ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Minimally Invasive Pulmonary Embolectomy With Thoracoscopic Assistance
Fallon J, Zapata D, Pickens A, Halkos M, Lattouf O. Minimally Invasive Pulmonary Embolectomy With Thoracoscopic Assistance. March 2020. doi:10.25373/ctsnet.11964948
Patient Selection
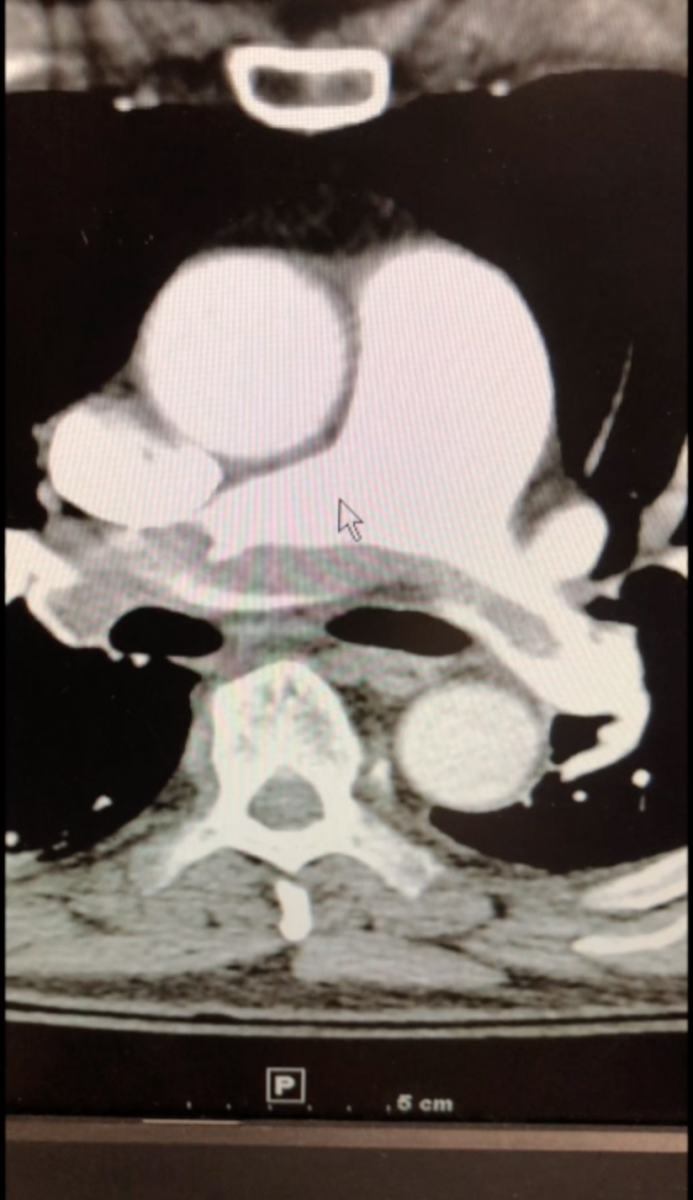
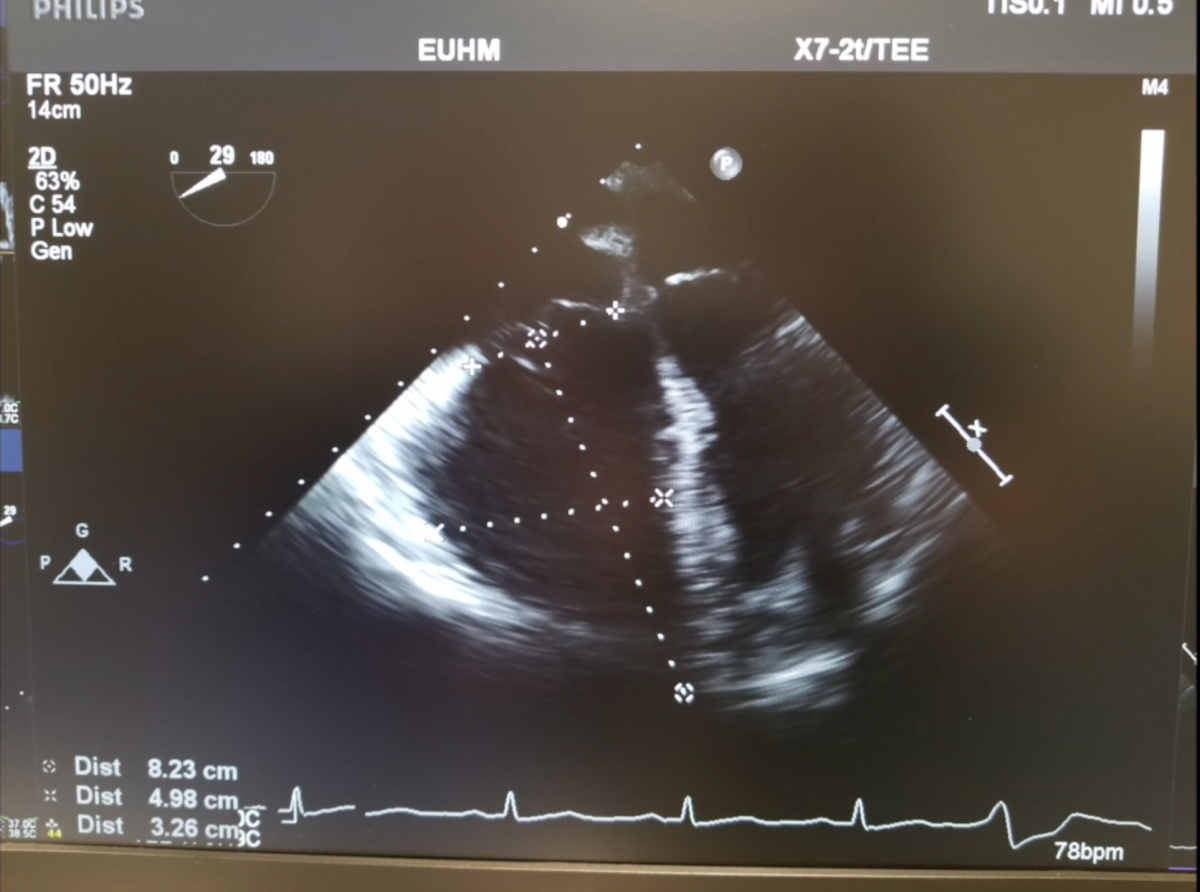
Surgical pulmonary embolectomy (SPE) is a safe and effective therapeutic approach to pulmonary embolism management for patients who are diagnosed with submassive and/or massive acute pulmonary emboli by clinical exam, supported by computed tomography (CT) and echocardiographic assessment. Other indications for surgical embolectomy include presence of thrombus-in-transit, concomitant cardiac pathology such as a large patent foramen ovale, or relative contraindications to thrombolytic therapy, including recent cerebrovascular or intracranial pathology, recent surgery, active bleeding, or other absolute contraindications to anticoagulation.
When such a patient presents to the authors, they activate their Pulmonary Embolectomy Response Team (PERT) and share a brief clinical resume, inclusive of pertinent clinical findings and CT and echo images. Accordingly, the multidisciplinary team, which includes CT surgeons, interventional cardiologists, vascular surgeons, pulmonologist, intensivists, and hematologists deliberate in order to reach a consensus on the best therapeutic approach.
Historically and most commonly, surgical pulmonary embolectomy has been performed through a median sternotomy with central cardiopulmonary bypass with or without cardioplegic arrest. Given advances in surgical technology along with improved safety of peripheral cardiopulmonary bypass, the authors have recently started to implement a minimally invasive approach to this procedure.
Encouraged by early results, the authors currently suggest that a minimally invasive approach for patients presenting with centrally located PE (main PA trunk or proximal right and left pulmonary artery branches) be considered specifically in patients with significant comorbidities or frailty. At this early stage of experience, and until the technique is further refined with the aid of specialized equipment, the authors recommend limiting this approach to proximal pulmonary artery embolic lesions.
However, especially when first implementing this procedure, they recommend a safe and cautious approach, and suggest the standard median sternotomy approach in patients who are or become hemodynamically unstable and in any patient with a complex clinical picture. Below is their step-by-step approach to minimally invasive surgical pulmonary embolectomy.
Operative Steps
- Expose and mobilize the common femoral artery, femoral artery bifurcation, and common femoral vein via an oblique groin incision. Mobilize enough for cannulation with proximal and distal control.
- Perform parasternal minithoracotomy over the left third intercostal space.
- Enter the left pleural space and incise the pericardium over the pulmonary artery to enter the pericardial sac. Place retraction sutures to optimize exposure.
- Use “ThruPort Soft Tissue Retractor” (Edwards LifeSciences) or Aztec Retractor/similar device to retract surrounding soft tissue and allow maximum visualization and access through the small surgical incision. Often, the authors use a self-retaining retractor along with the aforementioned soft tissue retractor to further spread the incision.
- Heparinize and begin peripheral cannulation for cardiopulmonary bypass. Place purse-string sutures in the femoral artery and femoral vein with 5-0 prolene sutures.
- Use the Seldinger technique to access the common femoral vein as follows: Access the vein with a needle and subsequent wire. Serially dilate the vessel to the size of the cannula. Insert venous cannula (25 French venous cannula) and position within the right atrium under TEE guidance. Connect venous line to bypass circuit.
- Use the Seldinger technique to access the common femoral artery as follows: Access the artery with a needle and subsequent wire. Serially dilate the vessel to the size of the cannula. Insert the arterial cannula (18 French Fem Flex cannula). Connect the arterial line to the bypass circuit.
- Commence full cardiopulmonary bypass.
- Make a 3 cm longitudinal incision in the main pulmonary artery. Use an empty ring forceps clamp to extract thrombus under direct visualization.
- Access distal segmental arteries by using a 30-degree, 5 mm thoracoscopic camera to visualize and extract further thrombus.
- For emboli in the left branch pulmonary artery, the operating surgeon should be on right side of the operating table.
- For right branch pulmonary artery emboli, the operating surgeon should be on the left side of the operating table for best distal visualization.
- Close the pulmonary artery in two running layers using 5-0 prolene suture.
- Wean from bypass and decannulate groin vessels. Reverse heparin with protamine. Manage any bleeding until hemostasis.
- Insert two chest tubes (24 French Blake), one in the pericardium and one in the pleural space.
- Close the chest using paracostal sutures to reapproximate the ribs, and multiple running sutures to reapproximate the fascia, subcutaneous tissue, and skin. Close the groin using multiple running sutures to reapproximate the fascia, subcutaneous tissue, and skin.
Preference Card
- Mini Aztec Retractor or ThruPort Soft Tissue Retractor for Thoracotomy
- Medtronic Peripheral Cardiopulmonary Bypass Cannulation Kit, including Arterial and Venous Cannulae
- Ring forceps
- 5 mm 30-degree thoracoscopic camera
- 24 French Blake x2
- 4-0 and 5-0 prolene suture
- Paracostal suture
- TEE availability
Tips and Pitfalls
- Digitally palpate the pulmonary artery prior to pericardiotomy to ensure accurate entry.
- Avoid injury to the left phrenic nerve when entering the pericardium.
- Extract clot slowly and carefully so that it does not fracture during extraction. Using a ringed forceps is also useful in preventing fracture of thrombus.
- Using the thoracoscopic camera to visualize and extract thrombus is particularly useful when clearing the right pulmonary vasculature and is a recommended technique for complete evacuation.
References and Suggested Reading
- Kalra R, Bajaj NS, Arora P, Arora G, Crosland WA, McGiffin DC, et al. Surgical embolectomy for acute pulmonary embolism: systematic review and comprehensive meta-analyses. Ann Thorac Surg. 2017;103:982–990.
- Dauphine C, Omari B. Pulmonary embolectomy for acute massive pulmonary embolism. Ann Thorac Surg. 2005;79:1240-1244.
- Keeling WB, Leshnower BG, Lasajanak Y, Binongo J, Guyton RA, Halkos ME, et al. Midterm benefits of surgical pulmonary embolectomy for acute pulmonary embolus on right ventricular function. J Thorac Cardiovasc Surg. 2016 Sep;152(3):872-878. Epub 2016 Mar 3.
- Keeling WB, Sundt T, Leacche M, Okita Y, Binongo J, Lasajanak Y, et al. Outcomes after surgical pulmonary embolectomy for acute pulmonary embolus: a multi-institutional study. Ann Thorac Surg. 2016 Nov;102(5):1498-1502.
- Kodani N, Ohashi T, Iida H, Kageyama S, Furui M, Uchino G. Emergency pulmonary embolectomy using minimally invasive cardiac surgery. Ann Thorac Surg. 2016 Apr;101(4):1569-1571.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.