ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Smart App in Cardiac Surgery: Your Pocket Prompter: AORTA TEVAR INDICATOR, a New Tool to Plan the Right Treatment for Thoracic Aorta
Magagna P, Pizzolato C, Balzarin A, Giordan M, Abdellah E, Salvador L. Smart App in Cardiac Surgery; Your Pocket Prompter: AORTA TEVAR INDICATOR, a New Tool to Plan the Right Treatment for Thoracic Aortic Pathology. August 2020. doi:10.25373/ctsnet.12755864
Introduction
The technological revolution in the field of medical education is here and it is time to embrace it. The adoption of the on-the-go learning style, the portability of smartphones, and the expression of concepts with interactive illustrations and their global reach have made application-based learning (apps) an effective means. Aorta Tevar Indicator is an application created for planning endo-prosthetic corrective treatment for diseases of the thoracic aorta. This app has been downloaded worldwide. The results of a survey reveal its widespread acceptance and success. The authors believe that educational apps can have a significant impact on shaping the future of cardiovascular education in the 21st century. This experience with app development and testing could work as a model for other medical educators.
About 80% of the worldwide population owns a mobile phone, independent from the degree of industrialization of their country. There are 5 billion active mobile phones; many are smartphones. On App Store, Google Play, and other stores, there are thousands of apps, but few of them are really useful in clinical practice. Why don’t we use this technology to improve the effectiveness of our medical practice? More specialists, such as neurologists and anesthesiologists, have already introduced smart phones and apps into their daily clinical practice. Several apps in cardiac surgery already exist, but they are mainly guidelines apps. We present a new tool to plan the optimal treatment for thoracic aortic pathology: a smart app named AORTA TEVAR INDICATOR.
If you are not an experienced surgeon, decision making in the setting of aortic pathology may be challenging. This new app guides you in the choice of operative strategy and device selection in the treatment of thoracic aorta pathology. How many times are young surgeons faced with a complex aortic case? In thoracic aortic pathology, the decision making process is based primarily on personal experience because there of unclear guidelines. For inexperienced surgeons interpreting CT images and doing vascular reconstruction, deciding on the treatment strategy (surgical, hybrid or endovascular; single or multistage timing) and choosing the appropriate device is difficult. For experienced surgeons, the App gives simple hints to facilitate the decision making process.
The AORTA TEVAR INDICATOR app guides you in the choice of the strategy and device for an appropriate treatment of thoracic aorta pathology. The app is available on Google Play and in the Apple store. There is also a web based version available through the highlighted link. (www.aortatevarindicator.com).
It is divided in two sections: one is dedicated to the ascending aorta and the other to the descending thoracic aorta. It is recommended to use the application only after diagnostic exams (e.g., CT angiography, MRI, etc.) have been performed in order to have all the required parameters necessary to create the plant project. This application, which is based on well-defined parameters, automatically calculates Body Surface Area (BSA) with the parameters indicated by both Mosteller and Dubois; Aortic diameter predictor at the level of Valsalva's sinuses, the supraaortic ridge, the ascending and descending aorta, Aortic Ratio, Critical Aortic Size, Aortic Size Index, and Z-Score.
The application is currently available for all Android operatiing systems. All the bibliographic references and the authors’ names can be found on your smartphone through the menu key. The app is free, and its development has not been financed by industry.
User's Guide
Aorta Tevar Indicator is an application created for the planning of endo-prosthetic corrective treatment for thoracic aorta pathology, and this application, which is based on well-defined parameters, automatically calculates:
- Body Surface Area (BSA) with the parameters indicated by both Mosteller and Dubois
- Aortic diameter predictor at the level of the Valsalva's sinuses, supraaortic ridge, ascending aorta, and descending aorta
- Aortic Ratio
- Critical Aortic Size
- Aortic Size Index
- Z-Score
It will be possible to choose the pathology of interest through a frame that will appear once the disclaimer is accepted:
Patient Data, Estimate, Type B Dissection, Traumatic (Thoracic Aorta Injury), Videos, References (Fig. 1)
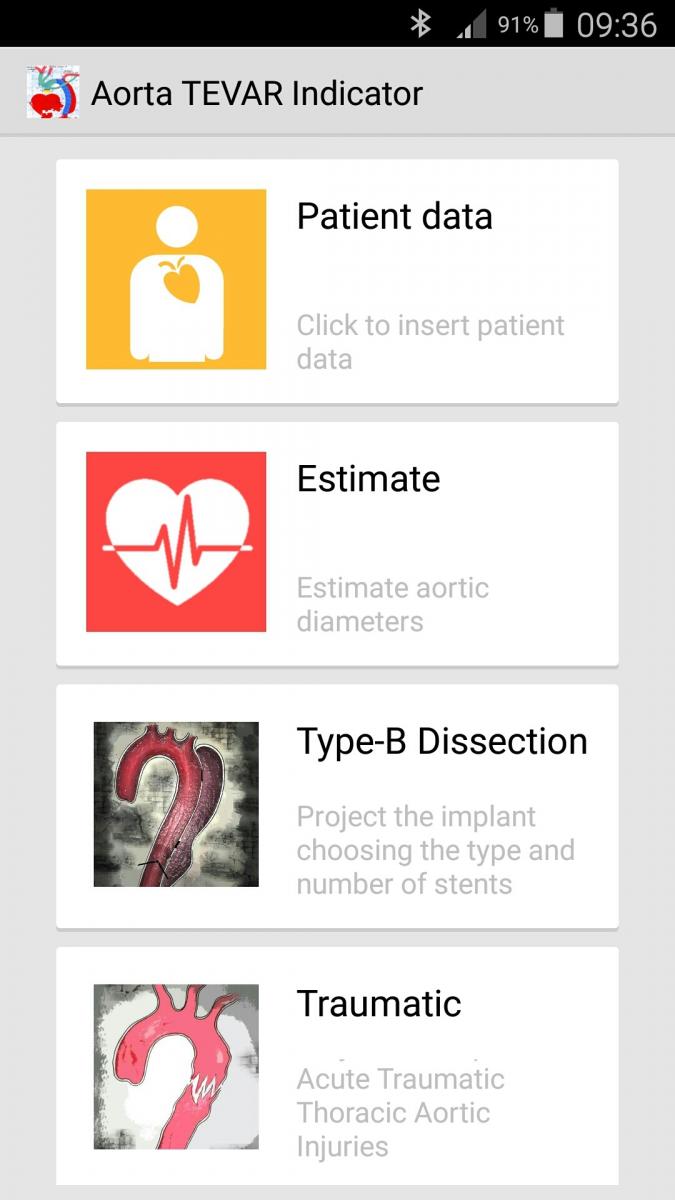
Figure 1
- PATIENT DATA. On this page, the following information must be provided:
- the patient's data (Fig 2)
- age, weight, height, gender, actual aortic diameters (according to Roman's instructions)
- the Body Surface Area (BSA) is calculated automatically according to Mosteller's and Dubois formula, then the following data is to be inserted: "Associated Condition": Marfan's syndrome, bicuspid aortic valve, aortic valve surgery, connective tissue disorder, family history of aortic dissection, hypertension, progressive aortic growth, patient pregnancy, surgeon experience (selecting "surgeon experience" will furnish a short description of the meaning of the term).
- ESTIMATE: Estimate aortic diameters. On this page, the following information must be provided. (Fig. 3)
- Measured aorta diameter (mm)
- Sinus of valsalva
- Supraaortic ridge/proximal ascending aorta
- Descending aorta
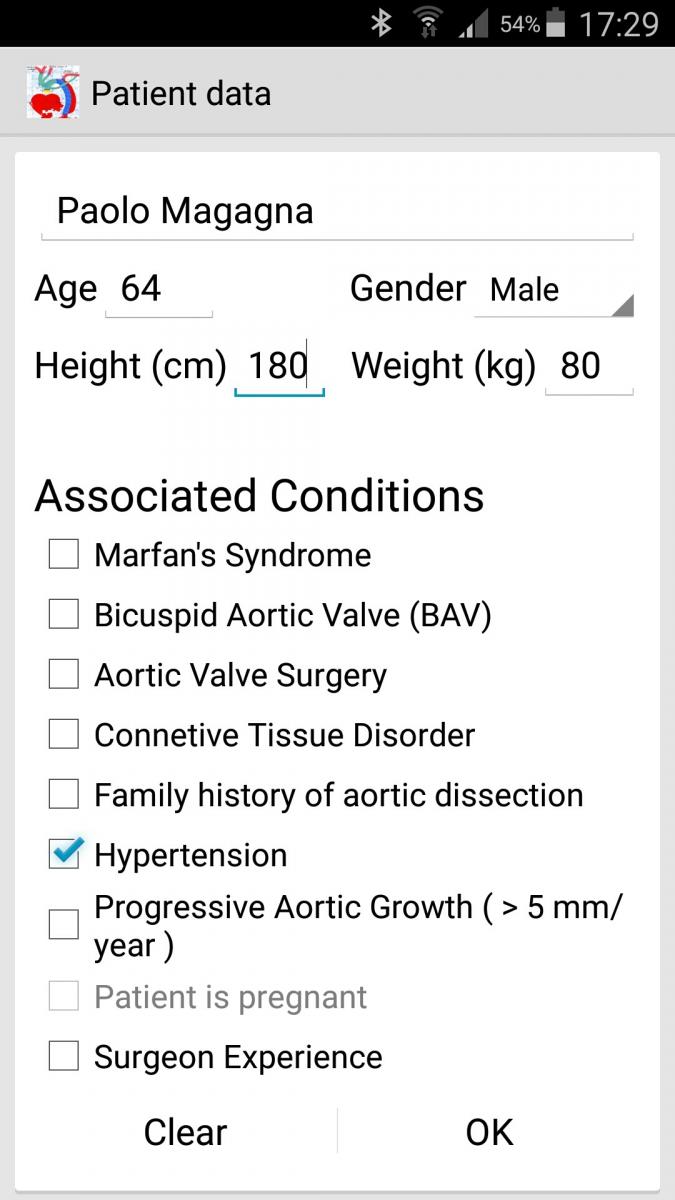
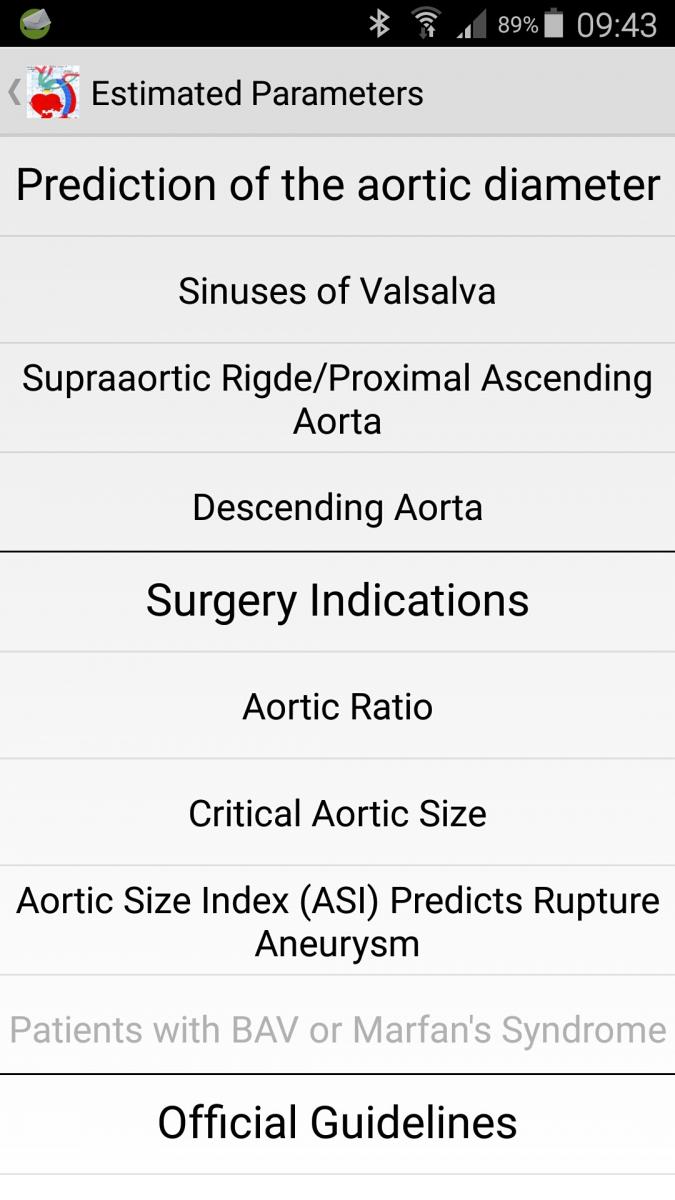
Figure 2 Figure 3
Selecting OK will take you to the second page ("ESTIMATED PARAMETERS"), which is subdivided into three sections:
- In the first section, aortic diameter predictor, the following elements are calculated: the theoretical aortic diameters according to the Roman, Biaggi and Hannuksela models. The Framingham study is likewise calculated for the Valsalva sinuses, for the ascending sinus-tubular-aortic junction, and for the descending thoracic aorta.
- In the second section, "surgery indications," the following parameters are calculated:
- Aortic ratio for the diameters at the Valsalva sinuses and at the ascending tubular-aortic sinus junction (these values must be related to their specific context). Based on the response, one of the following indications will appear: "Provide Operative Treatment" or "follow-up." If the section labelled "Associated Conditions," "Bicuspid Aortic Valve (BAV),” and/or "Marfan's syndrome" were selected, the "Z-Score" will also appear.
- Critical Aortic Size: in this section, the maximum theoretical aortic diameters are calculated and displayed. As above, the display may indicate either the recommendation to seek "Operative Treatment" or "Follow-up".
- Aortic Size Index: it is the ratio between the actual aortic diameter and the BSA. Davies subdivides them into three risk categories: Low Risk (4% yearly rupture); Moderate Risk (8% yearly rupture); Severe Risk (20-25% yearly rupture). Should the calculated risk fall within the "moderate" to "severe" risk range, the recommendation will be for "Provide Operative Treatment." In the event of a low risk calculation, recommendation will be for "Follow-up."
- Patients with BAV or Marfan's syndrome: If in the sections "Associated Conditions" the parameters "Bicuspid Aortic Valve (BAV)” or “Marfan's Syndrome” were selected, and the "critical aortic size index" is above the value of 10 cm/m2, the display will indicate "Provide Operative Treatment."
- DISSECTION TYPE B
You have to fill the patient data: "patient name or code," age, gender, height and weight.
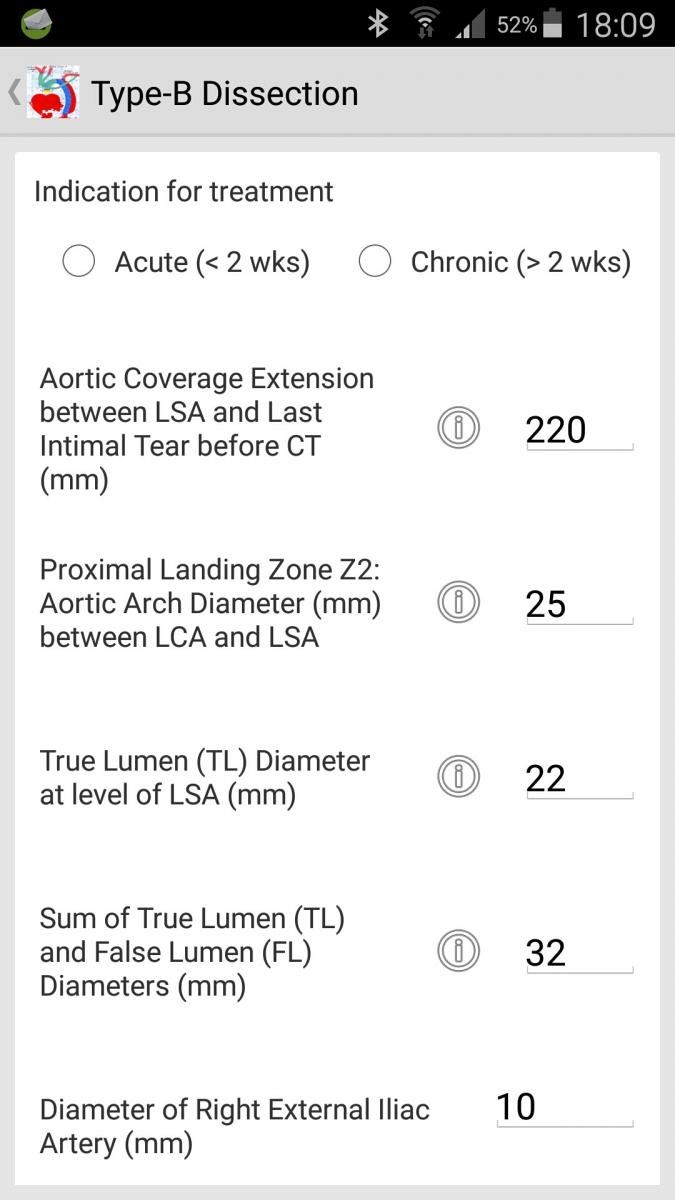
Figure 4
In this section, insert the parameters that will be used for the creation of the endovascular planning (Fig. 4):
- Proximal landing zone-Z2 Aortic Arch Diameter between Left Carotid Artery (LCA) and Left Subclavian Artery (LSA) (mm)
- Aortic diameter predictor (automatic calculations according to the directions of Roman, Biaggi, Hannuksela, and to the study of Framingham)
- Aortic coverage extension: between LSA and Last Intimal Tear before CT (mm)
- True Lumen (TL) diameter (mm)
- Sum True Lumen (TL) diameter + False Lumen (FL) diameter (mm)
- Right external Iliac Artery Diameter (mm)
- Left external Iliac Artery Diameter (mm)
- Right Femoral Artery Diameter (mm)
- Left Femoral Artery Diameter (mm)
Note 1. The IMPLANT DESIGN box shows the most suitable femoral access on the base of the femoral arteries and the stent graft diameters: if both the femoral arteries are not accessible (because of an insufficient diameter), an alternative access will be suggested (transapical access, iliac artery, abdominal aorta, axillary artery).
Note 2. By clicking on “?” on the side of the “Fill Patient Data,” an image will appear.
- INDICATION FOR TREATMENT: here are the major indications for endo-prosthetic treatment, in the acute and in the chronic patient, based on the collected demographic data
- TEVAR Acute Patient (<2 wks): Malperfusion, acute enlargement aortic diameters, persistent pain, uncontrolled hypertension
- TEVAR Chronic Patient (> 2 wks): Instead XL Trial, chronic enlargement aortic diameters (≥ 5 mm within five months), uncontrolled hypertension, transaortic diameters ≥ 40 mm.
Note. By Clicking on "?" near to INSTED XL TRIAL, this table will appear: "Aortic Morphology at 5 Years."
- SELECT IMPLANT TYPE: you can choose between COVER LSA or DON’T COVER LSA
- If you choose “COVER LSA"
- By default, it will be add 2 cm to the inserted value “Aortic coverage extension: between LSA and Last Intimal Tear before CT.” The diameter of the recommended stent graft is calculated on the indicated value in the box "Proximal landing zone-Z2 Aortic Arch Diameter between Left Carotid Artery (LCA) and Left Subclavian Artery (LSA) (mm)
- If you choose “DON’T COVER LSA," the diameter of the STENT GRAFT that you have to use is calculated based on the indicated value in the box “Prediction of The Aorta Diameter.” The length of the recommended Stent Graft and the amount of the implanting Stent Graft is calculated on the insert data in the box: "Aortic coverage extension: between LSA and Last Intimal Tear before CT (mm)"
Note. A 4.5 cm stent graft overlapping has already been considered when more stent graft is required.
- EXCUTE CALCULATIONS
Click on PLANNING
- SELECT MANUFACTURER: All stent graft brands will be shown in the box. Based on the provided data, you could choose among those brands (Bolton Relay, Gore-Tag, Jotec, Medtronic, Zenith-Cook).
- SELECT SOLUTION: By clicking on the stent graft brand name, you will see:
- The different solutions about the implant
- Model stent Graft
- IMPLANT DESIGN There will be indicated: (Fig. 5)
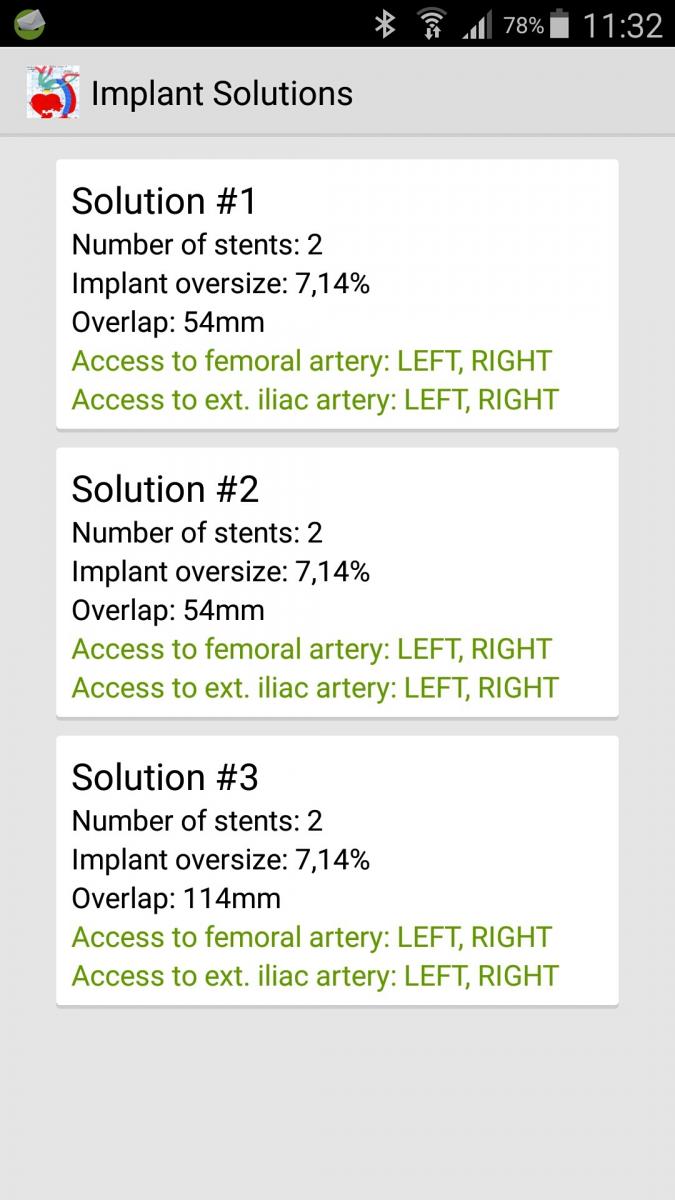
Figure 5
The Proximal and Distal Diameter Stent Graft
Covered Length
Catheter Diameter
Product Code
Implant Oversizing
Access suggest
Note. By clicking on the PDF icon on the right in the box “Implant Design,” it is possible to create a PDF form, reporting all the information about the patient's data and about the recommended stent grafts.
- THORACIC AORTA INJURY
You have to fill the patient data: "patient name or code," age, gender, height and weight
In this section, fill in the needed parameters useful to the creation of the endovascular planning.
- Proximal landing zone-Z2 Aortic Arch Diameter between Left Carotid Artery (LCA) and Left Subclavian Artery (LSA) (mm)
- Proximal landing zone Z3: Descending aorta diameter at LSA level or before aortic injury (mm)
- Distal landing zone Z4: Descending aorta diameter distally after aortic injury (mm)
- Aortic diameter predictor (automatic calculations according to the directions of Roman, Biaggi, Hannuksela, and to the study of Framingham)
- Aortic coverage extension: Suggested proximal and distal landing zone >20 mm
- Right external Iliac Artery Diameter (mm)
- Left external Iliac Artery Diameter (mm)
- Right Femoral Artery Diameter (mm)
- Left Femoral Artery Diameter (mm)
Note 1. The IMPLANT DESIGN box shows the most suitable femoral access on the base of the femoral arteries and the stent graft diameters. If both the femoral arteries are not accessible (because of an insufficient diameter), an alternative access will be suggested (transapical access, iliac artery, abdominal aorta, axillary artery).
Note 2. By clicking on “?” on the side of the “Fill patient data,” an image will appear.
- AORTIC INJURY CLASSIFICATION: it is from “Classification of blunt aortic injuries a new systematic overview of aortic trauma. Forensic Science International 195 (2010) 6-9”
- SELECT IMPLANT TYPE: you may choose between COVER LSA or DON’T COVER LSA.
- If you choose “COVER LSA”
- It will be added 2 cm by default to the inserted value in the Aortic coverage extension: Suggested proximal and distal landing zone >20 mm. The diameter of the recommended stent graft is calculated on the indicated value in the box "Proximal landing zone-Z2 AORTIC ARCH DIAMETER BETWEEN LEFT CAROTID ARTERY (LCA) AND LEFT SUBCLAVIAN ARTERY (LSA)
- If you choose "DON’T COVER LSA"
- The diameter of the stent graft to use is calculated on the indicated value in the box “Proximal landing zone Z3: Descending aorta diameter at LSA level or before aortic injury (mm)”. The length of the recommended Stent Graft and the number of the implanting Stent Graft are calculated on the basis of the data inserted in the box " Aortic coverage extension: Suggested proximal and distal landing zone >20 mm”
Note 1. A 4.5 cm Stent Graft overlapping has already been considered in case more Stent Graft are required
Note 2. By clicking on “?” on the side of the “Fill patient Data” box an image will appear
- EXCUTE CALCULATIONS
Click on PLANNING
- SELECT MANUFACTURER: All stent Graft brands will be shown in the box. Based on the inserted data, you could choose among those brands (Bolton Relay, Gore-Tag, Jotec, Medtronic, Zenith-Cook).
- SELECT SOLUTION: by clicking on the Stent Graft brand name, you will see:
The different solutions about the implant
Model Stent Graft
- IMPLANT DESIGN. There will be indicated:
PROXIMAL, DISTAL DIAMETER STENT GRAFT
Covered Length
Catheter Diameter
Product Code
Implant Oversizing
Access suggest
Note. By Clicking on the PDF icon on the right in the box “Implant Design,” it is possible to create a PDF form, reporting all the information about the patient's anagraphic data and about the recommended Stent Grafts.
- DEBRANCHING AND ANEURYSM: the patients who underwent a debranching of epiaortic vessels and in which there remains an aneurysmal disease of the descending thoracic aorta
You have to fill the patient data "patient name or code," age, gender, height and weight
In this section, you have to insert the parameters that will be used for the creation of the endovascular planning:
- PROXIMAL LANDING ZONE Used graft size (mm)
- DISTAL LANDING ZONE – Z4 - Aorta Descending Diameter proximal to the celiac trunk (suggest proximal and distal landing zone ≥ 20 mm)
- Aortic coverage extension between the origin the last epiaortic branch or the origin the LSA and DISTAL LANDING ZONE (mm)
- Right external Iliac Artery Diameter (mm)
- Left external Iliac Artery Diameter (mm)
- Right Femoral Artery Diameter (mm)
- Left Femoral Artery Diameter (mm)
- Proximal Angle Neck
Note 1. The IMPLANT DESIGN box shows the most suitable femoral access on the base of the femoral arteries and the Stent Graft diameters: if both the femoral arteries are not accessible (because of an insufficient diameter), an alternative access will be suggested (transapical access, iliac artery, abdominal aorta, axillary artery).
Note 2. By Clicking on “?” on the side of the “Fill patient data,” an image will appear
- INDICATIONS FOR TREATMENT: Endovascular repair should be considered as an option of repair for descending thoracic aorta aneurysm for patients unfit for open repair or for those fit patients with favorable anatomy (class IIa), impending aneurysm rupture with hemothorax, symptomatic descending aneurysm with recurrent chest pain, diameter aneurysm ≥ 6 cm, acute enlargement (Elefteriades JA. Natural history of thoracic aortic aneurysms: indications for surgery, and surgical versus nonsurgical risks. Ann Thorac Surg. Nov 2002;74 (5):S1877-80)
- EXCUTE CALCULATIONS
Click on PLANNING
- SELECT MANUFACTURER: All stent Graft brands will be shown in the box. Based on the inserted data, you could choose among those brands (Bolton Relay, Gore-Tag, Jotec, Medtronic, Zenith-Cook).
- SELECT SOLUTION: By clicking on the Stent Graft brand name, you will see:
The different solutions about the implant
Model Stent Graft
- IMPLANT DESIGN. There will be indicated:
PROXIMAL, DISTAL DIAMETER STENT GRAFT
Covered Length
Catheter Diameter
Product Code
Implant Oversizing
Access suggest
Note. By clicking on the PDF icon on the right in the box “Implant Design,” it is possible to create a PDF form, reporting all the information about the patient's data, and about the recommended stent grafts.
Limited liability
The above information is furnished exclusively as an informative tool and does not represent any claim to product accuracy or to completeness of product information. The data and information provided are furnished "as is" and no guarantee (implicit or explicit) is made as to their validity. Any clinical or surgical decisions made on the basis of the use of this product are the sole responsibility of the medical professional.
The author accepts no responsibility for the consequences of choice and use of the devices.
Intellectual property rights
All contents (text, images, software architecture, etc.) are protected by current copyright laws. Reproduction in whole or in part of this product is forbidden without the express written consent of the product owner with the exception of storage in a digital device (computer, smart phone or tablet).
CONCLUSION
It is difficult to put a patient in a mathematic formula, so every result needs to be put into context. AORTA TEVAR INDICATOR is different from other systems because it is the only app for android and IOS and is also a web app. Its conception starts from the pathology analysis. The app has a database that can be easily updated. It does have to be perfected. Further development of this app can only be done with your feedback.
AORTA TEVAR INDICATOR app is now available on APP STORE and on GOOGLE PLAY.
https://play.google.com/store/apps/details?id=com.irrlicht.aortatevarind...
https://itunes.apple.com/it/app/aorta-tevar-indicator/id1055302897?mt=8
References
- Akin I, Kische S, Rehders TC, et al. Thoracic endovascular stent-graft therapy in aortic dissection. Curr Opin Cardiol. 2010;25:552-9.
- Czerny M, Roedler S, Fakhimi S, et al. Midterm results of thoracic endovascular aortic repair in patients with aneurysms involving the descending aorta originating from chronic type B dissections. Ann Thorac Surg. 2010;90:90-4.
- Zoli S, Etz CD, Roder F, et al. Long-term survival after open repair of chronic distal aortic dissection. Ann Thorac Surg. 2010;89:1458-66.
- Parsa CJ, Schroder JN, Daneshmand MA, et al. Midterm results for endovascular repair of complicated acute and chronic type B aortic dissection. Ann Thorac Surg. 2010;89:97-102.
- Xu SD, Huang FJ, Yang JF, et al. Early and midterm results of thoracic endovascular aortic repair of chronic type B aortic dissection. J Thorac Cardiovasc Surg. 2010;139:1548-53.
- Manning BJ, Dias N, Ohrlander T, et al. Endovascular treatment for chronic type B dissection: limitations of short stent-grafts revealed at midterm follow-up. J Endovasc Ther. 2009;16:590-7.
- Blount KJ, Hagspiel KD. Aortic diameter, true lumen, and false lumen growth rates in chronic type B aortic dissection. AJR Am J Roentgenol. 2009;192:W222-9.
- Rodriguez JA, Olsen DM, Lucas L, et al. Aortic remodeling after endografting of thoraco abdominal aortic dissection. J Vasc Surg. 2008;47:1188-94.
- Hager E, Moudgill N, Lipman A, et al. Coil-assisted false lumen thrombosis in complicated chronic type B dissection. J Vasc Surg. 2008;48:465-8.
- Czerny M, Zimpfer D, Rodler S, et al. Endovascular stent-graft placement of aneurysms involving the descending aorta originating from chronic type B dissections. Ann Thorac Surg. 2007;83:1635-9.
- Christoph A. Nienaber, Stephan Kische, Hervé Rousseau, Holger Eggebrecht, Tim C. Rehders Guenther Kundt, Aenne Glass, Dierk Scheinert, Martin Czerny, Tilo Kleinfeldt, Burkhart Zipfel Louis Labrousse, Rossella Fattori and Hüseyin Ince for the INSTEAD-XL trial. Endovascular repair of Type B aortic dissection: long-term results of the Randomized Investigation of Stent Grafts in Aortic Dissection Trial. Circ Cardiovasc Interv. 2013;6:407-416
- Hagan PG, Nienaber CA, Isselbacher EM, et al. International Registry of Acute Aortic Dissection (IRAD): new insights from an old disease. JAMA 2000; 283:897–903.
- Braverman AC, Thompson R, Sanchez L. Diseases of the aorta. In: Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s Heart Disease, 9th Edition. Elsevier, Philadelphia, 2011.
- Hiratzka LF, Bakris GL, Beckman JA, et al. American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines; American Association for Thoracic Surgery; American College of Radiology; American Stroke Association; Society of Cardiovascular Anesthesiologists; Society for Cardiovascular Angiography and Interventions; Society of Interventional Radiology; Society of Thoracic Surgeons; Society for Vascular Medicine. Guidelines for the management of patients with thoracic aortic disease. Circulation 2010; 121:e266–e369.
- Rogers AM, Herman LK, Booher AM, et al. Sensitivity of the aortic dissection detection risk score, a novel guideline-based tool for identification of acute aortic dissection at initial presentation. Results from the International Registry of Acute Aortic Dissection. Circulation 2011; 123:2213–2228.
- Braverman AC. Acute aortic dissection: clinician update. Circulation 2010; 122:184–188.
- Davies RR, Gallo A, Coady MA, et al. Novel measurement of relative aortic size predicts rupture of thoracic aortic aneurysms. Ann Thorac Surg 2006; 81:169–177.
- Pape LA, Tsai TT, Isselbacher EM, et al. Aortic diameter >5.5 cm is not a good predictor of type A aortic dissection. Observations from the International Registry of Acute Aortic Dissection. Circulation 2007;116:1120–1127.
- Parish LM, Gorman JH III, Kahn S, et al. Aortic size in acute type A dissection: implications for preventative ascending aortic replacement. Eur J Cardiothorac Surg 2009; 35:941–945.
- Gaul C, Dietrich W, Erbguth FJ. Neurological symptoms in acute aortic dissection: a challenge for neurologists. Cerebrovasc Dis 2008; 26:1–8.
- Upchurch GR, Nienaber C, Fattori R, et al. Acute aortic dissection presenting with primarily abdominal pain: a rare manifestation of a deadly disease. Ann Vasc Surg 2005; 19:367–373.
- Suzuki T, Distante A, Zizza A, et al. Diagnosis of acute aortic dissection by D-dimer: the International Registry of Acute Aortic Dissection substudy on biomarkers (IRAD-bio) experience. Circulation 2009; 119:2702–2707
- Ticijana Prijon a, Branko Ermenc. Classification of blunt aortic injuries a new systematic overview of aortic trauma Forensic Science International 2010;195:6–9
- Elefteriades JA. Natural history of thoracic aortic aneurysms: indications for surgery, and surgical versus nonsurgical risks. Ann Thorac Surg. Nov 2002;74(5):S1877-80
- Konstantinos G. Moulakakis1,2, Spyridon N. Mylonas1,2,3, Ilias Dalainas1, John Kakisis1, Thomas Kotsis3, Christos D. Liapis. Management of complicated and uncomplicated acute type B dissection. A systematic review and meta-analysis. Ann Cardiothorac Surg 2014;3(3):234-246.
- Raimund Erbel, Victor Aboyans, Catherine Boileau, Eduardo Bossone, Roberto Di Bartolomeo, et al. 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014; 35 (41):2873–2926.
- Elizabeth L. Norton, Xiaoting Wu, Linda Farhat, Karen M. Kim, Himanshu J. Patel, G Michael Deeb, Bo Yang. Dissection of arch branches alone an indication for aggressive arch management in Type A dissection? Ann Thorac Surge (2019), doi: https://doi.org/10.1016/j.athoracsur.2019.06.060.
- Current options and recommendations for the treatment of thoracic aortic pathologies involving the aortic arch: an expert consensus document of the European Association for Cardio-Thoracic surgery (EACTS) and the European Society for Vascular Surgery (ESVS) Czerny M, Schmidli J, Adler S, van den Berg JC, Bertoglio L, Carrel T, Chiesa R, Clough RE, Eberle B, Etz C, Grabenwöger M, Haulon S, Jakob H12, Kari FA, Mestres CA, Pacini D, Resch T, Rylski B, Schoenhoff F, Shrestha M, von Tengg-Kobligk H, Tsagakis K, Wyss TR; EACTS/ESVS scientific document group. Eur J Cardiothorac Surg. 2019 Jan 1;55(1):133-162. doi: 10.1093/ejcts/ezy313.
- 2014 ESC Guidelines on the diagnosis and treatment of aortic diseases Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur Heart J 2014;35: 2873–2926 doi:10.1093/eurheartj/ehu281
- Mokashi SA, Svensson LG. Guidelines for the management of thoracic aortic disease in 2017. Gen Thorac Cardiovasc Surg. 2017;67(1):59-65. doi: 10.1007/s11748-017-0831-8.
- “Patologia dell'aorta toracica: Trattamento chirurgico ed endovascolare”. Edition Piccin. Paolo Magagna. December 2012. IBSN 978-88-299-299
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




