ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Life-Threatening Left Subclavian Arterial Rupture Following Blunt Thoracic Trauma: A Case Report
Tran KT. Life-Threatening Left Subclavian Arterial Rupture Following Blunt Thoracic Trauma: A Case Report. June 2019. doi:10.25373/ctsnet.8307314.
Introduction
Traumatic subclavian arterial rupture represents an uncommon complication of blunt chest trauma. Arterial rupture usually causes massive hemorrhages, and it must be quickly and properly confirmed by physical examination. Although it is uncommon, it is a challenging surgical problem and many surgeons have limited experience with its management [3, 4]. In recent years, complex subclavian injuries have been increasingly managed through endovascular intervention that is applied for patients who are hemodynamically stable at presentation [11]. However, for subclavian artery injury that appears early after trauma and arterial rupture that may cause life-threatening hemorrhages, surgery continues to be the only available treatment of choice in order to save the patient.
The author reports a clinical case of left subclavian arterial rupture after blunt chest trauma with profound hemorrhagic shock and almost clinical death. The patient received a successful operation with median sternotomy associated with left anterior thoracotomy in the style of “opening book” incisions.
Observation
A previously healthy 20-year-old man had a traffic accident and was immediately brought to the author’s hospital.
Reported on admittance, the patient was still conscious and breathing with difficulty with a rapid respiratory rate, more than 40 breaths per minute. The patient had an unstable hemodynamic status with blood pressure about 50/40 mmHg and a peripheral pulse rate more than 150 bpm. The distal pulses were not palpable in left upper extremities. The left hemithorax presented with multiple ecchymoses. No thoracic deformation was reported, but there was a complete absence of breath sounds in the left hemithorax. No fractures of extremities were found, and the abdomen was flat. The pelvis was stable.
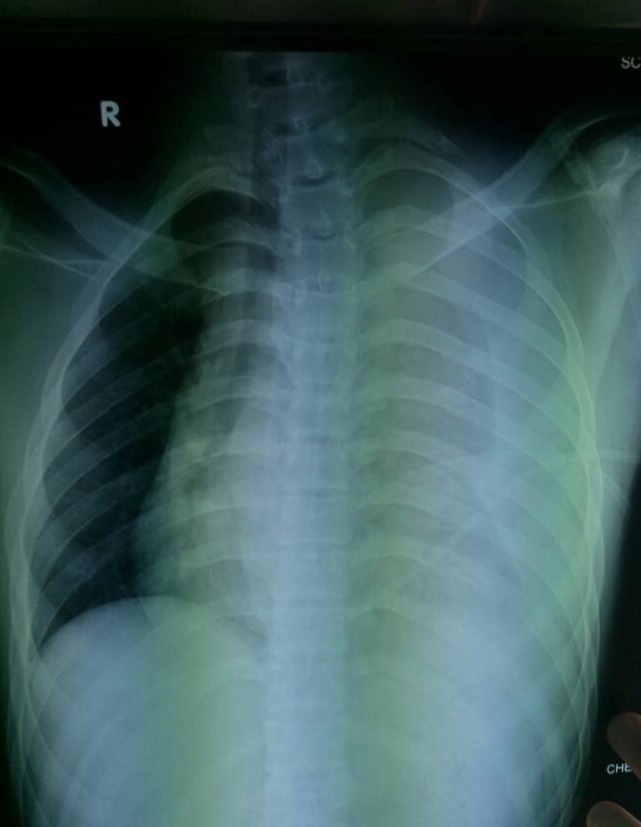
Figure 1. Image showing a massive left hemothorax, mediastinum displaced to the right with fracture of the first rib.
Resuscitation was initiated while a chest plain radiography on the bed was immediately performed (Figure 1). The author found the sign of a massive left hemothorax with mediastinal displacement to the right side, and the first left rib was fractured. The left clavicle remained intact. In this clinical setting, there was no time to make further imaging explorations, and the patient was urgently sent to the operating room for an emergency operation with a suspected diagnosis of fatal subclavian arterial rupture following blunt thoracic trauma.
Upon arriving in the operating room, the patient experienced bradycardia and then a cardiac arrest. The patient was intubated for general anesthesia and resuscitated aggressively with blood and other solutions available. Meanwhile a cardiac massage and an immediate access to the intrathoracic lesions were carried out. The author used two incisions: a median sternotomy and a left anterior thoracotomy via the third intercostal space according to an “opening book” style.
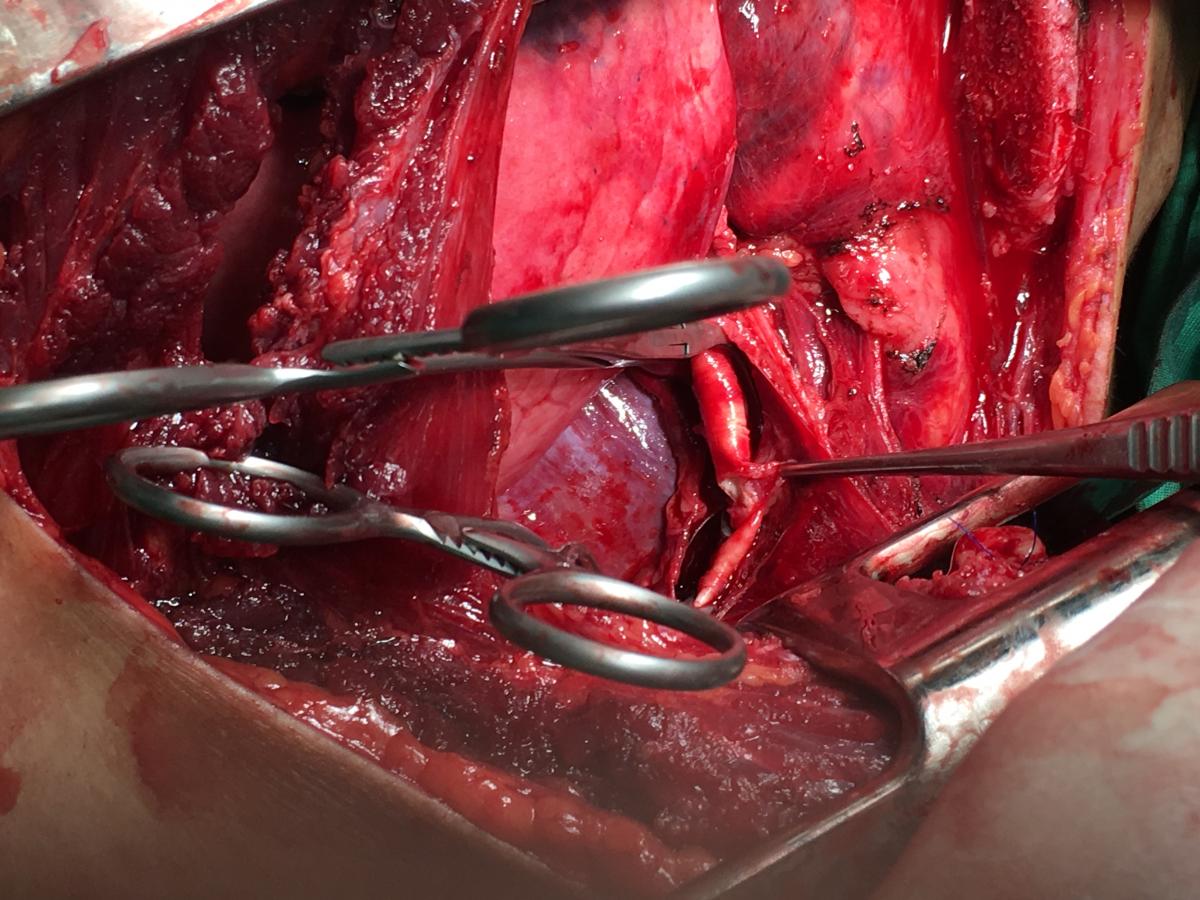
When the thorax was opened, the surgical team discovered the left pleural cavity flooded with blood and bleeding from the left ruptured subclavian artery, about 1 cm from its origin. There was no pericardial effusion. The bleeding artery was occluded quickly with two vascular clamps while the resuscitation continued with direct cardiac massage, vasoactive agents, solutions, and blood infusion (Figure 2). During the next 15 minutes, the heart returned a ventricular fibrillation and two direct electric shocks of 10 joules were applied, the sinusal rhythm then recovered and blood pressure was resumed. From that time until the end of operation, the hemodynamic parameters well-controlled in the acceptable range, with medium blood pressure around 60 mmHg. The patient’s two pupils were moderately dilated (about 4 mm) and almost slowly reactive to light.
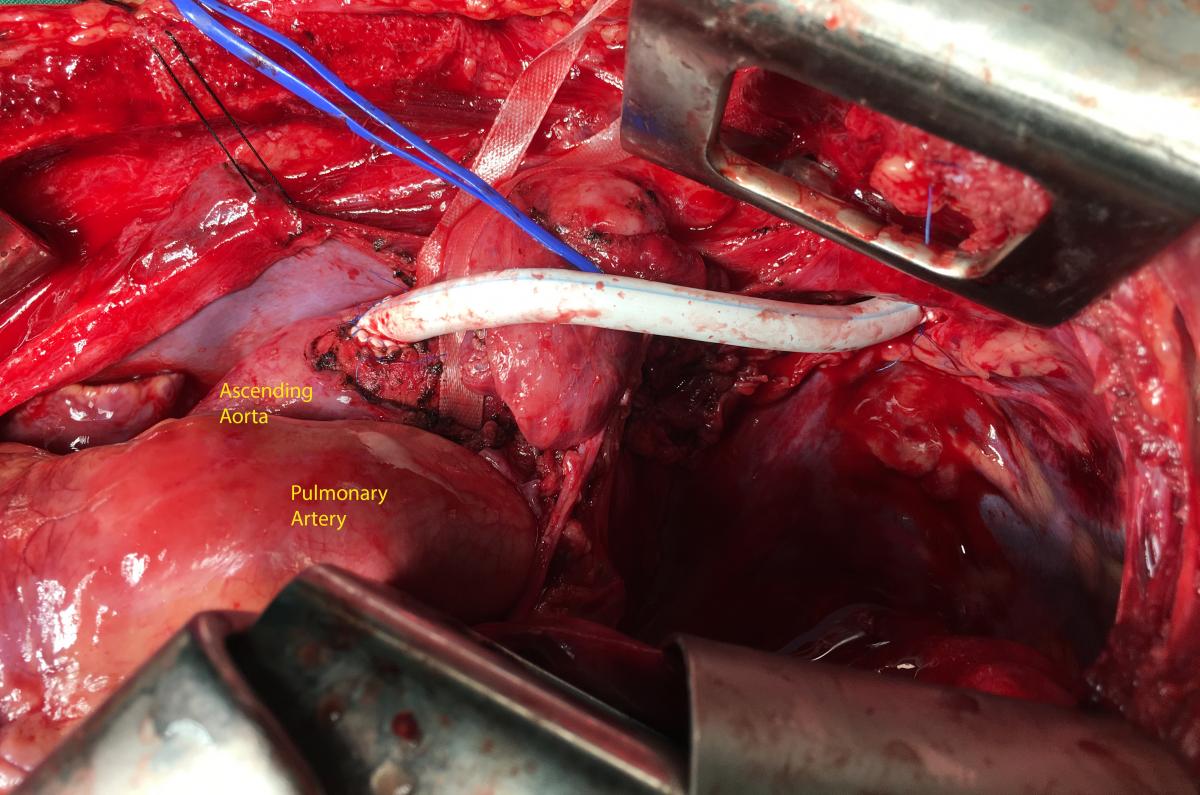
The left subclavian artery was ruptured about 2 cm of length, but the arterial wall was contused longer than the ruptured portion—this extended from the origin of subclavian to the left vertebral artery. The origin of subclavian artery was sutured with pledgets on the aortic wall, and a bypass with Gore-Tex 6 mm diameter was realized between ascending aorta and subclavian artery (the postlesion segment). The proximal and distal anastomoses were made with a termino-lateral and a termino-terminal type, respectively. The flux of left vertebral artery was preserved (Figure 3).
The lost blood estimated approximately 4000 ml, and the surgical team used up to 21 units of blood and other blood products to resuscitate this patient.
Postoperatively, the patient’s hemodynamic condition was stable, his pupils were bilaterally isochoric, isocyclic, and reactive to light, and his urine volume began to recover with no evidence of renal insufficiency. Troponin I concentration elevated up to 22.2 ng/mL but there were not any changes on electrocardiogram. This enzyme was only 3.5 ng/mL on the second postoperative day. Blood lactate was well-corrected from 14 mmol/L down to 3 mmol/L for the first 24 hours. No severe coagulation disorders were noted postoperatively. Cardiac function was preserved on echocardiography. Abdominal ultrasound of postoperative control found no evidence of intra-abdominal lesions, and there was no cervical spine fracture on radiography.
The patient was awakened and extubated successfully on the fourth postoperative day, and his Glasgow Coma Score was 15. Unfortunately, the patient suffered an ischemic lesion of left occipital lobe that was confirmed with computed tomography (CT) scan of the head (Figure 4). He had some symptoms such as imbalance, vision loss, language disorder, and swallowing reflex that were ameliorated for next 9 days, except for the swallowing reflex. The patient was given an endoscopic gastrotomy for a long-term feeding sonde. This sonde was removed successfully after nearly 3 months when the patient could eat by mouth. From that time, the patient was normal and presented neither neurological nor motor sequelae.
Discussions
Traumatic thoracic vascular injuries are often lethal in patients with thoracic trauma. Among these injuries, traumatic subclavian vascular injury is relatively uncommon because it is protected by subclavius muscle, clavicle, first rib, and deep cervical fascia [1]. The true incidence is likely underestimated, as many victims die prior to arriving at the hospital for definitive treatment, and it represents less than 0.4% - 2% of traumatic vascular injuries [3, 6, 9, 11]. Although the incidence is rare, traumatic subclavian artery injury can be fatal with a mortality rate as high as 30% [3, 6]. Some pathological types of subclavian artery injuries can be seen such as stretching, transection, or compression of the subclavian artery by broken bone fragments, in which the rupture lesion can cause massive hemorrhage and the patient quickly falls in severe shock and death [1, 11].
The diagnosis of traumatic subclavian artery injury depends on clinical situations. In cases where the patient is hemodynamically stable, the history may be obtained from the patient, but it is more likely to be provided to the medical staff by pre-hospital personnel and then some imaging diagnostic technique can be carried out in order to confirm the diagnosis of subclavian artery injury. CT angiogram has sensitivities of 97- 99.3% and specificities of 87.1- 99.8% and routine use before angiography and CT are now the diagnostic test of choice. A CT angiogram with 3D reconstruction can throw light on the degree of vascular damage, the level of injury, the involvement of the artery and vein, and any external compression due to hematoma [4, 5, 8].
In this case, the patient was clearly hemodynamically unstable. He suffered a profound shock and even a cardiac arrest during operation. The author could not make the diagnosis based on imaging but the clinical picture helped to make a definitive decision. In some particular situations, several authors agree that the blunt subclavian artery injuries may be suspected clinically [2, 9, 12]. According to Tennyson and colleagues [12], first rib fractures have long been recognized as a hallmark of severe trauma and there are a number of historical reports in the literature of subclavian artery injury directly associated with first-rib fractures. Katras and colleagues [5]. Sturm and Cicero [10] presented criteria that can alert the physician to the possibility of subclavian arterial injury following blunt thoracic trauma, which are: 1) fractured first rib; 2) diminished or absent radial pulse; 3) palpable supraclavicular hematoma; 4) chest film evidence of hematoma over the area of the subclavian artery or a widened superior mediastinum; and 5) brachial plexus palsy. In the situation presented here, the patient had two signs of these criteria, which were the first rib fracture and ipsilateral radial pulse absence. In fact, the criteria of Sturm and Cicero did not mention one highly significant finding, which was massive hemothorax.
Management of subclavian artery injury is still challenging because of its anatomic location (“a difficult corner”) that requests a specialized vascular surgeon. In recent years, advances in endovascular interventions for vascular injuries have achieved increasing success for treatment of subclavian artery injury caused by penetrating trauma such as a gunshot, stab, or iatrogenic catheter injury [11]. However, for a hemodynamically unstable patient, especially with profound hemorrhagic shock, the author thinks emergency operation is the only option. The choice of incision is one of the essential points to save the patient; this depends on the side injured and the location of the arterial disruption. For some authors, the standard approach to left-sided injuries is anterolateral thoracotomy with subsequent supra- or infraclavicular incision, while the right-sided injuries are typically managed by median sternotomy with supraclavicular extension. And for the others, a median sternotomy for exposure of left subclavian artery has been used successfully as it is safe, reliable, gives rapid hemostasis and maximum exposure of the operative field [3]. Nwiloh and colleagues [7] used the trap door incision to manage the left subclavian artery injury, especially for repairing the proximal left subclavian artery. The trap door incision can start with a third or fourth anterior thoracotomy to first obtain control of the proximal left subclavian artery, and then a partial sternotomy to connect the thoracotomy. The upper sternotomy incision is then extended to the supraclavicular region, and the sternum and ribs are then elevated with a chest retractor for exposure of the underlying vessels. The author used two incisions: a median sternotomy and a left anterior thoracotomy in the style of “opening book” with the left clavicle elevated by the sternum retractors. This approach led the surgical team to enter the thorax the most quickly and easily and to avoid traumatism of supraclavicular structures such as nerves, thoracic canal, etc, without claviculectomy.
Postoperatively, the patient presented several signs of left occipital ischemia as mentioned above, although the flux of the vertebral artery was preserved. The reasonable cause to explain this complication was the long time of vertebral clamp during the subclavian artery repair. Its consequences were regressive shortly postoperatively, which showed that the preservation of all branches of subclavian artery are always important. Other postoperative complications were often seen in case of profound hemorrhagic shock such as severe acidosis, coagulation disorders, infection, etc, which were corrected depending on the specific clinical setting that the author did not emphasize in this report. The good rehabilitation of this patient suggests that the diagnostic and operative management option was reasonable.
Conclusions
The subclavian artery injury is rare but often fatal. The key for early diagnosis of such vascular injury is the high index of suspicion with some suggestive clinical criteria. Rapid transportation, aggressive resuscitation, and emergency surgical exposure and repair are the pillars to successfully manage these rare vascular injuries.
References
- Assenza M, Centonze L, Valesini L, Campana G, Corona M, Modini C. Traumatic subclavian arterial rupture: a case report and review of literature. World J Emerg Surg. 2012;7(1):18.
- Chauhan MS, Gupta A, Sharma A, Grover V, Gupta VK. Isolated right subclavian artery injury with fractured right first rib following blunt trauma chest. Int Surg J. 2016;3(2):1015-1017.
- Fares A, Shaikh N. Subclavian artery injury following blunt trauma: a report of three cases. J Emerg Med Trauma Acute Care. 2012;2012(1).
- O'Connor JV, Byrne C, Scalea TM, Griffith BP, Neschis DG. Vascular injuries after blunt chest trauma: diagnosis and management. Scand J Trauma Resusc Emerg Med. 2009;17:42.
- Katras T, Baltazar U, Rush DS, et al. Subclavian arterial injury associated with blunt trauma. Vasc Surg. 2001 Jan-Feb;35(1):43-50.
- Kou HW, Liao CH, Huang JF, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center [published online ahead of print January 9, 2019]. Eur J Trauma Emerg Surg. https://doi.org/10.1007/s00068-018-01070-5
- Nwiloh J, Etukokwu K, Orakwe O, Ikwu C, Onyenwuzor C, Iziga N. (2016). Left subclavian artery injury: is there still a role for trap door incision in the minimally invasive era? Niger J Cardiovasc Thorac Surg. 2016;1(2):67-70.
- Raviraja A, Chandrashekar CM, Roshan SD, Srinivas JV. (2009) Subclavian artery and vein injury following clavicle fracture due to blunt trauma. Injury Extra. 2009;40(2):36-38.
- Sturm JT, Dorsey JS, Olson FR, Perry JF Jr. The management of subclavian artery injuries following blunt thoracic trauma. Ann Thorac Surg. 1984;38(3):188-191.
- Sturm JT, Cicero JJ. The clinical diagnosis of ruptured subclavian artery following blunt thoracic trauma. Ann Emerg Med. 1983 Jan;12(1):17-9.
- Ta N, Idoguchi K, Fukuma H, Ono H, Nakao S, Matsuoka T. Case report: urgent endovascular treatment of subclavian artery injury after blunt trauma [v1; ref status: indexed, http://f1000r.es/4x8]. F1000Research. 2014;3:310.
- Tennyson C, Karunaratne D, McLaughlin KE, Hasan R, Grant SW. Delayed subclavian artery rupture secondary to a traumatic first rib fracture. Trauma Case Rep. 2018;16:1-3.