ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Rapid Reperfusion: Management Strategy of ATAAD with Cerebral Malperfusion
Thakur SK, Tam R. Rapid Reperfusion: Management Strategy of ATAAD with Cerebral Malperfusion. August 2023. doi:10.25373/ctsnet.23925684
Cerebral malperfusion is a known complication of type A acute aortic dissection, which is linked to considerable perioperative mortality and morbidity. This article presents a case of Stanford acute type A aortic dissection (ATAAD) successfully managed by early percutaneous fenestration, transluminal angioplasty of the right carotid artery, and emergency central aortic repair of the ATAAD.
The Patient
A sixty-four-year-old man presented to the emergency department with a history of syncope followed by tonic-clonic seizures and dense left hemiplegia, without chest or back pain. Because of low GCS, urgent intubation was required. Five years earlier, the patient had undergone an abdominal aortic aneurysm repair, and he had been under annual surveillance for a 45 mm ascending aortic aneurysm. On a head and neck CT with a brain perfusion scan, a significant right MCA area and right frontal lobe infarct without hemorrhagic changes were visible along with evidence of ATAAD affecting the aortic arch and its branches (Figure 2). On the gated CT aortogram, an extensive ATAAD involving arch vessels was visible from the ascending aorta to the abdominal aorta (Figure 1). Both true and false lumens supplied blood to the brachiocephalic artery, and the right common carotid artery's flow was compromised.
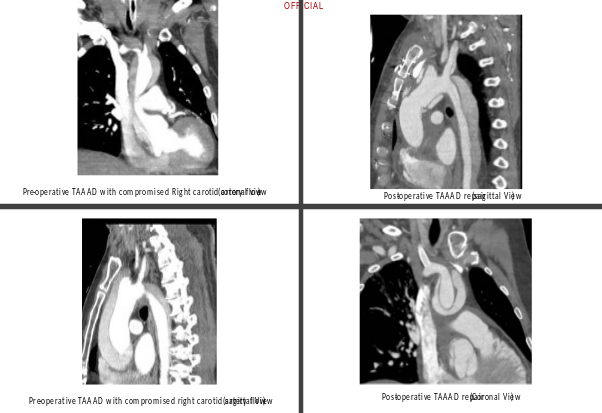
Figure 1
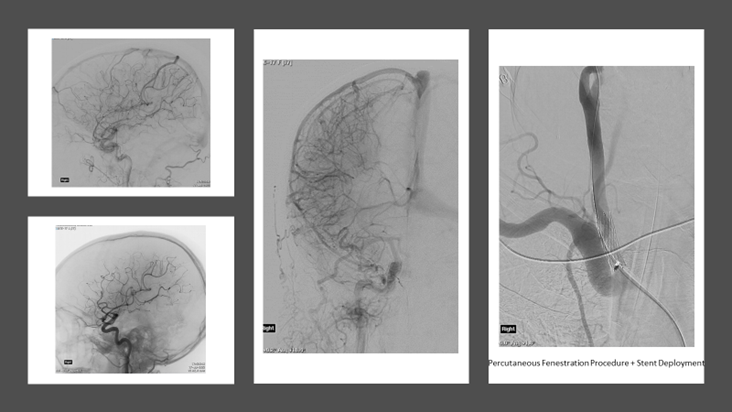
Figure 2
The Procedure
The multidisciplinary team's immediate suggestions included percutaneous fenestration and transluminal angioplasty of the right common carotid artery, followed by an MR perfusion scan to reassess cerebral circulation. Through the right common femoral artery, a successful percutaneous fenestration procedure into the right common carotid artery was carried out, and a stent was successfully deployed (Figure 3).
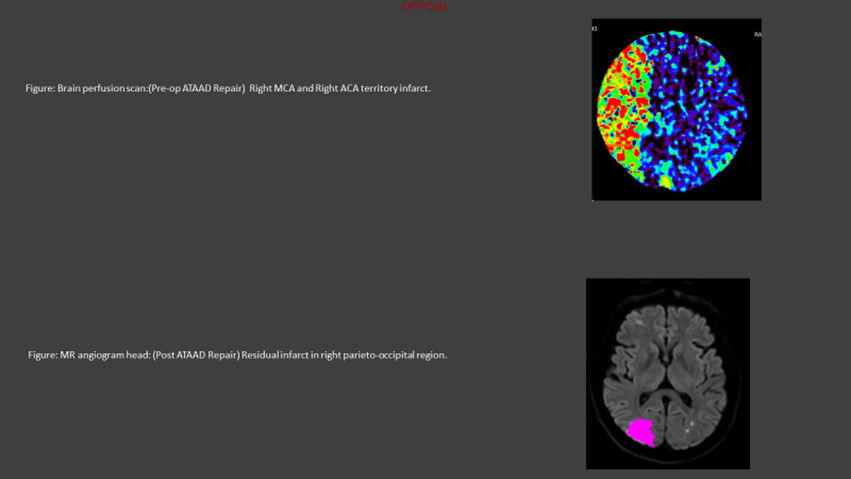
Figure 3
The patient experienced hemodynamic instability during MR imaging, necessitating an urgent pericardiocentesis, followed by prompt ATAAD central aortic repair with right femoro-femoral cardiopulmonary bypass. An antegrade cerebral perfusion via the brachiocephalic artery and hypothermic circulatory arrest at 24°C were used during the surgical procedure. By using the open distal approach, a supracoronary ascending aorta replacement and aortic valve resuspension procedure were performed. Recovery after surgery was difficult because of the patient's prolonged ventilation and acute kidney injury, which resolved within seven days. The patient was discharged home from stroke rehabilitation on postoperative day eighteen after full recovery from left hemiplegia.
Discussion
Although urgent surgical repair of the aorta is the preferred management strategy for patients with ATAAD, the best way to treat ATAAD in patients with cerebral malperfusion is still debated. Cerebral malperfusion complicates 6 to 20.3 percent of ATAAD cases (2,1). Hospital mortality in patients with ATAAD who had cerebral malperfusion was 43.7 percent as opposed to 17 percent without cerebral malperfusion (3).
Central aortic repair, percutaneous fenestration, and direct revascularization of damaged arteries are some of the therapeutic techniques available for restoring blood flow to malperfused areas (4).
There is disagreement over when to restore the central aorta. The results of both immediate and delayed repair for ATAAD with malperfusion have been reported by numerous researchers with varied degrees of success.
Early aortic repair proponents believe aortic repair must be completed immediately. In terms of mortality rates, surgical therapy within five hours, in the rapid repair group, performed better than the delayed repair group, with surgical therapy past five hours, with rates of 14 percent and 67 percent, respectively. Compared to 17 percent in the delayed repair group, 86 percent of patients in the rapid repair group fully recovered (5).
Delaying aortic surgery has been documented in patients with traumatic aortic disruption exacerbated by severe central nervous system injury, severe burns, or infected wounds, and in patients with Marfan syndrome, ATAAD, and stroke (6,7).
In conclusion, for patients with ATAAD and associated cerebral malperfusion, the best course of treatment remains debatable. However, a rapid reperfusion technique followed by a prompt central aortic repair worked reasonably well in this case.
References
- Significance of malperfusion syndromes prior to contemporary surgical repair for acute type A dissection: Outcomes and need for additional revascularizations: European Journal of Cardio-Thoracic Surgery, Volume 32, Issue 2, August 2007, Pages 255–262, ☆ Arnar Geirsson, Wilson Y. Szeto, Alberto Pochettino, Michael L. McGarvey, Martin G. Keane, Y. Joseph Woo, John G. Augoustides, Joseph E. Bavaria
- Stroke and outcomes in patients with acute ATAAD. Circulation. 2013;128(11 Suppl 1) S175. Bossone E, Corteville DC, Harris KM, Suzuki T, Fattori R, Hutchison S, Ehrlich MP, Pyeritz RE, Steg PG, Greason K, Evangelista A, Kline-Rogers E, Montgomery DG, Isselbacher EM, Nienaber CA, Eagle KA.
- Surgical results of acute aortic dissection complicated with cerebral malperfusion. Ann Thorac Surg. 2005;80(1) 72. Tanaka H, Okada K, Yamashita T, Morimoto Y, Kawanishi Y, Okita Y.
- Thorac Cardiovasc Surg. 2017;29(2):181-185. Malperfusion in Type A Dissection: Consider Reperfusion First. Joshua B Goldberg, Steven L Lansman, Masashi Kai, Gilbert H L Tang, Ramin Malekan, David Spielvogel.
- Neurological outcomes after immediate aortic repair for TAAAD complicated by coma. Circulation. 2011;124(11 Suppl) S163.Tsukube T, Hayashi T, Kawahira T, Haraguchi T, Matsukawa R, Kozawa S, Ogawa K, Okita Y.
- Acute Traumatic Disruption of the Thoracic Aorta: A Ten-Year Experience: The Annals of Thoracic Surgery: The Annals of Thoracic Surgery: Volume 31, Issue 4, April 1981, Pages 305-309 Cary W. Akins M.D. Mortimer J.B uckley M.D. Willard Daggett M.D. Joseph B. McIlduff M.D.W. Gerald Austen M.D.
- Intentional delayed repair of acute dissection of the ascending aorta complicated by stroke: J Thorac Cardiovasc Surg, 109 (1995), pp. 807-808; W Piccione, I.N Hamilton, H Najafi
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




