ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Cardiac Tamponade Due to a Strangulated Visceral Pericardial Hernia After Convergent Procedure
Bloom JP, Tolis, Jr. G, Birkett RT, Rosenblatt MS, Fitton TP. Cardiac Tamponade Due to a Strangulated Visceral Pericardial Hernia After Convergent Procedure. October 2019. doi:10.25373/ctsnet.9934208.
A 74-year-old man with persistent atrial fibrillation, severe tricuspid regurgitation (TR), and pulmonary hypertension underwent a convergent procedure (CP). The CP is a closed chest, transdiaphragmatic laparoscopic hybrid epi- and endocardial ablation procedure for the treatment of complex atrial fibrillation that has been shown to be safe and effective (1). To gain access to the epicardium, the abdomen was insufflated and a subcentimeter incision was made in the central tendon of the diaphragm medial to the falciform ligament, one centimeter superior to the left hepatic lobe. A pericardioscopy cannula was subsequently advanced into the pericardial well. The coronary sinus and left and right inferior pulmonary veins were identified and transmural lesions were performed across the posterior left atrial wall and anterior surface of the left inferior pulmonary vein. After the surgical portion, a 19 French Blake drain was left in the pericardial well prior to cannula removal. A full endocardial ablation procedure was then performed via traditional percutaneous femoral access during the same operative setting.
There were no postoperative complications and the patient was discharged home on postoperative day three on dofetilide and warfarin. To date, the patient remains in sinus rhythm with near-resolution of his tricuspid regurgitation and normalization of his right ventricular function and diameter and pulmonary arterial pressures. Both the anti-arrhythmic and anti-coagulation medications were discontinued.
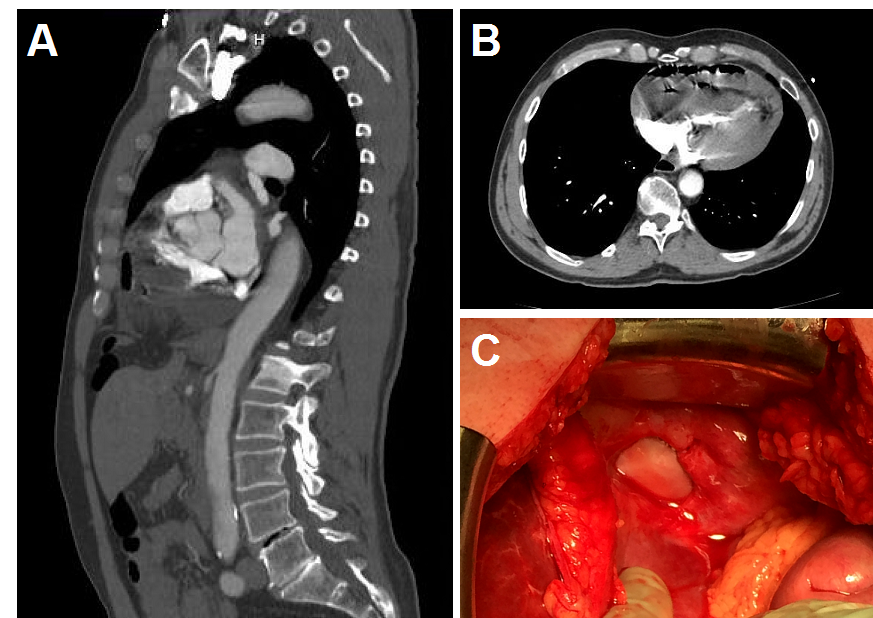
Figure 1. (A) Sagittal CT image showing diaphragmatic defect with small bowl herniated into the pericardium. (B) Axial CT image showing intrapericardial loop of small bowel compressing the chambers of the heart causing cardiac tamponade. (C) Photographic image of the defect in the diaphragm after reduction of intestinal contents.
Two and a half years later, the patient presented with acute onset of severe epigastric pain and associated nausea and vomiting. Concern for possible aortic dissection prompted a computed tomography angiogram of the chest, which revealed the small bowel herniated through the diaphragmatic defect with ventricular compression. Although initially stable, the patient became hemodynamically unstable during transfer and on arrival was on multiple vasopressors. His abdomen was rigid with peritoneal rebound tenderness. Initial laboratory evaluation revealed an arterial pH of 7.04 with a base deficit of 17, an anion gap of 21, and lactate of 8.4. He was taken emergently to the operating room for exploratory laparotomy. Reduction of the herniated small bowel through the diaphragmatic defect from the CP resulted in immediate restoration of normal hemodynamics. A 20 cm in length of infarcted jejunum was resected and primarily reconstructed. The 2 cm defect in the central tendon of the diaphragm could not be approximated primarily due to tension. Because of the potential contamination from the infarcted small bowel, the falciform ligament was secured in a circumferential fashion over the defect with a running 2-0 Prolene® suture. The patient did well postoperatively and was discharged home six days later.
Cardiac tamponade is a life-threatening problem characterized by an increase in pericardial pressure and the classic Beck’s triad of muffled heart sounds, hypotension, and elevated jugular venous distension. The hallmark feature on the electrocardiogram is electrical alternans, and a pulsus paradoxus is typically appreciated. In the unstable patient, treatment typically requires emergent pericardiocentesis or open drainage with a pericardial window. Mortality approaches 100% if unrecognized, thus early diagnosis and intervention are key to survival.
The CP has been shown to be a safe and effective treatment method for atrial fibrillation in patients who have failed conventional endocardial ablation therapy. This procedure particularly benefits patients who do not warrant other open cardiac surgical intervention and/or who cannot tolerate single-lung ventilation. Long-term restoration of sinus rhythm is present in 46-84% of cases. Historically, the diaphragmatic defect was left unclosed after the case to facilitate the egress of blood should a perforation occur during the electrophysiology ablation portion of the procedure.
This is the third case report of a patient with a pericardial hernia after the CP (2, 3). While there are similarities to the prior case reports, this is the first where a patient presented with acute life-threatening cardiac tamponade. This patient had a remarkable outcome after his CP with near complete resolution of his tricuspid regurgitation, pulmonary hypertension, and right ventricular dilation. Moreover, he was liberated from anti-arrhythmics, long-term systemic anticoagulation, and the associated complications of thromboembolisms. Unfortunately, almost 2 1/2 years later he suffered a terrible complication that resulted from an iatrogenic defect in the diaphragm. This report highlights a typical dilemma in surgery, where procedures that provide a vital therapeutic benefit to patients can have unintended serious consequences, and further highlights the importance of careful patient selection for invasive procedures and the importance of clinical history for guiding diagnosis.
Since this case, the authors have changed their surgical approach for CP to a transxiphoid method obviating the need for a transdiaphragmatic incision, and, in cases that they use a transdiaphragmatic approach, they are now closing the diaphragm defect around the Blake drain.
References
- Geršak B, Zembala MO, Müller D, Folliguet T, Jan M, Kowalski O, et al. European experience of the convergent atrial fibrillation procedure: multicenter outcomes in consecutive patients. J Thorac Cardiovasc Surg. 2014;147:1411–1416.
- Shrestha S, John J, Jacobowitz I, Greenberg Y, Yang F. Pericardial hernia: an unusual complication of convergent atrial fibrillation ablation. Oxf Med Case Reports. 2016;5:107–108.
- Kaufman AJ, Kahn ET, Villena-Vargas J, Steele JG, Flores RM. Laparoscopic repair of an intrapericardial diaphragmatic hernia after convergent Maze procedure. Ann Thorac Surg. 2017;103(6):e541-e543.




