ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Adequate Cardiac Care? Conundrum for Nonaffluent Countries
Senza soldi is nati non fanno miracoli (without money the saints do not perform miracles) - Old Italian proverb
It is our choices, Harry, that show what we truly are, far more than our abilities. - Albus Dumbledore, Headmaster at Hogwarts in Harry Potter and the Chamber of Secrets by JK Rowling.
Abstract
Access to cardiac care remains disproportionate and diverse. About 80% of activist cardiac care, including cardiac surgery and/or catheter-based procedures, are available to 9% of the world population in North America and Western Europe. Even within Europe, > 50% of coronary artery surgery (CAS) output was catered to 28.6% population of Europe in Scandinavia, Benelux and Germany, Switzerland and Austria in 2001. The increase in the cost of activist cardiac care continues to rise with expanding role of technology. The issue of adopting appropriate technologies has been advocated earlier. The tricky semantics of 'appropriate' technology is often an euphemistic assertion of a two-tier system of health care and implies derogation of the nature of care affordable to the non-affluent countries. The guidelines by American or European Societies about adequacy of different cardiac care services and facilities are 'untenable' in many parts of the world. What remains unclear is what is adequate or appropriate--especially in nonaffluent countries where health care facilities are distributed unevenly.
Different standards emerging in different parts of the world need not be considered as inferior. Evolution of a unifying criteria of appropriateness and necessity would lead to a more uniform pattern of referral. In less affluent economies, a bias for wide-spread fostering of interventional technology may affect the quantum of care delivery in coronary revascularization. A realistic guideline for selection of appropriate strategy and adequate technology may already be in order for expedient care delivery to larger sector of population. A similar dilemma exists in management of valvular and congenital heart diseases.
Parity and equivalency of adequacy of different techniques or treatment options need be established. Both the patients and the doctors need have the freedom to have individually suitable option without the fear of having the therapy stigmatized as 'backdated' or 'inferior.' Definition of quality will keep on changing with time, culture and other considerations. What is an essential ingredient of quality of service/ training in one country/community/culture may be considered unnecessary/irrelevant in another. Role models for cardiac care delivery need be regional. 'Universal' standards based on reality in one country or one civilization will not bring in the desired quality or a greater quantum of care to greater number of patients. Comprehensive algorithms of universal appropriateness of patient selection and adequacy of treatment options/technologies need be developed on longterm outcomes. Avenues for updating technology in nonaffluent countries need to address the information and skills transfer methods, content of the literature and the education system, profession-industry relationship, the economics of increased output of care, and the role of obsolescent or evanescent technologies.
Introduction
The Global Forum for Health Research has defined the 10/90 gap as less than 10% of global spending on health research devoted to diseases or conditions that account for 90% of the global disease burden. About 50 to 60 billion US dollars are spent in the research and development for diseases that interest mostly the developed world and out of this only one tenth is spent for diseases affecting developing countries. This is true about the cardiac disease burden too. A nearly similar gap also exists in therapeutics arena--only about 10% resources are spent in cardiac care for the 90% of global cardiac disease burden. Nonaffluent countries bear the most of this disparity.
Insufficient cardiac care in the midst of scientific abundance of the present era is a ground reality in countries with limited resources. The increase in the cost of activist cardiac care continues to rise with expanding role of technology in surgical and medical cardiac interventions. At both national and grass roots cardiac care delivery level, one wonders how fast and in what manner new developments should be adopted. The overall cost of taking these developments to every man. woman and child is of concern even in developed affluent countries.
In the evolving scenario of globalized economic model and the so-called free market forces, the rural and the urban poor are going to be further marginalised in the process of structural adjustments as dictated by the international monetary fund, world bank etc. What are the options in nonaffluent countries to improve the health care, the income-generating capacities and access to a better quality of life with dignity that they deserve? The medical community cannot allow a large section of population in nonaffluent countries die without ever affording the 'correct' but expensive treatment. Harrison's concerns (in the Principles of Internal Medicine 12th Edition) remain relevant today: "It is becoming increasingly necessary to establish stringent priorities in the expenditure of money for health care...as resources become more and more constrained, it will be necessary to weigh the justification of performing costly operations that provide only a limited life expectancy against the pressing need for more primary care for those persons who do not have adequate access to medical care. In the last analysis the medical profession should provide leadership and guidance to the public in matters of cost control, and physicians must take this responsibility seriously without being or seeming to be self-serving. It is important, however, that the socioeconomic aspect of health care delivery not be permitted to interfere with the concern physicians have for the welfare of their patients."
Dimensions of the Problem
The tricky semantics of 'appropriate' technology--advocated for several decades--is an euphemistic assertion of a two-tier system of health care and implies derogation of the nature of care affordable to the non-affluent countries. On one hand, there is a move by the fiscal neoconservatives to justify and further foster two-tier system of health care for the haves and have-nots as ground reality, albeit unfair. On the other hand, there is growing social anger and justified medical objections to such discrimination in the clinical management of disease. Lewis Thomas had once succinctly noted "An extremely complex and costly technology for the management of heart disease has evolved, ... all kinds of electronic gadgetry, and whole platoons of new professional personnel to deal with the end results... Almost everything offered today for the treatment of heart disease is at the level of technology." How does one bring about equitabiliy? There are no easy answers.
What remains unclear is what is adequate or appropriate, especially in nonaffluent countries where health care facilities are distributed unevenly. In countries like China, India, etc, poised to make rapid economic progress, there are star hospitals with state-of-the-art medical facilities, highly skilled medical professionals, and people who can afford to pay for these services. At the same time, the millions there go without the benefits of primary health care in rural areas as well as in urban slums. During this phase of economic transition, there is also an epidemiological transition. Though the communicable diseases have been on the decline, the non-communicable and degenerative disorders of advancing age are on the rise. These countries thus face double burden of pre- and post-transition diseases.
The growth of cardiac surgery and catheter-based therapeutics has been neither universal nor uniform. Apart from the anglophone millieu of USA, Canada, UK, Australia & New Zealand, the practice of activist cardiac care in quantity and quality in the rest of the world remains highly heterogeneous. About 80% of activist cardiac care, including cardiac surgery, was available to 9% of the world population in North America and Western Europe [1] . The North Americans have the access to half the world's resources in cardiac surgery [2] while it is least (18 operations per million population) in Africa [3]. In disadvantaged countries, the technology-intensive and capital-intensive nature of cardiac surgery and transcatheter therapeutics tends to make it follow the inverse care law of Hart: the availability of good medical care tends to vary inversely with the need for it in the population served [4]. Country-wise cardiac surgical yield in number of procedures per million population and the proportion of subsets (viz., coronary artery surgery, valve surgery, etc.) have grown in parallel with the socioeconomic development of the countries [5]. But annual total cardiac surgical yield of a country perhaps reflects the expertise pool in the country. Brazil and India, despite their overall less-than-adequate economic performances, are among the top five countries in the world in annual total cardiac surgical yield. Moreover, new centers of excellence in service and research have emerged in Argentina, Brazil, China, India, Korea, Poland, Saudi Arabia, Thailand, Turkey, and other nonaffluent countries.
Economics and politics play a complicating role. Equity of access to cardiac surgery and catheter-based interventional therapy is of concern in many parts of the world--not just in the nonaffluent countries. Against a backdrop of widespread malnutrition, inadequate basic health care facilities and referral systems, and insufficient health budgets and its allocation to cardiac care, cardiac services may indeed be of secondary importance in some areas in Asia, Africa, Central and South America and eastern Europe. In many countries in these regions cardiac surgical centers were often started as political gratuity and 'prestige projects' rather than priority-based. There is a lack of database of available manpower, projected need and prevalent epidemiology in many such countries. Impact of activist cardiac care in changing the cardiovascular disease burden has also not been addressed in national planning in several countries.
Principles of Problem-Solving
The options for technology of treatment and patient selection for activist care must remain adequate for the disease status--irrespective of the patient status--rich or poor, wherever they are, in the developing or developed world. But even medically, the term 'appropriate' is perceptual. What is adequate in one sector or by one set of parameters is not adequate or appropriate in another scenario. The endgoals of all therapy, including activist cardiac care, need be prioritized. Hemodynamic improvement is different from increased exercise capacity, which is different from patient satisfaction. Patient satisfaction--a highly valued parameter in current ambience of private hospital management--needs be put in proper perspective. The quality of cardiac care is being increasingly equated with application of complexity of technology. The image of progress of a country's infrastructure is measured in terms of high tech facilities to suit the criteria of visible vociferous affluent minority and not the wellness of muted majority in a poor country. Whether it truly makes the quality of life better is now questioned as the mounting costs pose problems even for affluent countries.
The grammar of all service industries, including the practice of medicine, will always be tempered by society and time. Different ground realities of different communities will inevitably vary the nuances in practice of cardiac care, which may finally question our fondly held beliefs. Moreover, observed 'facts' in one community may be different in different communities due to differences in epidemiology and natural history of diseases. It is a sign of maturity of the discipline of cardiac sciences that different standards have started emerging in different parts of the world. Such different standards need not be considered as inferior. They may well open up the way for assimilation of new ideas. The guidelines issued by American College of Cardiology, American Heart Association, American Association of Physicians, and the European Society of Cardiology about adequacy of different cardiac care services and facilities may be useful benchmarks for North America or Western Europe, but are not applicable in many parts of the world. It is useful to remember that even these current western guidelines have evolved over a period of time to the present requirements.
Appropriateness in care recipient selection
The rate of coronary artery surgery or catheter-based procedures in number/million reflects also the pattern of referral for therapeutic intervention in different regions. A RAND corporation study had shown an earlier very conservative approach to coronary revascularization in UK compared to USA [6]. By 2002, coronary artery surgery productivity in UK had increased at a rate ahead of several other countries. Spain, Sweden, Switzerland, the Netherlands and UK have held Appropriateness panels to rate coronary revascularization [7]. Even within Europe, > 50% of coronary artery surgery output was catered to 28.6% population of Europe in Scandinavia, Benelux and Germany, Switzerland and Austria in 2001.
Another emerging reality is the declining quality of the surgical patients. A noticeable change in case-mix in recent times, especially in the western countries, is the increasing number of patients requiring repeat revascularization. By 2000, most major academic surgical centers in Europe had about 15 - 20 % patients with previous cardiac surgery. While the number of emergency coronary artery bypass grafting immediately after percutaneous coronary intervention (PCI) has remarkably dwindled, an increasing number of elective surgical patients now have had previous PTCA and/or stent. In obvious financial terms, explosive growth of PCIs and stents have also increased the total cost of therapy for coronary artery disease. The number of patients requiring coronary artery surgery after initially successful stenting or other PCIs is increasing all over the world. An Australian study has indicated that the cost of uncomplicated coronary artery surgery after initially successful PCI (without stenting) is 2.1 times the cost of uncomplicated primary CAS. This ratio will increase further as stenting becomes more utilized [8]. This scenario is compounded further by higher cost of recent surgical innovations, newer drugs and PCI accessories, and new stents. Affluent economies of Scandinavia, Benelux, Austria, Germany, Switzerland, Australia, France, Italy, UK, and USA have so far been able to absorb the raised cost. But even in these countries, finally the increased total cost may cater to a fewer number of patients having multiple episodes of revascularization. In less affluent economies, a bias for wide-spread fostering of interventional technology may affect the resources and thus the quantum of care delivery in coronary revascularization. The benefits of the post-genomic revolution have not yet arrived in the market place, even in USA or Europe. When they would do, they are likely to be expensive and push the total cost of treatment of ischemic heart disease still higher.
A similar conundrum exists in management of valvular heart disease. Rheumatic heart disease is still an important heart disease in India, China, Eastern and Southern Europe, Africa and South America, and common especially among the rural poor, who find even a single monthly injection of Penicillin unaffordable. WHO surveys in 1970s and 1980s and institutional reviews in 1990s [9] showed an extremely high incidence of the rheumatic fever (RF) and rheumatic heart disease (RHD) in the developing countries. Nearly 400,000 deaths occur due to RF and its heart complications. The global burden of the disease is estimated at a high 1% of school children. Economic impact of RHD is more profound than the mere morbidity or mortality of the disease. In India alone, even at conservative estimates, the incidence is 5 to 6 per thousand school children, and nearly 200,000 cases are added on every year.
The treatment consists of dilating or opening the narrowed valve (or replacing it), and is largely palliative since the rheumatic disease remains an ongoing process. Throughout the 1980s and early 1990s, the debate had raged essentially between a closed mitral commissurotomy (CMC) and an open mitral valvotomy (OMV) [10]. That is until early 1990s when the ubiquitous balloon made its appearance. All the arguments made earlier by the cardiac experts in favor of OMC, like opening the valve under vision with precision, ability to release the subvalvular structures to give maximal mobility to the valve, and reduced incidence of embolism, all were quickly forgotten as the interventionalists rushed to their cath labs armed with the new balloons! The mechanism of dilatation and hemodynamic improvement are similar in both closed techniques--surgical CMC and interventional mitral valve balloon dilatation (MVBD). But MVBD has now become the preferred method of treatment in the western countries since it is less traumatic and is cost effective when compared to open heart surgery. It is also important to remember that the disease has been controlled in the developed countries and the rheumatic mitral stenosis cases are rare. Some of the practicing cardiothoracic surgeons in the West, let alone the trainees, have not even seen a closed mitral commissurotomy and thus have no expertise in performing this simple operation. The scenario of declining expertise is fast catching up in the developing countries though the ground realities there remain widely different.
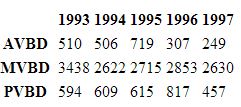
Meanwhile, by the end of the decade 1991-2000, disappointing results, dangers of the procedures and small size of selected subset of potential beneficiaries have led to waning of interest in balloon dilatation of valves. In Europe, aortic valve balloon dilatation (AVBD) decreased drastically while mitral valve balloon dilatation (MVBD) considerably reduced in number. The table indicates the declining trend even from the middle of the decade of 1990s [11].
Apparently the information of the changing acceptance of percutaneous balloon valve dilatation technology in Europe has not percolated down to India or other similar developing countries, and the multinationals continue their hard-sale marketing to compensate for the shrinking market in North America and western Europe.
Similarly, another case in point is the treatment of Patent Foramen Ovale (PFO). They are present in 10-15% of the healthy population. In USA, half the patients of stroke with a unknown cause have a PFO. Some 3.6 - 3.8% of medically treated patients with PFO suffer an embolic stroke each year in USA, a rate which falls to 3 - 3.4% in the surgically treated patients. Until the mid-1990s the conventional wisdom was to leave the asymptomatic PFOs alone as the outcome in adults with ASD was not considered to improve by surgical closure. Warfarin and surgical correction were reserved for those in whom aspirin was not effective or those who required warfarin or cardiac surgery for other reasons. Since the advent of the occluder devices, it is now claimed that the annual risk of stroke can be cut down to about 0.9% with catheter-mounted occluders. However. this more expensive procedure does not have less complications than surgery. In 8% patients, a second occluder is necessary to correct the residual shunt. Atrial fibrillation is common and some patients develop cardiac tamponade. Has the availability of technology and abundance of skilled manpower in the western countries led to reversal of earlier wisdom, and identification of a new subset, albeit very small, of patients for interventional approach? It amounts to perverse validation of Chandon's postulate (for every new product you can always market a new necessity, albeit unnecessary).
Marked ethnic diversity of epidemiology and natural history of different cardiovascular diseases has only recently been highlighted. This factor also needs to be accommodated in criteria for patient selection.
Evolution of a uniform criteria of appropriateness and necessity would lead to a more uniform pattern of referral. A realistic guideline for selection of appropriate strategy and technology may already be in order for expedient care delivery to larger sector of population and for survival of the profession.
Adequacy of treatment options and technology
Parity/equivalency of adequacy of different techniques or treatment options also need be established. Both the patients and the doctors need have the freedom to have individually suitable options without the fear of having the therapy stigmatized as 'backdated' or 'inferior.' Continuously updated flow of emerging information and relevance to ground realities are the best insurances for deciding appropriateness of treatment options and technology. In industrial production, mass customization connotes a process where products can be produced in bulk, but modified by the end user. This concept of relevant modification of products and services by the end users need be adopted by the cardiac care delivery systems in less affluent countries.
Good Clinical Practice protocols need to emphasize that different invasive treatment options may coexist with equitable outcomes. Thus the worth of different treatment options may be similar while vastly differing in technology, national cost and the price to the patients. It is necessary to get beyond the perceptual bias and ignore the flavor-of-the-season and not speculate about what will fly and what will die.
The treatment options in the management of in rheumatic mitral stenosis is an example of difficulties in making rational choices. The costs of a closed mitral commissurotomy (CMC), an open mitral valvotomy (OMV), and a balloon dilatation (MVBD) at a public hospital in India are approximately Rs. 3000, 40,000, and 75,000 (USD 60, 800, 1500) respectively and are correspondingly higher at private hospitals. The cost differential is similar in other nonaffluent countries. MVBD is not only a more expensive procedure in nonaffluent countries but also has no proven superiority and carries a small but definite risk of serious complications. Incidence of significant regurgitation after MVBD is uniformly around 5% in the literature and majority of these patients require emergency open-heart surgery for mitral valve repair or replacement. In contrast, CMC is one of the most economical heart operations and is effective in alleviating the symptoms of critical mitral stenosis in uncomplicated cases. The procedure has been around for nearly 60 years and has given excellent long term relief of symptoms and has had extremely low morbidity and mortality. In a series of closed mitral commissurotomy in over 9,000 patients in Bombay, India, mortality has been less than 0.5%, important regurgitation requiring mitral valve replacement occurred in only 0.2% patients. There is no need to discard such efficient and economical operation, especially in nonaffluent countries in favor of technically advanced but costly alternatives unless substantially better results are evident.
Similarly an exclusive bias for bileaflet valves over a tilting disc valve or a ball-and-cage valve among some surgeons in poorer countries often times puts valve replacement beyond reach of several nonaffluent patients because of the cost differential. Again, valve repair for rheumatic mitral disease may not be the current preferred mode in Caucasian population in Western Europe or USA, but it continues to save the day in South Africa or India. Until recently small aortic valve prostheses were frowned upon in the western world while they have been implanted routinely in other parts of the world with good results for a long time.
The cost differential between the surgery and catheter-based occluder for PFOs or coil embolization for PDAs is also significant in developing countries. Again, until today there is no observed scientific validation with adequate statistical power that total arterial revascularization leads to greater freedom from reoperation than LIMA, > LAD + SVG to other arteries. The proponents of evidence-based medicine may note to their dismay that a perceptual bias has been created in favor of total arterial revascularization. The craving for the so-called newest thing from the West is more often observed in the developing world. National inferiority complex (linked to commercial and military might ?) often leads to overall reduced efficiency in the quantum of cardiac care.
Role models of cardiac care delivery
Implantation of US or West European model of cardiac surgical service in other parts of the world may not be the answer, though on a simplistic level that would easily provide for uniformity. Regional role models of centers may be more appropriate: they would provide equitable quality of service and similar long term results. Quality is an elusive, nebulous concept and will keep on changing with time, culture and other considerations. Quality assurance is necessary to ensure uniform standards which need to be inclusive. Turmoil in UK in recent years over performance assessment of individual centers, surgeons have brought into focus the roles of multiple factors (including random chance) in final outcome. Air travel with all the present hassles possibly no longer has the quality it used to have in the past, but is now the acceptable standard for sake of security. Thus to decide on universal standards based on reality of one country or one civilization will not bring in the desired quality. What is essential ingredient of quality of service, training in one country, community, culture may be considered unnecessary/irrelevant in another. One may always wonder what the necessary standard would be: Model T Ford or Lexus LX300 with all add-on features when essential goal is transportation.
Obsolescent Technologies
Most of the basic surgical ideas or innovations have been introduced in the main stream since mid-1970s. Almost all the operative treatments, viz. arterial switch for TGA, CABG including use of LIMA, heart transplant, etc, had all been historically accomplished before the 1980s. Even the balloon angioplasty had been successfully introduced by Grunzig in 1976, providing a roadmap for the current use of stents and other percutaneous coronary interventions, valve dilatations, embolizations etc. In subsequent years mainly auxillary technological feats have been introduced facilitating these procedures.
Not all new technologies get embraced in the main stream of therapeutic options. Moreover, as technology develops further, some of the earlier technology gets discarded viz., disc oxygenators of 1950s became museum pieces as the disposable bubble oxygenators became standard practice in the 1960s. Expensive technologies with short shelf-life always play havoc with the economics of developing countries. It amounts to social irresponsibility of the industries not to publish studies on less-than expected efficacy of new technology and dump obsolescent technologies discarded by the West on the developing countries. Transmyocardial laser revascularization, introduced with brouhaha in mid-1990s, finally proved to be another technique that failed. Currently, robotic surgery (better termed as telekinetic surgery) technology is far from maturity and universal application. Several aspects of its current technology are likely to be obsolete in near future. To be realistic, an evolutionary gradient of technologies will always exist among countries. It will call for national and professional wisdom to choose technologies with longer shelf-life against the backdrop of national affordability. At times it is cheaper and more expedient for a nonaffluent country to make a quantum leap than to proceed through the whole process of technology evolution.
Economics of increased output of care
We find the relationship between cardiac surgical output of a region and gross national income, purchase power parity in international US dollar (GNI - PPP), to be nonlinear and multifactorial. Increased prosperity in terms of GNI-PPP of the countries boost cardiac surgery output only in the initial take-off and ascent phases. Subsequent rise in prosperity is not entirely reflected in further surgical productivity. Besides prosperity and international investor dependency, the national epidemiology, priorities, health care delivery system and political structure were determinants of increased quantum of care in terms of procedures/million population. For example, beyond a critical threshold, rise in GNI - PPP in European countries has not led to proportional rise in valve surgery output in number/million population. Per capita GNI - PPP in the Baltic states (7797 USD) in 2000 was lower than Middle European states (10434 USD) or even the Balkan states (7890 USD) yet valve surgery output in n/million population in the Baltic states (137) was much higher than that in the Middle European states (94) or in the Balkan region (66). Similarly, coronary artery surgery output in n/million population in the Baltic states (280) was higher than that in the Middle European states (248), or in the Balkan region (100).
Profession-Industry relationship
Cardiac care component of medical industrial complex has a high degree of built-in cost and profit ceiling and is de facto controlled globally by a handful of multinationals with a virtual monopoly. Most of the recent technologies in medical science are offshoots from the defense technology and its emergence with the end of cold war cannot just be co-incidental. Dominance of the capital-intensive market forces now threatens even clinical decisions and capability for correct care delivery. The so-called nexus between the industry and the doctors was always there and will remain there. The doctors need to recover their earlier role of prime mover and initiator and get out from their current status as clinical validators of the handouts of the industry. The latest or the most expensive is not always the best.
Though the epicenter of clinical application still remains in the developed affluent countries, the cradle of evolving technology (ET) is moving away from there for several reasons. The cost of commercial viability of products and devices and the medical industries as a whole has increased tremendously in USA and other developed countries in last two decades. Litigation-prone western society, preferential cost of development and preparedness of infrastructure in other countries have all contributed to such a move of ET. While it has opened up the Pandora's box of ethicality of 'trying out' of new technology, drugs, devices in nonaffluent country populations first, it has also focused the contribution of international cardiac specialists community. However, the politics and perceived notions of 'acceptability' has led to investment of the industries to certain so-called countries of excellence and has not translated into global groundswell of clinical services and facilities nor has it spawned growth of medical industries in all countries. On the other hand, growth of infrastructure medical industries for equipment and consumables, for example, in Brazil, India, China, Korea, etc., sometimes even at defiance of standard business norms have led to growth of cardiac surgery and catheter-based therapeutics in those countries. Thus, indirectly the market forces have modulated the international growth of cardiac care delivery. In fact, the cost of the equipment and the consumables and the unaffordable exchange rate (specially in the nonaffluent countries where they matter most) have been the greatest hindering factors in sustaining the cardiac care delivery programs. Perhaps a south - south trade will help in reducing the magnitude of the problem.
Bridging the gap
Technological advances, even just the available and affordable technology, have presented tremendous opportunities for comprehensive cardiac care. Despite infusion of technologies, quality problems may emanate from underuse, misuse or overuse of such technologies. Care delivery systems need to address both internal and external accountability of fiscal responsibility and demonstration of enhanced quality of care to society at large. Unhindered innovative thinking may be necessary in evolving new universal norms of appropriateness of treatment options, technologies and care recipient selection. By adopting cost-effective strategies in treatment, we could direct the limited resources to where they really should be, that is towards an effective preventive program.
Cost containment has been one of the compulsive considerations. Industries have their reasons for developing disposable once, only products which are cloaked in scientific data to avoid possible complications. Improvisations in the developing world often get around that prohibitive cost of disposables by resterilizing such products. Legislations have been brought in several western countries for compliance with such single use protocol. But multiple use of 'disposable' stabilizers in Off-Pump Coronary Artery Bypass (OPCAB) in India, Eastern Europe, Russia and several South American countries is a current reality, and has led to exponential growth of OPCAB in these countries, with reportedly similar morbidity and mortality as in the West. Many prolific cardiac surgical programs in the developing world owe their origin to humble beginning with resterilized cannulae and other products, and a great deal of improvisations. If rendering service is the ultimate goal, at times it is expedient to ignore the plumage and care for the dying bird.
Avenues for updating technology
Brain drain due to migration of related health professionals has been an oft-lamented, oft-cited cause of lack of growth of cardiac surgical facilities in many developing countries. Now may be the time to consider such migration as a move to brain sanctuary. Activist cardiac care centers demand expertise which cannot be sustained in absence of adequate work load and adequate working conditions. Moreover, such migration allows for higher turnover in limited training and work positions in cardiac surgical facilities in source countries. Besides inflow of remittances, it allows for future and potential bridges for flow of information and technology and investment, as has been noticed in Hungary, Greece, Turkey, India, Thailand, and the Philippines. Restrictive legislative measures, as introduced in some countries, may be short-sighted measures. Free migration of related health professionals may pave the way for bidirectional movement for outsourcing at a later stage and will foster growth of cardiac surgical facilities.
Information and skills transfer
Rapid growth in communication technology and internet sites have helped to provide access to information and dissemination of knowledge to bridge the gap of scientific isolation of cardiac surgeons in the disadvantaged countries with little time lag. But there appears to be a disconnect in medical literature from clinical reality. The bulk of the literature seems to accent on the so-called cutting edge. In the cardiac surgical literature in the last 5 years there have been a disproportionately higher number of papers on total arterial revascularization, homografts, Ross procedures, off-pump coronary artery bypass surgery, etc., while even in the developed world they are not practised universally. But these signals from the literature do distort the priorities in nonaffluent countries. Resources get diverted to exotic diseases and technologies with short shelf life, thus accentuating the 10/90 gap. Besides the cutting edge information, current medical literature needs to reflect the current reality of practice to foster awareness of appropriate care.
High profile visits of 'expert' teams from the developed world often have rather low impact as the soil may not be ready for the seed. Preparedness is often lacking not in absorbing the technical expertise but in infrastructure and the acceptance of the recipient community. Moreover, ground realities of the economics of the recipient countries are often different. Such help in the past has been inspired as much by altruism as by the financial pressure of the sponsoring organizations (private or government or joint sector). Moreover, in certain instances such exercises have degenerated into colonialist harvesting of patients. Help from the developed world to foster activist cardiac care in disadvantaged areas of the world has to come as aid to equal partners, and not as investment in potential colonies. It has to address primarily the needs of the recipient community and not the future needs of the 'exporters.' In absence of fairness, the recipients will always find out better alternate source of technology - transfer. Cardiac care is not one more commodity in technological neocolonisation. Globalization has acquired unsavory connotation in recent times. Any exercise overtly towards that goal is likely to become counterproductive.
Altruism and charity has been the basis of some international efforts in information and skills transfer in cardiac surgery to nonaffluent countries. Local training in recipient countries and collateral training in existing regional centres need to address the long-term resources and restraints of recipient countries in developing the norms and avenues of growth.
This paradigm has been compounded by current out-sourcing in the trade in health services and related factors. Cross-border telediagnostic and consultation services from USA hospitals to Central and South America and Mediterranean, from India to Nepal and Bangladesh, from China, Japan and Singapore to South Asian countries, from Australia to Asia-Pacific countries have all carried the pattern of cardiac care of the source hospitals to recipient hospitals and communities even though the pattern of the source centers varied considerably. Cross-border specialty services at a lower cost also change the reality of cardiovascular disease burden lowering of different countries. A decade ago, several USA and West European centers provided cardiac surgical care to several patients from Asia, Middle East and Africa. Today a large number of coronary artery bypass and other open heart operations in India at a lower cost is provided to not only patients from neighbouring countries, Eastern Mediterranean and East African countries but also from affluent western countries. Outsourcing of resources, facilities and services is likely to become more complex and wide spread in future due to economic imperatives and will work in favour of nonaffluent countries.
Conclusions
The objective of cardiac surgeons remains to take the best care to all their patients. The need is to become once again the masters to control the technology and to guide the industry rather then be led by this combine. It will be a sign of maturity of cardiac surgeons to establish national standards of care and treatment and compare these with the emerging data from different parts of the world. Such differing standards will reflect the ground realities.
In the evolving epidemic of cardiovascular disease in developing countries, most of the global cardiovascular disease burden shifts to the nonaffluent countries. Thus, the language of activist cardiac care needs to be universal, irrespective of the locale where the care is delivered. We hope that emergence of comprehensive algorithms of universal appropriateness of patient selection and adequacy of equivalent technology of treatment options would lead to growth of more centers all over the world to make the benefits of equivalent activist cardiac care accessible to millions more of people.
References
- Unger F, Ghosh P. International cardiac surgery. Semin Thorac Cardiovasc Surg 2002;14:321-323.
- Pezzella AT. International cardiac surgery. Ann Thorac Surg 1998;65:903-904.
- Cox JL. Changing boundaries. J Thorac Cardiovasc Surg. 2001;122:413-418.
- Hart JT. The inverse care law. Lancet 1971;1:405-412.
- Ghosh P, Unger F. Cardiac activist care. Cardiac surgery and catheter based procedures in Europe in 1998. Cor Europaeum 2000;8:128-138.
- Brook RH, Kosecoff JB, Park RE, Chassin MR, Winslow CM, Hampton JR. Diagnosis and treatment of coronary disease: comparison of doctors' attitudes in the USA and the UK. Lancet 1988;1:750-753.
- Fitch K, Lázaro P, Aguilar MD, Kahan JP, van het Loo M, Bernstein SJ. European criteria for the appropriateness and necessity of coronary revascularization procedures. Eur J Cardio-thorac Surg 2000;18:380-387.
- Barakate MS, Hemli JM, Hughes CF, Bannon PG, Horton MD. Coronary artery bypass grafting (CABG) after initially successful percutaneous transluminal angioplasty (PTCA):a review of 17 years experience. Eur J Cardiothorac Surg 2003; 23:179-186.
- Vijaykumar M, Narula J, Reddy KS, Kaplan EL. Incidence of rheumatic fever and prevalence of rheumatic heart disease in India. Int J Cardiol 1994;43:221-8.
- Magotra RA, Kasar NK, Mall SP. Close versus open approach to mitral stenosis. An objective analysis. Ind Heart J 1987;39:60-64.
- Ghosh P. Changing Trends in valve surgery in Europe:1991-2000. J. Heart Valve Dis 2004;13:1-10.