ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Phlegmasia Cerulea Dolens (PCD) as a Complication of Covid-19: Case Report
Jan A, Hayat MK. Phlegmasia Cerulea Dolens (PCD) as a Complication of Covid-19: Case Report. May 2021. doi:10.25373/ctsnet.14529258
Introduction:
Phlegmasia Cerulea Dolens (PCD) is a rare condition with high mortality and morbidity risk resulting due to massive deep venous thrombosis (DVT), arterial occlusion and subsequent compartment syndrome[1-2]. These patients are seen to present with a classical triad of severe pain, significant edema and bluish discoloration (cyanosis) of the affected limb[3].
PCD is the only accepted indication for thrombolysis and/or thrombectomy in patients with DVT, especially in those with signs of ischemia or gangrene. Accordingly, catheter – directed thrombolysis or urgent removal of the occluding thrombi using manual techniques (surgical or catheter-directed thrombectomy) should be seriously considered in this population of patients[4].
The management of this rare condition, its early recognition and initiation of prompt empiric treatment to prevent the lethal complications is vital. Treatment options include anticoagulation, systemic thrombolytics, catheter directed thrombolysis (CDT), pharmacomechanical CDT, surgical and percutaneous thrombectomy[5]. We report a 42-year-old male, post COVID-19 (2 months), presenting with PCD and treated with thrombectomy.
Case Report:
A 42-year-old male presented to the out-patient department of our tertiary care hospital with complains of swelling and discoloration of his left lower limb (LLL), on/off pain in the limb and cough. The cough was gradual in onset, present for the past 2 months, non-productive and associated with fever initially (not anymore). He also gave history of one episode of hemoptysis in the past 2 days. Two months ago the patient was in his usual health and had symptoms of cough and body aches. He was diagnosed as a case of COVID-19 and supportively managed. After two weeks, he developed Deep Venous Thrombosis (DVT) and was started on anticoagulation. The patient had no history of thrombotic events or thrombolysis. The DVT progressed in the next fortnight and the patient’s LLL swelling worsened.
Upon examination, the patient was not sitting comfortably in his bed with a mild cough and left lower extremity pain. Vitally stable. Systemic examination was unremarkable. Lower left limb examination revealed (Figure 1 and 2) grossly edematous limb, gangrenous with necrotic skin patches, purple in color, cold up to the knee, pulses were palpable in the femoral region while doppler signals were very weak below the popliteal artery, weak motor response and intact sensory responses. The right lower limb was normal.
Figure 1
Figure 2
An urgent CT-angiogram was performed (Video 1) which showed left Dorsalis pedis and Posterior tibial arteries not opacified with contrast. Diffuse subcutaneous and deep soft tissue edema. Left femoral, tibial and saphenous veins are distended (possibly DVT). Another significant finding from the CTA was the evidence of pulmonary embolism with evolving pulmonary infarcts bilaterally, multiple mixed cavitating and non-cavitating lesions in both lungs associated with ground glass haze and small left pleural effusion, multiple large mediastinal and upper abdominal lymph nodes, hilar lymph nodes eroding walls of bilateral pulmonary arteries.
Video 1
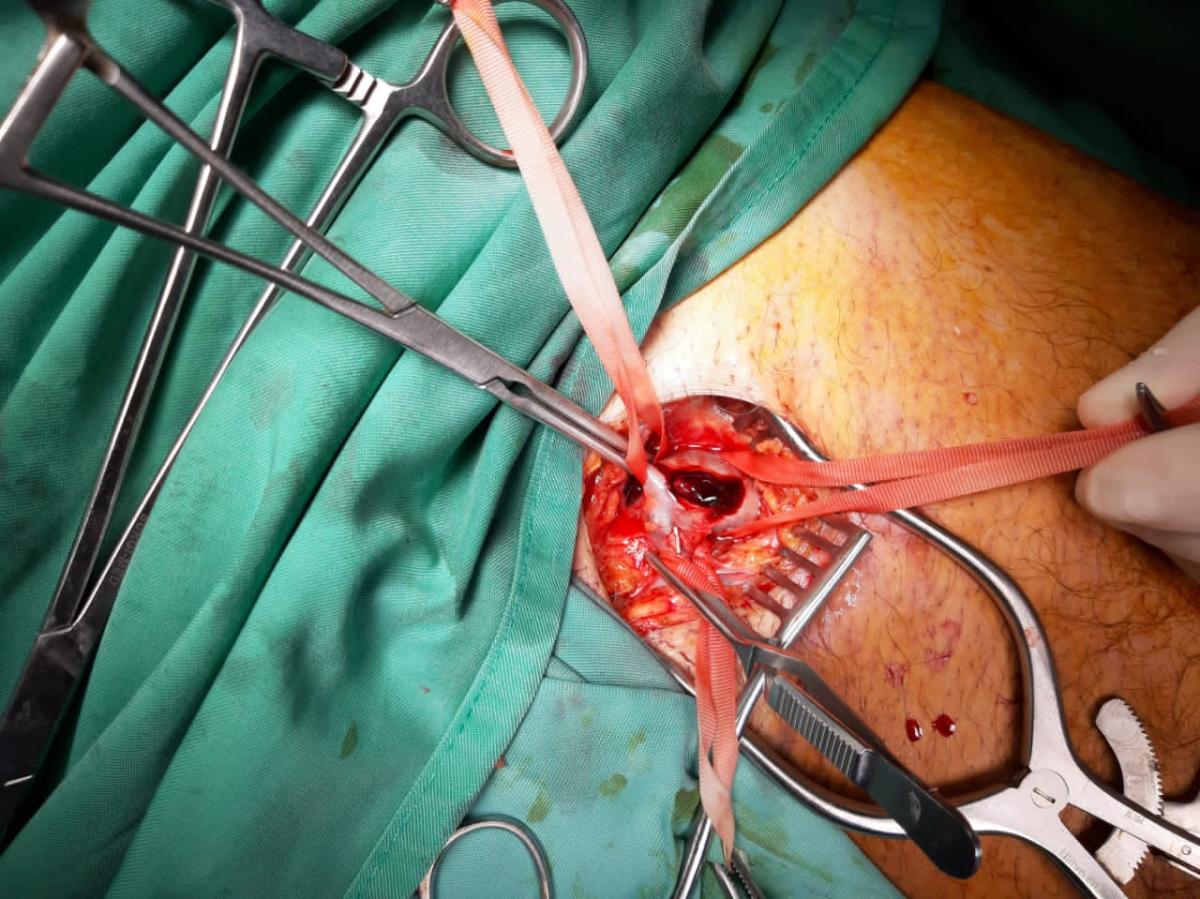
Left inguinal incision was given and femoral vein exposed. Proximal and distal control attained, and vein opened. A large clot was visualized with no venous flow (Figure 3). Thrombectomy was done using suction and fogarty (Video 2). Also, distal compression of leg was done to mobilize the thrombus. Both proximal and distal veins approached. Free venous flow was established. Veins closed with 6/0 prolene.
Video 2
The patient was kept on anticoagulation post operatively and mobilized on the 1st post-op day. Significant improvements in the sign and symptoms of left leg were seen post operatively and he was subsequently discharged to home.
Figure 3
Discussion:
Phlegmasia Cerulea Dolens (PCD) is an emergency and prompt actions are necessary for limb salvage. It has various risk factors, such as malignancy, heparin induced thrombocytopenia, femoral vein catheterization, anti-phospholipid antibody syndrome, and pregnancy, all these lead to hypercoagulable state[6]. The SARS-CoV-2 (COVID-19) is a respiratory syndrome associated with a hypercoagulable state in adult and hence a potential risk factor for DVT[7]. DVT complicating to PCD have been reported in cases of HIV-AIDS, COVID-19 and cancer patients[7-9].
It is a rare complication but can occur at all ages with no gender predominance of note as of now. However, the involvement of left-sided limbs in comparison to the right have been established. This is due to the compression of left common iliac vein by right common iliac artery[6]. The pathogenesis of PCD involves the complete obstruction of the superficial and deep venous return, resulting in increased interstitial tissue pressure, arrest of capillary flow, tissue ischemia, and eventually gangrene of the limb[10].
Diagnosis of PCD is mainly clinical. The use of Doppler ultrasound and computed tomography also has a role in ascertaining the diagnosis[11]. Once the diagnosis is established, I/V Heparin should be initiated and thrombus removal plan discussed and conducted[12]. Two options for thrombus removals exist, venous thrombectomy or endovascular methods that include catheter directed or pharmacomechanical thrombectomy. The mode of treatment will largely depend on the condition of the patient determined by the clinical categories of Acute Limb Ischemia (ALI)[13]. In this patient, the surgical thrombectomy option was opted for as the limb ischemia was increasing and immediate action was required to save the limb. In addition, the patient was unstable hematologically with an INR of 6.46 and APTT varying between 60 and 90 seconds, yet the patient’s condition was not improving. Post-operative examination of the left lower limb had shown significant improvement however, the swelling and discoloration had not subsided completely.
Conclusion:
PCD is a possible complication of COVID-19 and it can effectively be treated with open thrombectomy.
References
- Barnett D, Casey J. A Case of Phlegmasia Cerulea Dolens. Cureus. 2020;12(9):e10187. DOI: 10.7759/cureus.10187.
- Elsaid AS, AlQattan AS, Elashaal E, AlSadery H, AlGhanmi I, Aldhafery BF. The ugly face of depp venous thrombosis: Phlegmasia Cerulea Dolens – Case report. International Journal of Surgery Case Reports. 2019;59:107-10. DOI: 10.1016/j.ijscr.2019.05.021.
- Chang G, Yeh JJ. Fulminant phlegmasia cerulea dolens with concurrent cholangiocarcinoma and a lupus anticoagulant: a case report and review of the literature. Blood Coagulation & Fibrinolysis. 2014;25(5):507-11. DOI: 10.1097/mbc.0000000000000057.
- Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, et.al. Antithrombotic therapy for VTE disease. Chest. 2012;141(2):E419S-E496S. DOI: 10.1378/chest.11-2301.
- Said A, Kraft P, Sayed L. Delayed yet successful mechanical thrombectomy for Phlegmasia cerulea dolens in a limb with severe arterial disease and May-Thurner Syndrome. Case Report in Vascular Medicine. 2020;2020:1-5. DOI: 10.1155/2020/8866030
- Kou CJ, Batzlaff C, Bezzant ML, Sjullin T. Phlegmasia cerulea dolens: A life-threatening manifestation of Deep Vein Thrombosis. Cureus. 2020;12(6):e8587. DOI: 10.7759/cureus.8587
- Visveswaran GK, Morparia K, Narang S, Sturt C, Divita M, Voigt B, et.al. Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Thrombosis: Phlegmasia Cerulea Dolens presenting with venous gangrene in a child. J Pediatr. 2020;226:281-4. DOI: 10.1016/j.peds.2020.07.032
- Abah J, Menanga A, Njoyo L, Minkande JZ. Phlegmasia cerulea dolens: case report on a HIV-AIDS patient in a sub-saharian semi-urban practice. Pan African Medical Journal. 2014;19:282-85. DOI: 10.11604/pamj.2014.19.282.4385.
- Cojocari V, Casian D, Gutu E. Warfarin associated venous limb gangrene in cancer related DVT (Case report). International Journal of Surgery Case Reports. 2017;32:66-9. DOI: 10.1016/j.ijscr.2017.01.047.
- Aggarwal DG, Bhojraj SS, Behrainwalla AA, Jani CK, Mehta SS. Phegmasia Cerulea Dolens following heparin induced thrombocytopenia. Indian J Crit Care Med. 2018;22:51-2. DOI:10.4103/ijccm.IJCCM_183_16.
- Chinsakchai K, Duis K, Moli FL, Borst GJ. Trends in management of Phlegmasia Cerulea Dolens. Vascular and endovascular Surgery. 2011;45(1):5-14.
- Yang SS, Yun WS. Surgical thrombectomy for Phlegmasia Cerulea Dolens. Vasc Spec Int. 2016;32(4):201-4. DOI:10.5758/vsi.2016.32.4.201.
- Nogren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et. al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007;45(S):S55-67.
Discaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.