ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Concomitant Closure of Atrial Septal Defect and Correction of Pectus Excavatum
Yuksel, Mustafa; Arslan, Didem Gungor; Ermerak, Onur; Yanartas, Mehmet; Yildizeli, Bedrettin (2017): Concomitant Closure of Atrial Septal Defect and Correction of Pectus Excavatum.
CTSNet, Inc.. https://doi.org/10.25373/ctsnet.5239561
Retrieved: 20:34, Jul 26, 2017 (GMT)
Introduction
Holt-Oram Syndrome (HOS) is characterized by skeletal abnormalities of the hands and arms, and heart problems. It is estimated to affect 1 in 100,000 individuals (1). People with HOS have abnormally developed bones in their upper limbs. They also may have additional bone abnormalities including a missing thumb, a long thumb that looks like a finger, partial or complete absence of the radius or ulna, an underdeveloped humerus, and abnormalities of the clavicle or scapula. About 75% of individuals with HOS have congenital cardiac problems that can be life-threatening (2). The most common problems include atrial and ventricular septal defects (ASD and VSD, respectively) (3).
In the normal population, the frequency of pectus excavatum is 300 to 400 in 1,000 live births, but it is much higher in individuals with HOS (4). Since ASD is the most common (60%) cardiac problem in HOS, coexistence of pectus excavatum and ASD is not uncommon.
Case Presentation
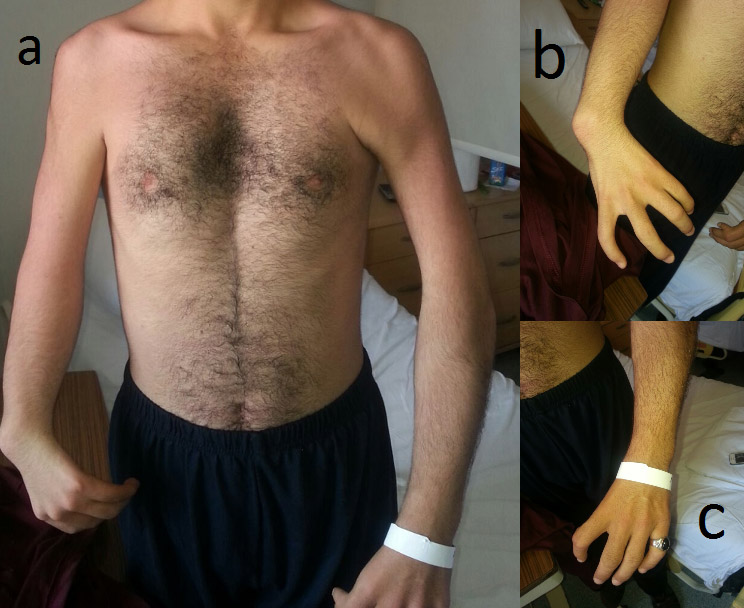
A 20-year-old male patient presented with HOS. He had no thumb on either hand and a pectus excavatum deformity (Figure 1). An ASD and mild aortic valve insufficiency were observed on echocardiography. Surgery was indicated due to substantial shunting, which may lead to volume overload of the right atrium, right ventricle, and pulmonary arteries.
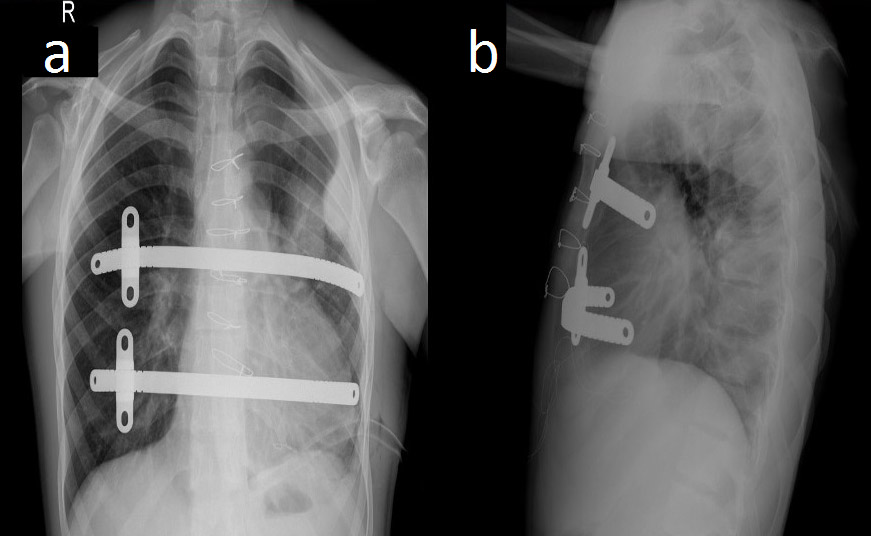
Figure 2. Postoperative chest radiographs showing the bar positions in anteroposterior (a) and lateral (b) projections.
The authors decided to perform synchronous ASD closure and correction of the pectus excavatum deformity. The patient was placed in the supine position with the arms abducted to expose the anterior and lateral chest wall. The deepest point and the bilateral highest points (thoracic entry and exit points) of the thorax were marked. Two bars were used to correct the deformity. In total, four skin incisions were made: in the third intercostal space on the left side, in the fourth intercostal space in the anterior axillary line, in the third intercostal space on the right side, and the fourth intercostal space in the anterior axillary line on the right side. Subcutaneous pockets (two left and two right) were made by blunt dissection, and a median sternotomy was performed. The introducer was slowly advanced across the anterior mediastinal space immediately under the sternotomy. Using the introducer, a strand of cloth tape was pulled through the tunnel. The tape functioned as a guide for placement of the pectus bars, and then the pericardium was opened. The patient was put on cardiopulmonary bypass, the superior and inferior vena cavae were clamped, and the aorta was clamped. Cardioplegia was administered. The ASD was closed with a pericardial patch and cardiopulmonary bypass was terminated. Sternal wires were placed for sternal closure, but were not twisted. The introducers were linked to the tape and two bars were inserted with the convexity facing posteriorly, and the sternal wires were twisted. A bar flipper was used to turn the two bars over while pulling up the sternum. The rotated bars were fixed with butterfly stabilization on the right sides of the chest, and were fixed with PDS sutures on the left side (Figure 2). There was no need to use a thoracoscope, because the authors were able to see the procedure under direct vision through the sternotomy. The incisions were closed and the patient was taken to the cardiac intensive care unit with a mediastinal and two thoracic (left and right) chest tubes.
The patient was extubated six hours postoperatively, taken to the regular hospital unit on the first postoperatıve day, and discharged to home on the eighth postoperative day. After one year, the wound healing was perfect (Figure 3).
Comment
The concomitant presence of chest wall deformities, such as pectus excavatum, and cardiac abnormalities that necessitate surgical intervention creates a conflict for surgeons. In adults, concomitant scheduled surgery is reliable and offers excellent long-term cosmetic results (5). Moreover, it allows a better thoracic exposition with no added perioperative risk.
The authors' approach for the simultaneous repair of ASD and pectus excavatum has proven to be safe and satisfactory. The technique uses a vertical midline sternotomy, so there is no need to use a thoracoscope. This combined procedure also allows excellent exposure for the correction of ASD, and is much safer for inserting the trocar and steel bars, which are situated under direct vision through the sternotomy.
The majority of reports and review articles regarding this combination of problems have focused on infants and children. Reports of simultaneous repair in adults are rare. Okay and colleagues reported on four adult patients who underwent simultaneous operations based on a modified Ravitch procedure (6). Okamura and colleagues reported the case of a 47-year-old woman who had a concomitant pectus excavatum and atrial septal defect repair using a combination of the Ravitch procedure (ie, transverse sternal osteotomy and excision of costal cartilages) and the minimally invasive procedure, popularized by Nuss, using the convex bar (5). In this case, none of the additional procedures of costal cartilage excision were performed, so that pain relief could be easier and the operation shorter. Only one example of our concomitant surgical procedure is reported by Kao and colleagues in a 25-year-old man with pectus excavatum and ASD corrected by sternotomy and Nuss procedure, but in that case a single bar was used (7). Similar excellent outcomes were described.
In conclusion, concomitant pectus deformity correction and open heart surgery can be performed safely, eliminating the risks of a second operation in a staged procedure. Correction of pectus deformity in this setting using a minimally invasive Nuss procedure is feasible and straightforward.
References
- Csaba E, Marta V, Endre C. Holt-Oram syndrome. Orv Hetil. 1991;132:73-78.
- Basson CT, Huang T, Lin RC and et al. Different TBX5 interactions in heart and limb defined by Holt-Oram syndrome mutations. Proc Natl Acad Sci USA. 1999;96:2919-2924.
- Basson CT, Bachinsky DR, Lin RC and et al. Mutations in human TBX5 (corrected) cause limb and cardiac malformation in Holt Oram syndrome. Nat Genet. 1997;15:30-35.
- Saxena AK, Schaarschmidt K, Schleef J, Morcate JJ, Willital GH. Surgical correction of pectus excavatum: the Munster experience. Langenbecks Arch Surg. 1999;384:187-193.
- Okamura T, Nagase Y, Mitsui F, Shibairi M, Utsumi K, Watanabe H. Simultaneous repair of pectus excavatum and congenital heart defect in adults by using the convex bar. Ann Thorac Surg. 2004;77:1827-1829.
- Okay T, Ketenci B, Imamoglu OU and et al. Simultaneous open-heart surgery and pectus deformity correction. Surg Today. 2008;38:592-596.
- Kao CH, Tsai CS, Huang TW, Lee SC, ChengYL. The Nuss procedure for pectus excavatum at the time of atrial septal closure. Ann Thorac Surg. 2010;89:985-986.