ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Hilum First-Fissure Last Biportal VATS Right Lower Lobectomy for Lung Cancer
Gherzi L, Ferrari M, Pardolesi A. Hilum First-Fissure Last Biportal VATS Right Lower Lobectomy for Lung Cancer. August 2022. doi:10.25373/ctsnet.20457117.v1
Anatomic lung resection is the gold standard procedure for the treatment of primary non-small cell lung cancer (1).
The division of the interlobar fissure may represent a critical step when performing lower lobectomies. The presence of an incomplete or partially incomplete fissure may result in a prolonged dissection of the parenchyma. The identification of the interlobar pulmonary artery can also be more challenging as a result. This effectively leads to a higher risk of prolonged air leak in the postoperative time (2).
To date, there is no unanimous consensus to assess and define the completeness of the lung fissures. Craig et al. in 1997 (3) proposed a four-stages classification based on both the degree of completeness of the fissures and the location of the pulmonary artery at the base of the oblique fissure. More recently, Schieman and his colleagues modified Craig’s scale to create an intuitive, simple, and reproducible grading system that could be used by surgeons and radiologists in the preoperative work up (Table 1) (4).
|
Grade |
Surgical Identification | Radiologic Identificaiton |
|---|---|---|
| 1 | Entirely separate pulmonary lobes | Fissure extended to the hilum medially along all cuts |
| 2 | Complete visceral cleft with an exposed pulmonary artery at the base and some parenchymal fusion | Fissure extended to the artery medially, but not along the hilum along all cuts (including instances when the fissure line could not be clearly seen or seemed to terminate in the lung tissue without extending entirely to the pulmonary artery medially) |
| 3 | A visceral cleft only evident for part of the fissure without a visible pulmonary artery | Fissure extended into the lung for a distance and terminated before reaching the pulmonary artery |
| 4 | Absent fissure | No visible fissure line |
This video presents the surgical technique to perform video-assisted “hilum first–fissure last” right lower lobectomy with a two-port approach in a seventy-five-year-old female nonsmoker. The woman was admitted to an institution with a diagnosis of a 32 mm right lower lobe adenocarcinoma. The preoperative chest computerized tomography (CT) scan displayed the presence of a partially incomplete fissure. The completeness of the interlobar fissure was given the grade of 3, according to the Craig’s scale classification (Figure 1).

Figure 1: Incomplete major fissure (grade 3) showed in axial and coronal planes on preoperative CT scan.
Patient Selection
Any patient selected for VATS lobectomy, in which incomplete fissure is recognized preoperatively or intraoperatively, is eligible for the fissureless technique through the anterior approach.
According to ESMO Guidelines, “VATS should be the approach of choice in stage I tumors.” Moreover, the National Comprehensive Cancer Network (NCCN) Guidelines for NSCLC recommend that, “VATS should be strongly considered for patients with no anatomic or surgical contraindications, as long as there is no compromise of standard oncologic and dissection principles of thoracic surgery” (5).
Therefore, minimally invasive thoracic surgery could be consistently applied, and only anatomical or oncological intraoperative conditions such as impossible single lung ventilation, strong adhesions, tumor or lymph nodes dimension, and incomplete fissure might represent a relative contraindication to the procedure (6).
Preference Card
-
30-degree 10 mm endoscopic camera
-
Tissue retractor: Alexis® wound protector-retractors (Applied Medical, California, US)
-
Usual 5 mm endoscopic instruments (grasping forceps, dissectors, scissors, suction)
-
Endoscopic staplers: Endo GIA™ (Covidien-Medtronic, Dublin, Ireland) or Echelon Flex™ (Ethicon-Johnson & Johnson, New Jersey, US)
-
Energy devices: Harmonic Ace® (Ethicon-Johnson & Johnson, New Jersey, US) or Maryland LigaSure™ (Medtronic, Dublin, Ireland)
-
Endoscopic retrieval bag
Operative Steps
The procedure was performed under general anesthesia with double-lumen intubation. The patient was placed in left lateral decubitus, with the patient's hip that should be positioned at the level of the table break, to allow maximum separation of the intercostal spaces. The right arm should be placed between two pillows to improve the patient’s stability and reduce conflict with surgical tools. The surgeon then stands in front of the patient (Figure 2), with the scope normally held by the assistant surgeon who stands on his/her left.
The procedure was started by performing a roughly 4 cm utility incision, protected by a tissue retractor (Alexis®) at the level of the fifth intercostal space along an imaginary line between the tip of the scapula and the nipple. Then the subsequent 10 mm camera trocar was placed under direct vision, two intercostal spaces below the utility incision on the anterior axillary line.
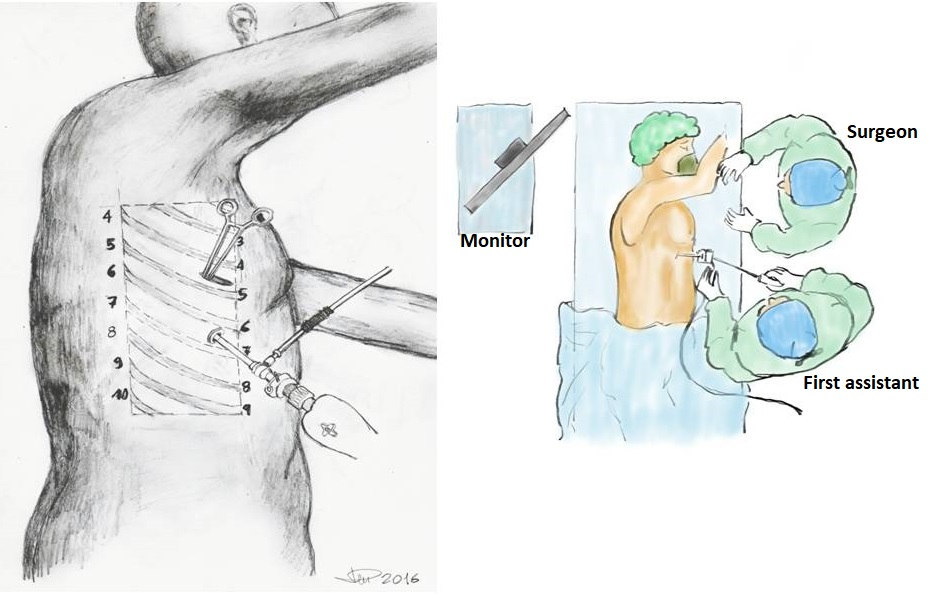
Figure 2: Position of the surgeon in front of the patient and port placement for a thoracoscopic right lower lobectomy.
Step 1: Division of the Pulmonary Ligament
The first step consisted of freeing the lung dividing the inferior pulmonary ligament. The lung was gently pulled backward using a lung clamp (i.e., a Duval clamp), thus allowing the exposure of the triangular ligament. The ligament was incised with the Harmonic Ace up to the border of the inferior pulmonary vein. The energy device, used cooperatively with gentle traction on the lower lobe, eased the maneuver (Figure 3A). Station 9 lymphadenectomy was performed in this phase (Figure 3B).
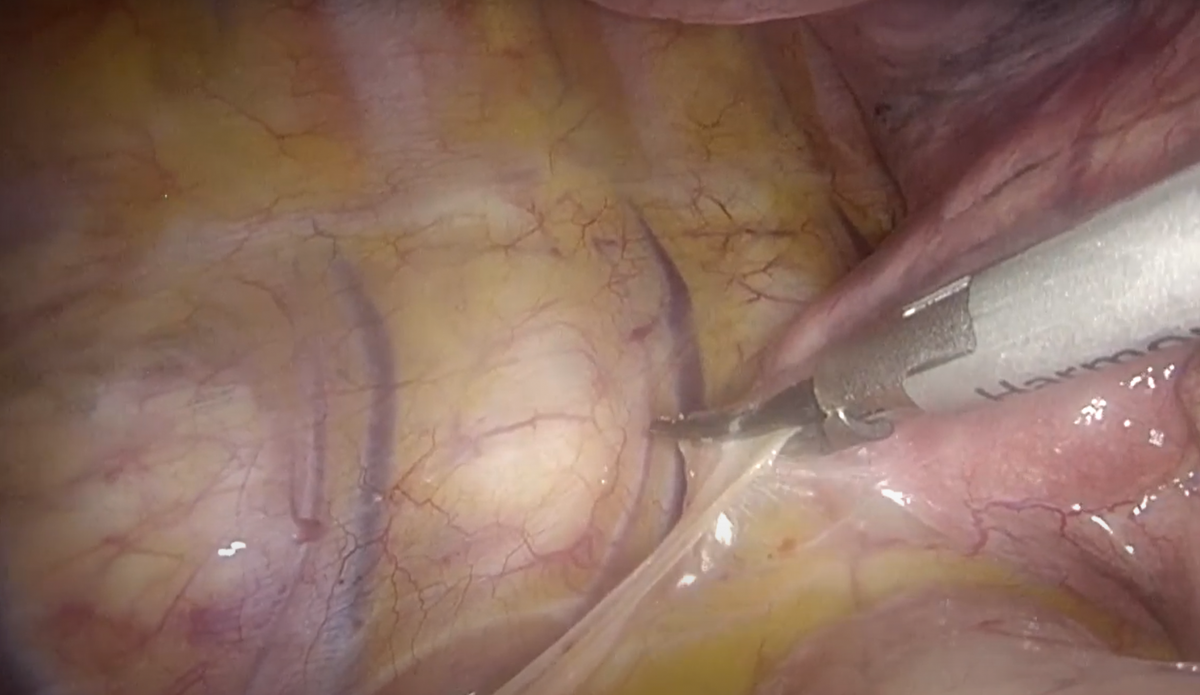
Figure 3A: Division of the pulmonary ligament with the energy device combined with gentle upward traction of the lower lobe.
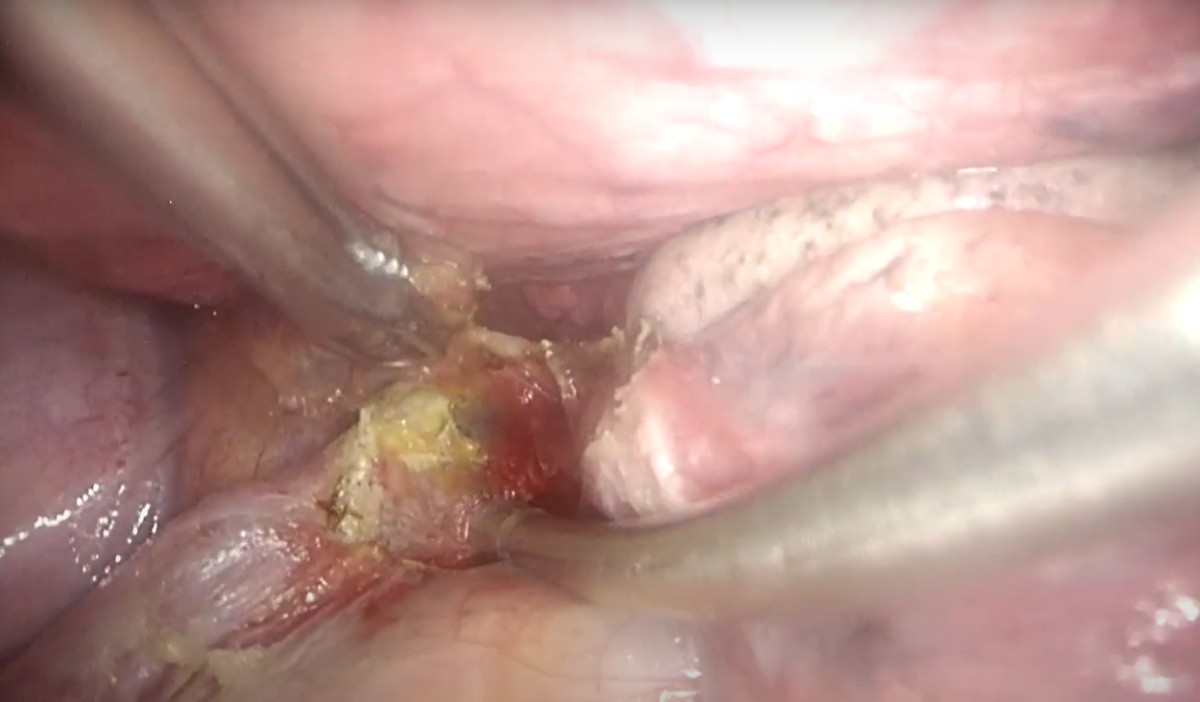
Figure 3B: Station 9 lymph node lies within the pulmonary ligament and can be easily harvested at this time of the procedure with blunt dissection and coagulation.
Step 2: Isolation and Division of the Right Inferior Pulmonary Vein
Once the inferior pulmonary vein was visualized, the dissection was extended anteriorly and posteriorly to open the mediastinal pleura around the hilum and to expose and identify the middle and superior pulmonary veins.
After confirming normal venous anatomy, the inferior pulmonary vein was isolated and dissected using a 30 mm Endo GIA with a gold vascular load. The stapler was introduced through the utility incision in a top-to-bottom direction, which ensures the tip of the instrument does not push on other vessels (Figure 4).
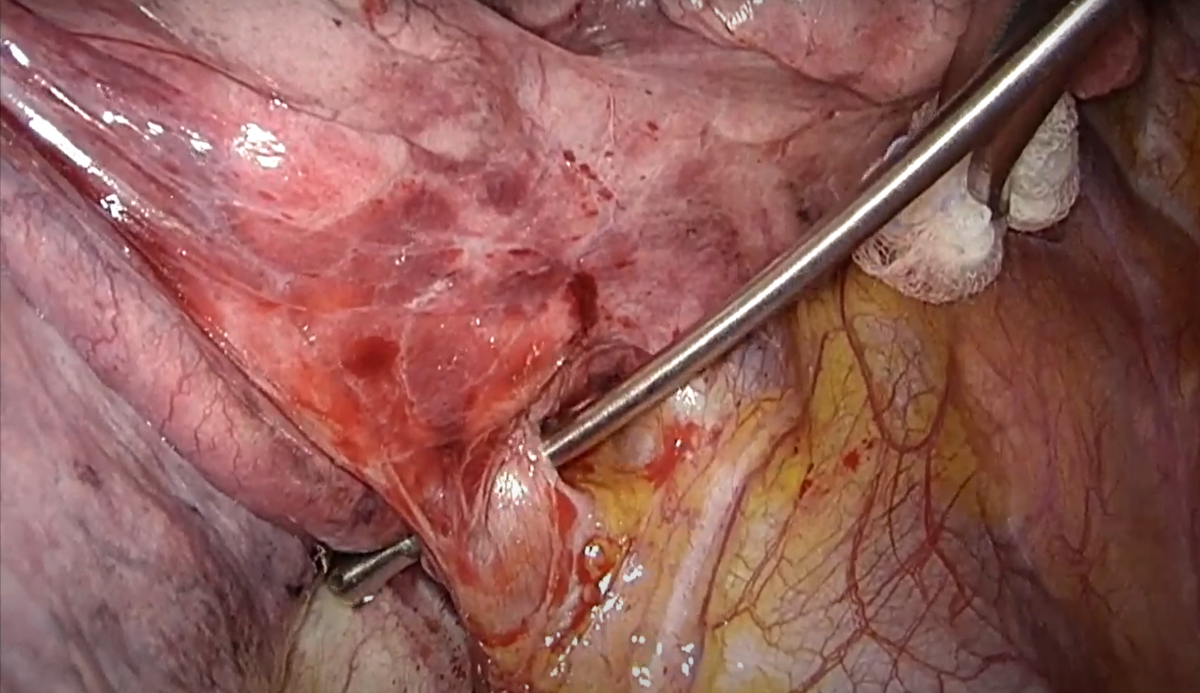
Figure 4A: Isolation of the inferior pulmonary vein.
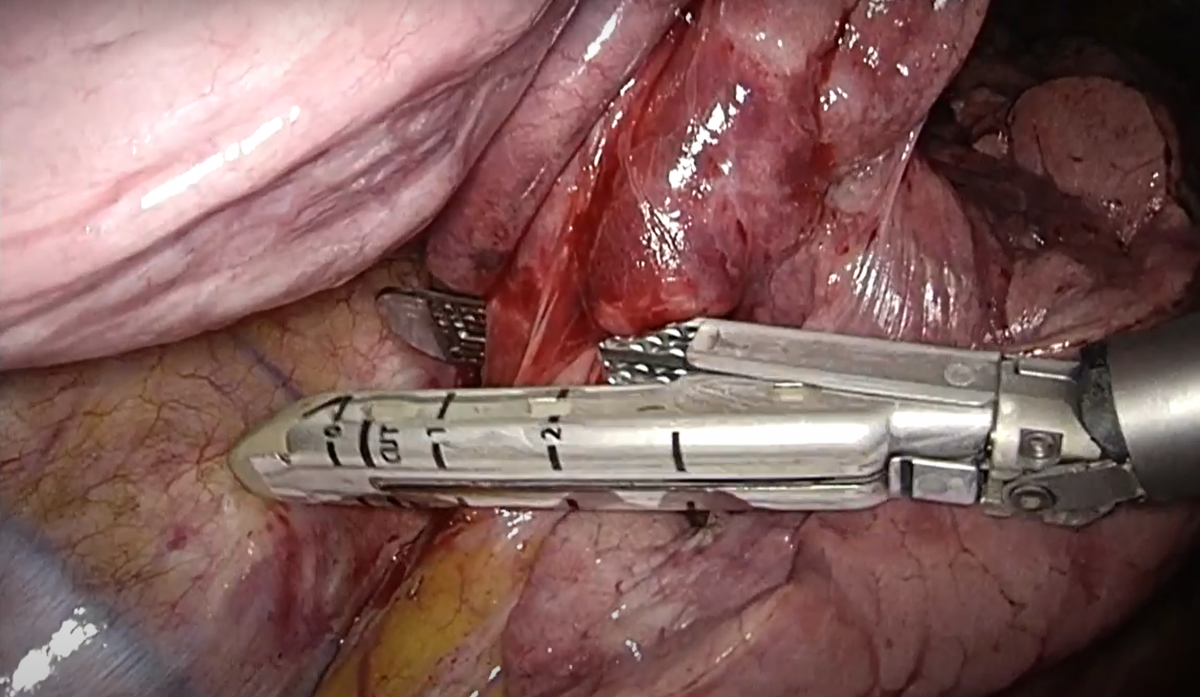
Figure 4B: Dissection of the inferior pulmonary vein with a vascular 30 mm gold Endo GIA.
Step 3: Isolation and Division of the Bronchus
The lower lobe bronchus lies just above the vein. The bronchus was approached from the posterior view, tilting the lung anteriorly and upward. All surrounding tissues of the anterior, inferior, and superior aspects of the bronchus were cleared with blunt dissection or with the help of a small gauze mounted on a clamp. Interlobar lymph nodes could have been excised with the help of the Harmonic Ace. It is critical to properly identify the middle lobe bronchus and the lower lobe apical segment.
Isolation of the bronchus should be carried out carefully and gently, avoiding injuries to the pulmonary artery that is located just above the bronchus.
As before, the stapler with a 30 mm or 45 mm load was introduced through the utility incision and slid around the bronchus in a front-to-back direction, taking care to push the parenchyma upward to have better vision of the rear aspect of the bronchus (Figure 5).
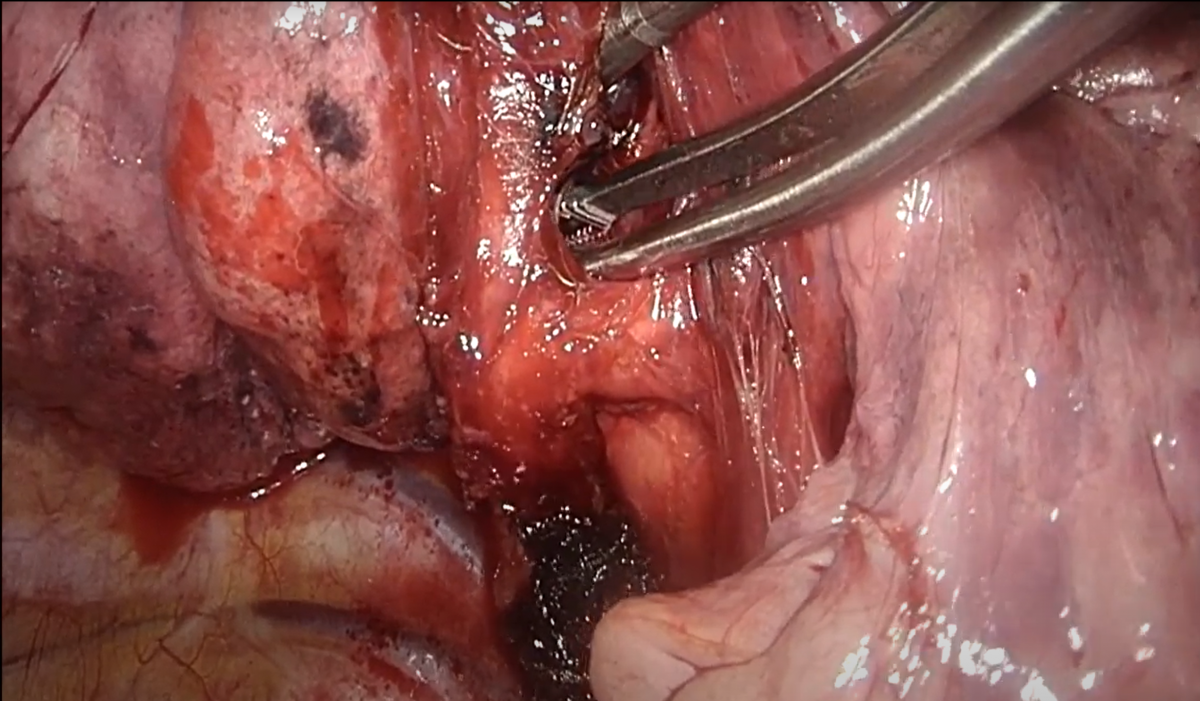
Figure 5A: Relations between lower and middle lobe bronchi and pulmonary artery.
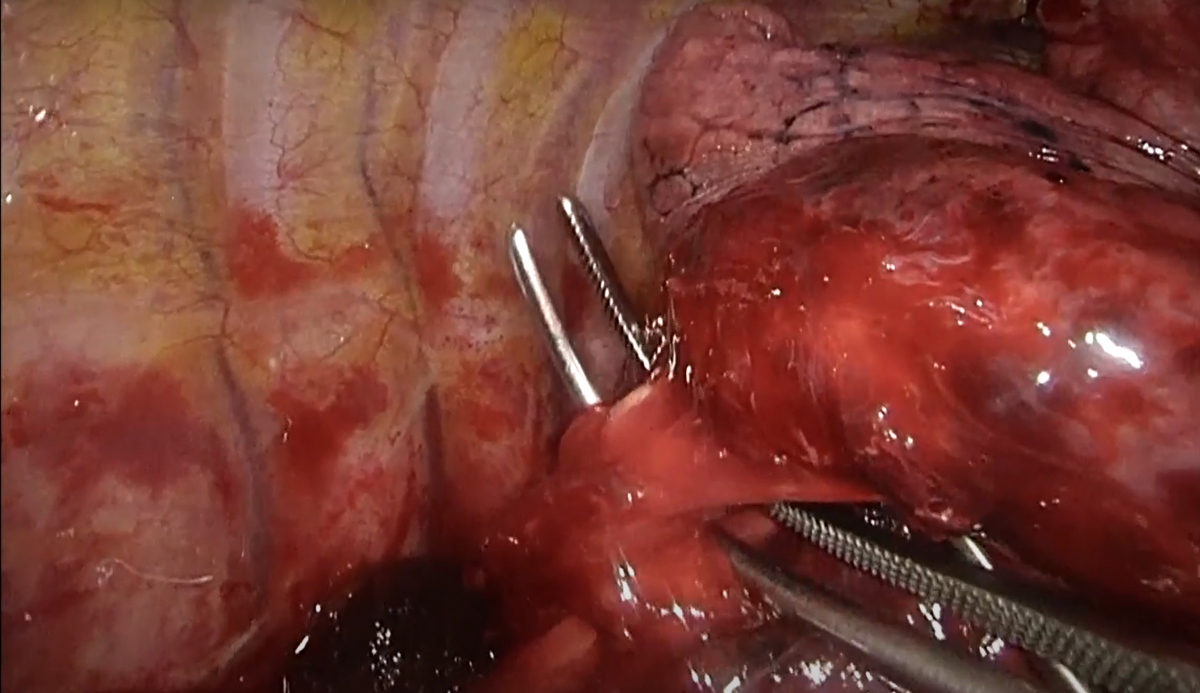
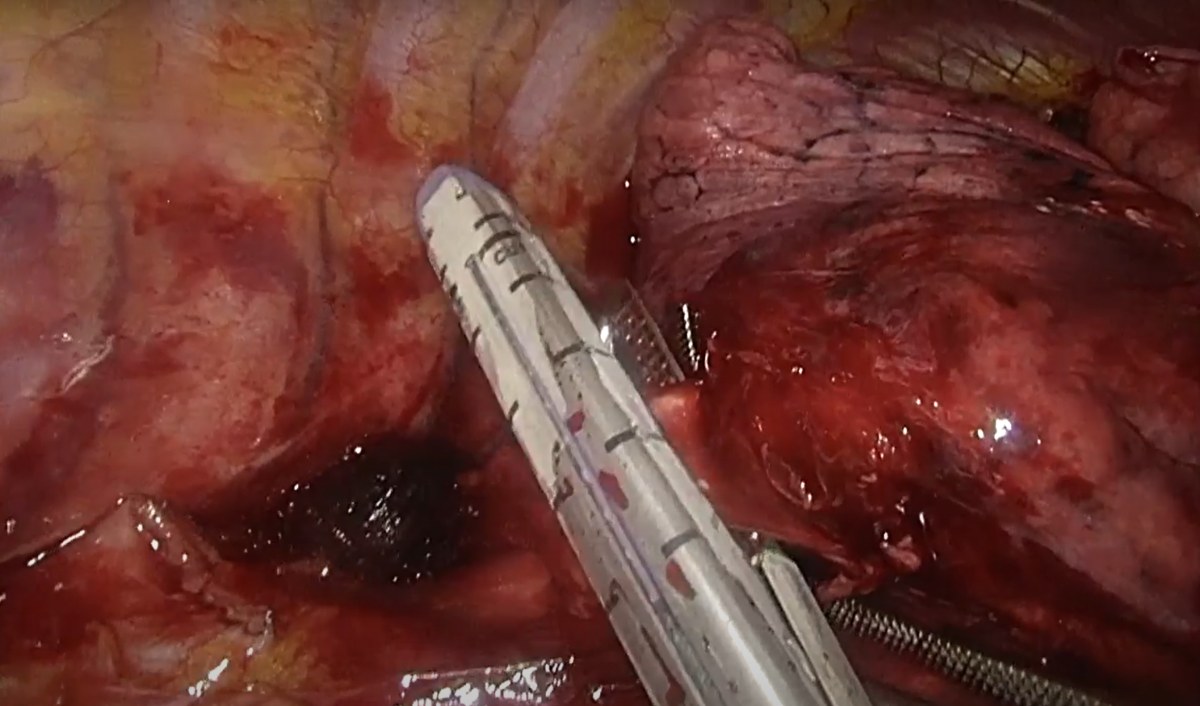
Figure 5BC: The lower lobe bronchus is isolated with a curved clamp and divided with a violet 45 mm Endo GIA after the re-expansion maneuver.
Step 4: Isolation and Division of the Artery
Once the bronchus has been divided, the artery should be identified just above the bronchial stump. The surrounding tissues were cleared with blunt dissection of the suction instrument and then isolated with a curved dissector on a vessel loop (Figure 6A). Attention must be paid to properly identify the S6 segment artery (Figure 6B). Lastly, the artery was stapled with a gold 30 mm Endo GIA in the same manner as the bronchus (Figure 6C).
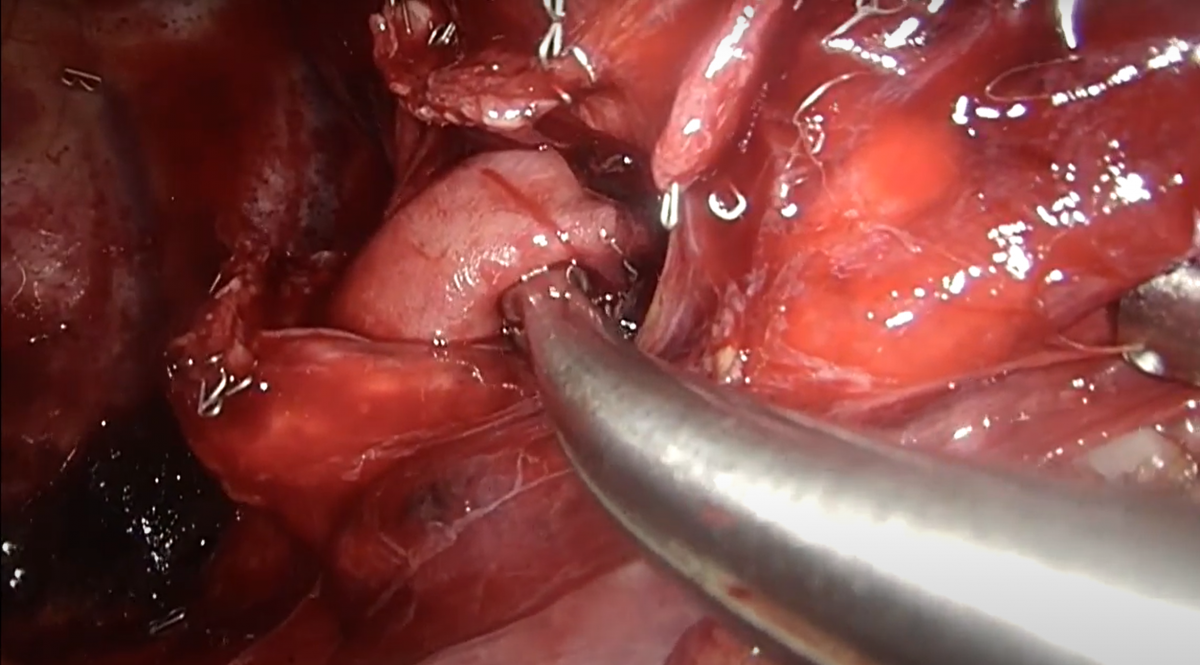
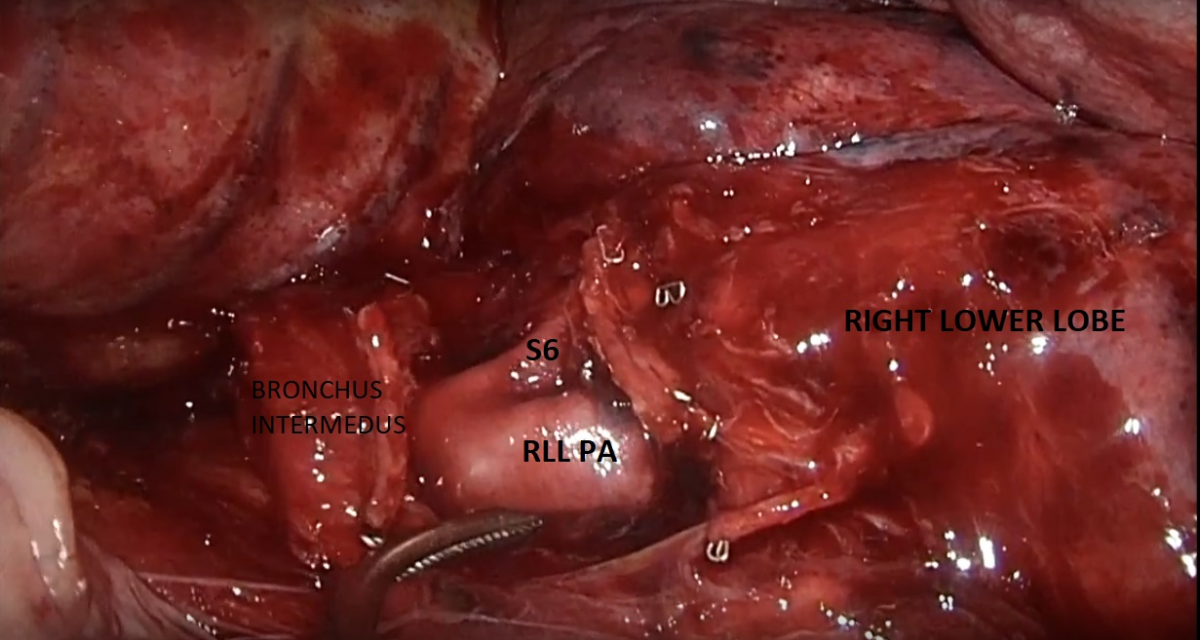
Figure 6AB: The lower lobe artery is identified and cleared with attention of S6 segment branch.
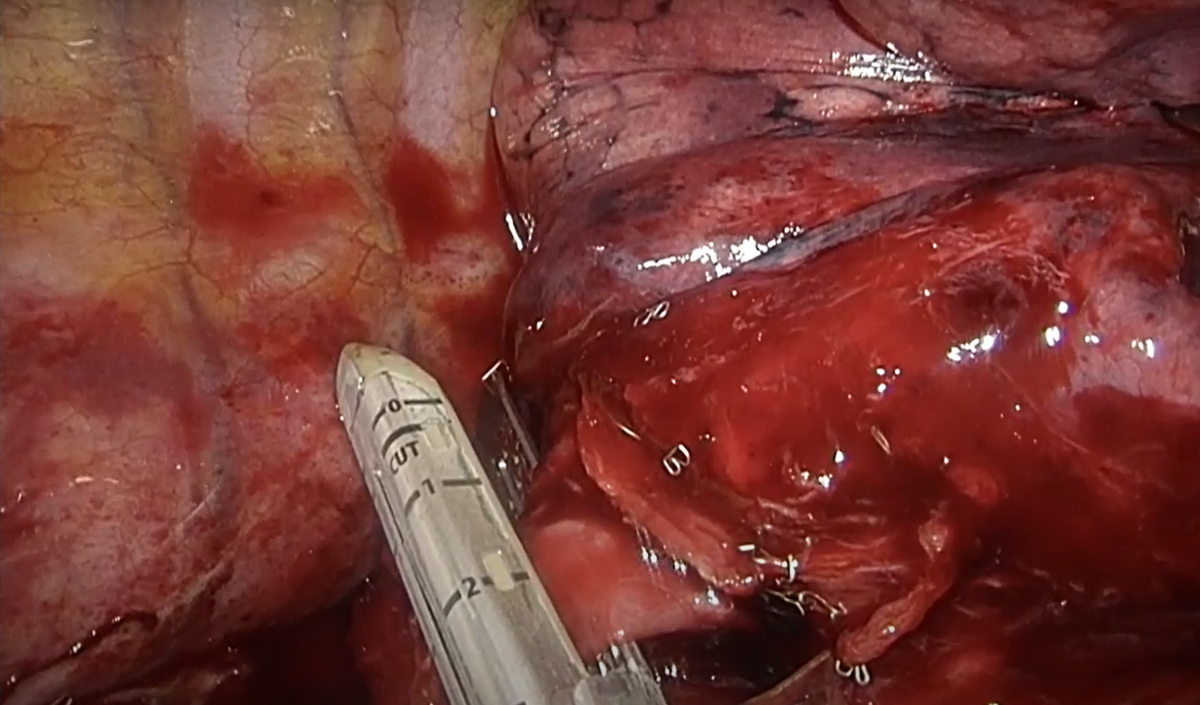
Figure 6C: The artery is divided with a gold 30 mm Endo GIA.
Step 5: Division of the Oblique Fissure
The fissure was eventually divided starting from the anterior aspect with one to three cartridges, keeping the interlobar pulmonary artery stump under direct view. Then the posterior part was easily stapled, taking care to place the anvil of the stapler just above the pulmonary artery (Figure 7).
The lobe was then pulled out of the chest through a specimen retrieval bag.
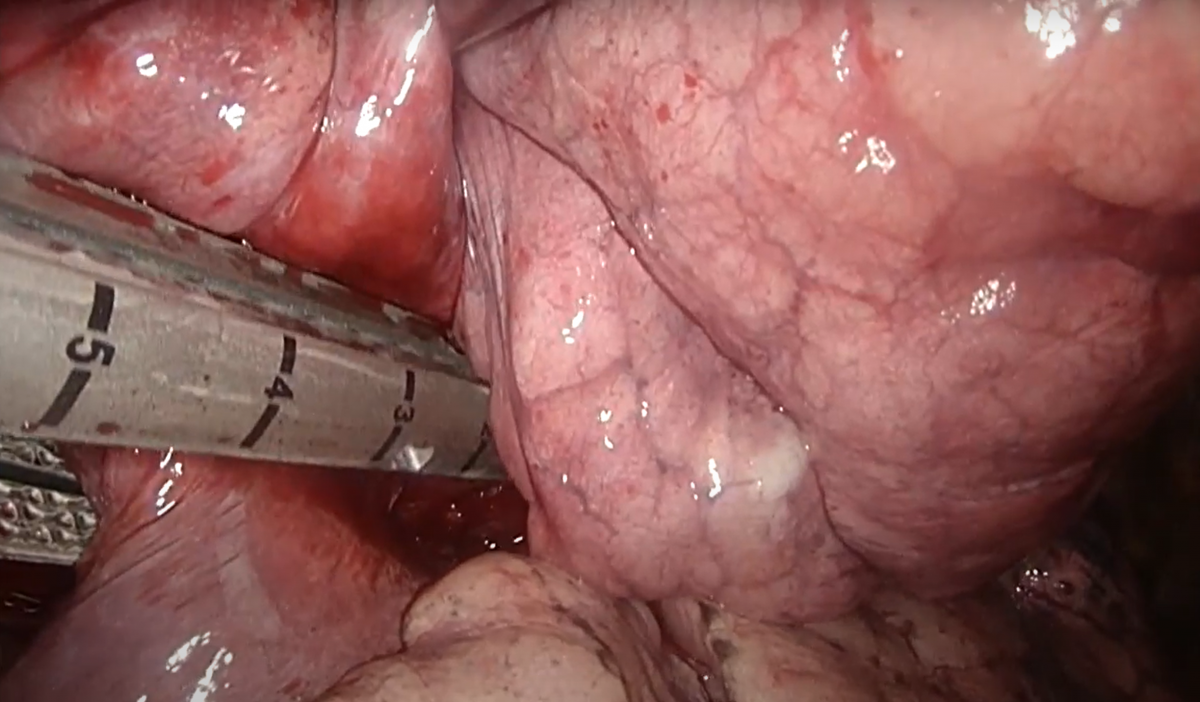
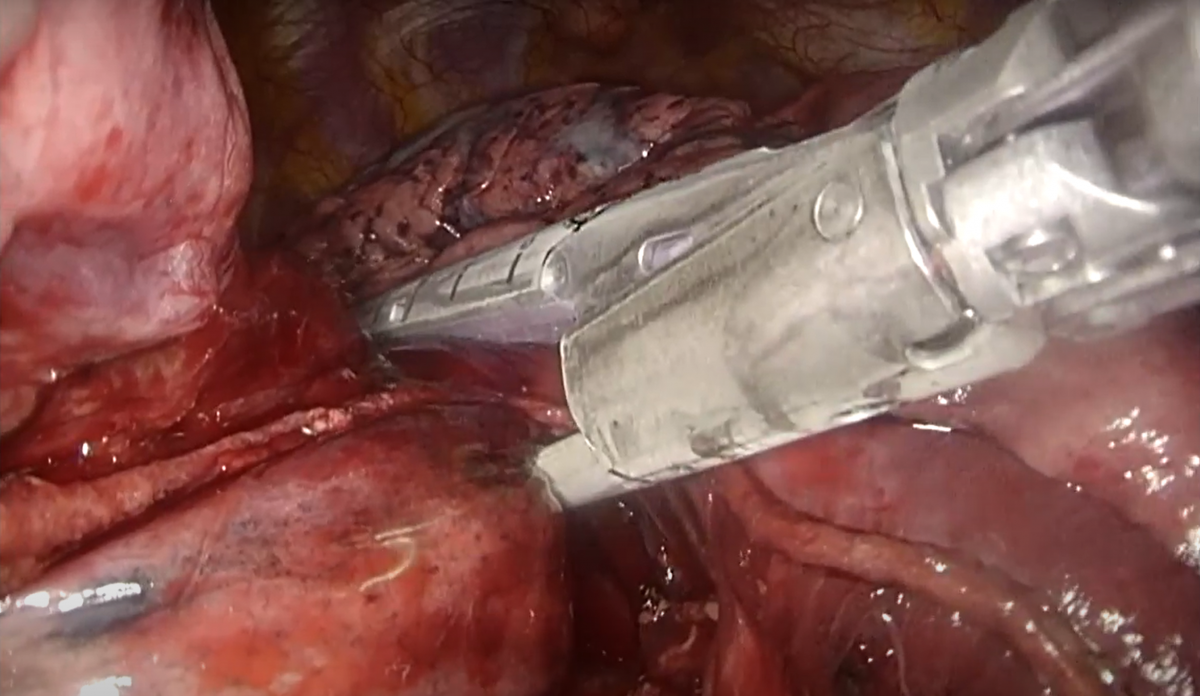
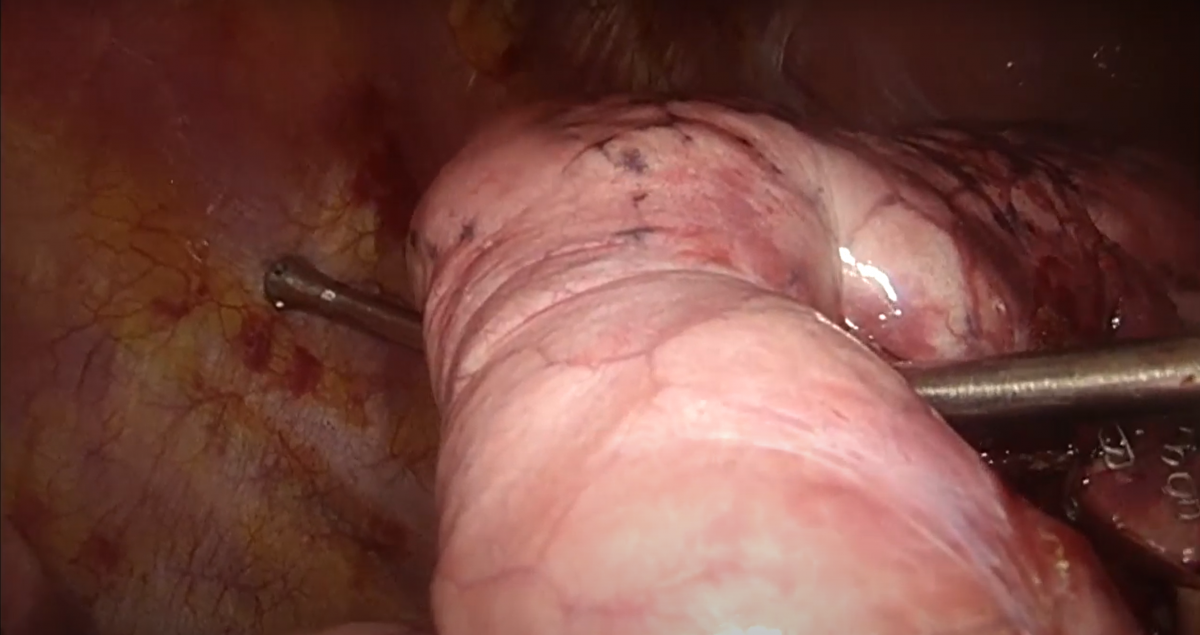
Figure 7: The fissure is completed with multiple cartridges of parenchymal 45 and 60 mm Endo GIA.
Tips and Pitfalls
-
When performing a fissure-last right lower lobectomy, the middle lobe bronchus can be easily twisted or narrowed when the stapler is slid around the lower lobe bronchus compared to standard procedures. We suggest creating a path for the stapler by placing a suction instrument or a right-angle clamp around the lower lobe bronchus. This “trick” may aid in sliding the stapler more easily, avoiding injury to the pulmonary artery and the middle lobe bronchus.
-
Identification of the lower lobe apical segment artery (A6) is a crucial step in avoiding vascular injuries. Usually the A6 origins at the same level of the middle lobe artery. Sometimes it may arise higher and more posteriorly. In this situation, dividing the A6 separately from the basal trunk is recommended.
Comments
The anterior approach for VATS lobectomies described by Hansen and colleagues (7) has the advantage of providing a standardized technique with low conversion rates, adaptable by many surgeons familiar with an open approach.
The operative steps described for the right lower lobe show that the hilum is approached from the bottom to the top, starting with the pulmonary vein, then the bronchus, and eventually the artery. This can be done without the need to dissect the fissure, effectively reducing the risk of postoperative complications.
This approach is almost feasible in every case. It can be applied in a reproducible manner, especially when the fissure is completely absent.
References
- Deboever N, Mitchell KG, Feldman HA, Cascone T, Sepesi B. Current surgical indications for non-small-cell lung cancer. Cancers (Basel). 2022;14(5):1263. doi:10.3390/cancers14051263
- Gómez-Caro A, Calvo MJR, Lanzas JT, Chau R, Cascales P, Parrilla P. The approach of fused fissures with fissureless technique decreases the incidence of persistent air leak after lobectomy. Eur J Cardiothorac Surg. 2007;31(2):203-208. doi:10.1016/j.ejcts.2006.11.030
- Craig SR, Walker WS. A proposed anatomical classification of the pulmonary fissures. J R Coll Surg Edinb. 1997;42(4):233-234.
- Schieman C, MacGregor JH, Kelly E, et al. Can preoperative computed tomography of the chest predict completeness of the major pulmonary fissure at surgery? Can J Surg. 2011;54(4):252-256. doi:10.1503/cjs.007910
- Sihoe ADL. Video-assisted thoracoscopic surgery as the gold standard for lung cancer surgery. Respirology. 2020;25 Suppl 2:49-60. doi:10.1111/resp.13920
- Manolache V, Motas N, Davidescu M, et al. Minimally invasive thoracic surgery - video assisted thoracic surgery: technique and indications. Chirurgia (Bucur). 2022;117(1):101-109. doi:10.21614/chirurgia.2608
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (Vats) lobectomy using a standardized anterior approach. Surg Endosc. 2011;25(4):1263-1269. doi:10.1007/s00464-010-1355-9
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.





Comments