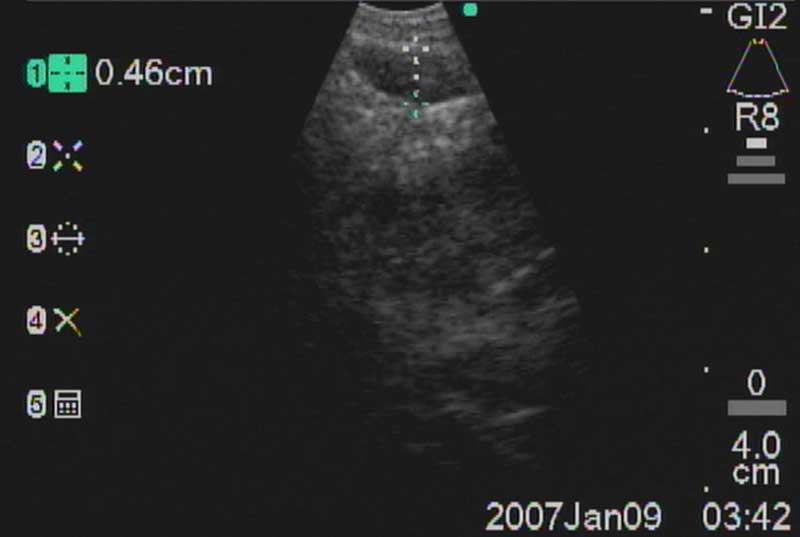
Figure 8c: Once the needle screw has been released, the biopsy needle can usually be easily advanced through the tracheobronchial wall and into the node using a quick, slightly forceful jab.
An alternative method of ‘visual’ needle placement is frequently necessary, particularly for the paratracheal nodes where the cartilaginous rings are thicker. In this case an appropriate intercartilaginous space is identified relative to the location of the node of interest, and the needle is placed in the interspace under direct fiber optic visualization. It is useful to have the tip of the needle and sheath just barely visible at the bottom right hand corner of the screen, and then advance the scope forward, directing the tip of the needle to the appropriate interspace. The tip of the needle should puncture the mucosa and with the needle now fixed in position, the scope can be slightly advanced. This causes the needle to assume a more perpendicular angle relative to the trachea and allows the needle to avoid the tracheal cartilages. The needle is then passed across the trachea and into the node, and aspiration proceeds (Figure 10, Video 2).
Mountain-Dresler nodal stations accessible by EBUS include stations 1,2,3,4,7,10, and 11 and lymph nodes with short axis dimensions of 5mm or greater may usually be biopsied without difficulty. Sensitivity and yield are maximized after 3 separate passes through each node. It is important to have real-time cytologic analysis and feedback in order to confirm that an adequate specimen containing lymphocytes has been achieved, which provides evidence of nodal sampling (Figure 11).
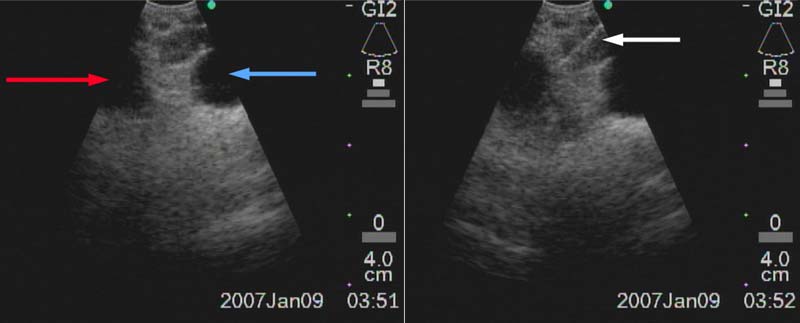
Figure 9: Right paratracheal node (4R) between truncus anterior of R PA (red arrow) and azygos vein (blue arrow). Biopsy needle is advanced through the node (white arrow).
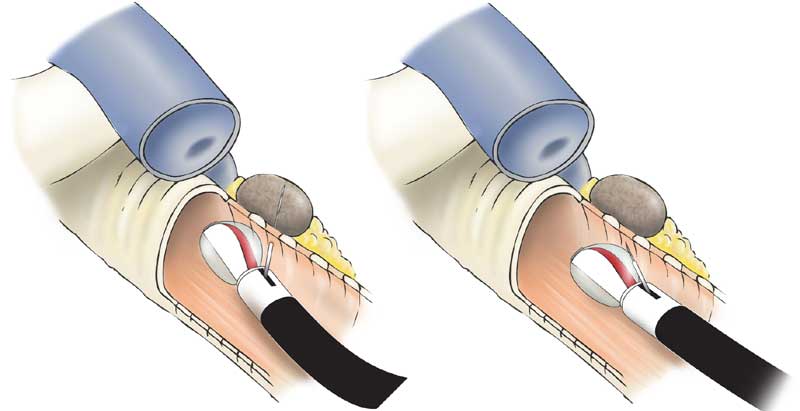
Figure 10: Visual placement of needle into intercartillaginous mucosa (left) with slight advancement of scope to increase angle of attack as needle is advanced (right) into a paratracheal node.
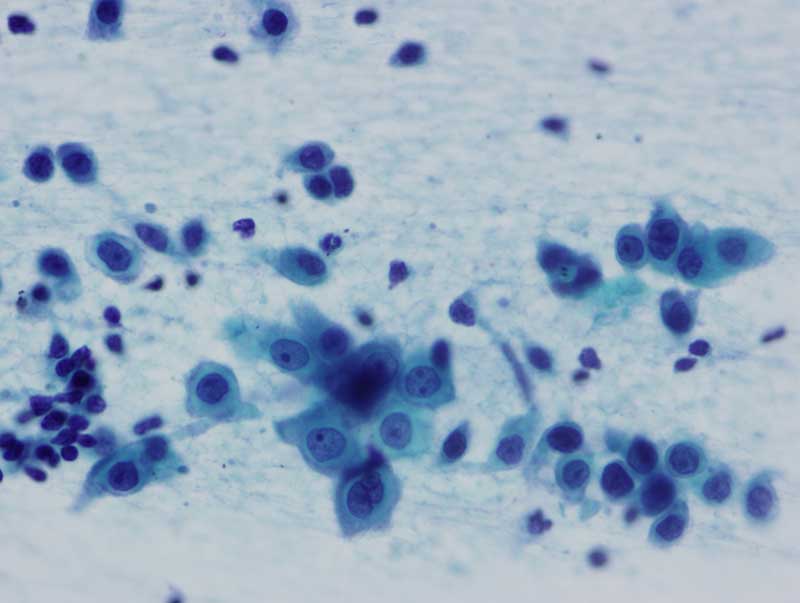
Figure 11: EBUS aspirated cells from a squamous cell carcinoma metastatic to a paratracheal lymph node. Smaller cells are lymphocytes.
Preference Card
- EBUS bronchoscope (BF-UC160F-OL8; Olympus America Inc., Center Valley, PA)
- EBUS ultrasound processor (EU-C60; Olympus America Inc., Center Valley, PA)
- EBUS 22 G TBNA needle (NA-201SX-4022; Olympus America Inc., Center Valley, PA)
- Standard fiberoptic bronchoscope (for preliminary evaluation and to suction secretions better).
- Two monitors, one for the US view, and one for the fiberoptic image. This will prevent having to toggle backwards and forwards between views. Alternatively, the newer Olympus video processor (CV-180; Olympus America Inc., Center Valley, PA) allows picture-in-picture display, obviating the need for a second monitor.
- Balloon for the ultrasound probe
- 20 cc syringe with tubing to apply suction to needle.
Slide preparation:
- Box of frosted glass slides (each separately marked for various nodal stations, with patient ID#). Usually you will make 2-5 slides per needle pass.
- Box of clear glass slides (for making smear).
- Slide holders with fixative (Carnoy’s soln.) (1 for each nodal station).
- Slide holder for air dried slides (1 is sufficient).
Tips & Pitfalls
- Nodes in the subcarinal area are straightforward to biopsy.
- Paratracheal nodes, particularly those at the left tracheobronchial angle may sometimes present a challenge, particularly if they are small. On the left side it is almost always best to visually place the needle in the intercartillaginous space, allowing the needle to hook the mucosa, and then advance the bronchoscope slightly to allow the needle to pass at more of a right angle to the wall of the trachea. Otherwise the needle will tend to pass at 30 degrees to the tracheal wall and it invariably hits cartilage instead.
- Extreme care must be taken when advancing and retracting the needle. It is important that the tip of the sheath be outside the scope when the needle is advanced to avoid deploying the needle inside the scope which will cause damage to it. Similarly, if the needle is not completely retracted into the sheath before withdrawing the needle from the scope, the exposed tip of the needle can damage the inside of the scope.
- For biopsy of more distal nodes (levels 10 or 11) it is often better to do so with the balloon deflated so that the scope can be passed more distally.
- Although not designed for use in the esophagus, the BF-UC160F-OL8 scope can be passed into the esophagus to access nodes in the periesophageal, perigastric and even celiac axis areas.
Results
Two recent reports have examined the utility of EBUS in staging of the mediastinum in patients with NSCLC. Yasufuku, et al, performed EBUS-FNA on 102 patients with potentially operable NSCLC. CT identified 92 suspicious (‘positive’) mediastinal nodes and PET identified 89 [2]. EBUS-FNA diagnosed mediastinal nodal metastases in only 37 nodes. The sensitivity, specificity and accuracy of EBUS-FNA was 92%, 100% and 98%, compared to 76%, 55% and 61% for CT, and 80%, 70% and 73% for PET. The false negative rate was 8%. In a separate study, Herth, et al, performed EBUS-FNA on 502 patients with CT enlarged mediastinal nodes and reported sensitivity, specificity and accuracy rates of 94%, 100% and 94% respectively [3]. In this study 37 nodes did not yield a positive diagnosis after EBUS-FNA, and 35 of these were found at surgery to have malignancy, resulting in a NPV of only 11%. Neither study reported any serious complications following the procedure.
Only one study has directly compared the accuracy of EBUS-FNA to mediastinoscopy for the mediastinal staging of lung cancer. Annema, et al, performed EBUS-FNA and mediastinoscopy on 21 patients with NSCLC, 16 of which had normal sized (<1cm short axis dimension) nodes [4]. Six patients had N2 or N3 nodal metastases, however only 2 were detected by EBUS (4 were detected by mediastinoscopy). The false negative rate of EBUS-FNA was 66%, and 33% for mediastinoscopy. Because of the low prevalence of N2/N3 metastases in this study, and the overall small number of patients included, it is difficult to draw conclusions form it.
Our surgical group has currently performed over 50 EBUS procedures without complication and training in EBUS is now part of our resident curriculum. Whether EBUS-FNA is as accurate as mediastinoscopy for staging of the mediastinum remains to be determined and is currently the object of an ongoing prospective study at The University of Texas M.D. Anderson Cancer Center. However, given the fact that EBUS avoids an operation, is easily practiced in an outpatient setting with less morbidity and discomfort compared to mediastinoscopy, it seems likely that it will become the predominant method for histologic sampling of mediastinal nodes in the future. Pulmonologists throughout the country have already embraced EBUS. With our detailed knowledge of mediastinal anatomy and technical proficiency, it is a simple and natural technique for thoracic surgeons to master.
References
- Sarkiss M, Kennedy M, Riedel B, et al. Anesthesia technique for endobronchial ultrasound-guided fine needle aspiration of mediastinal lymph node. J Cardiothorac Vasc Anesth 2007;21:892-6.
- Yasufuku K, Nakajima T, Motoori K, et al. Comparison of endobronchial ultrasound, positron emission tomography, and CT for lymph node staging of lung cancer. Chest 2006;130:710-18.
- Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006;61:795-8.
- Annema JT, Versteegh MI, Veselic M et al. Endoscopic ultrasound added to mediastinoscopy for preoperative staging of patients with lung cancer. JAMA 2005;294:931-6.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.