ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Surgery for Chronic Thromboembolic Pulmonary Hypertension: Thromboendarterectomy of the Pulmonary Artery
Jan A, Shah SM, Muhammad A, et al.. Surgery for Chronic Thromboembolic Pulmonary Hypertension: Thromboendarterectomy of the Pulmonary Artery. February 2019. doi:10.25373/ctsnet.7757375.
Introduction
Chronic thromboembolic pulmonary hypertension (CTEPH) is caused by proximal pulmonary artery thromboembolic occlusion or obstruction. Patients present with shortness of breath, early fatigue, and decreased exercise capacity. Once the obstruction sets in, it is accompanied by remodeling of the branches of the pulmonary artery. This causes pulmonary artery hypertension and subsequently leads to right ventricular (RV) dysfunction, which eventually leads to RV failure [1]. The American Heart Association makes a class 1 recommendation that indicates CTEPH should be promptly evaluated for pulmonary endarterectomy, even if symptoms are mild [1].
Pulmonary thromboendarterectomy is a potentially curative surgery for CTEPH. The incidence is estimated to be between one and five percent among survivors of acute pulmonary embolism (PE) [2]. However, diagnostic data from echocardiography and computed tomography (CT) scans done when PE is first diagnosed suggest that many patients with CTEPH have undiagnosed pulmonary hypertension. This may indicate that the first clinical presentation of CTEPH may present as acute PE [3]. Apart from pulmonary embolism, hypercoagulable states may be the etiology of this disease.
Medical therapy is aimed at lowering the resistance of and pressure in pulmonary vessels. This includes vasodilators and drugs inducing remodeling of the vessels. It does improve symptoms such as exercise intolerance and oxygen desaturation. Medical therapy is not curative, and its effects are relatively modest [4]. Surgery is the only definitive therapy for CTEPH, and pulmonary thromboendarterectomy is the surgical procedure of choice.
Patient History
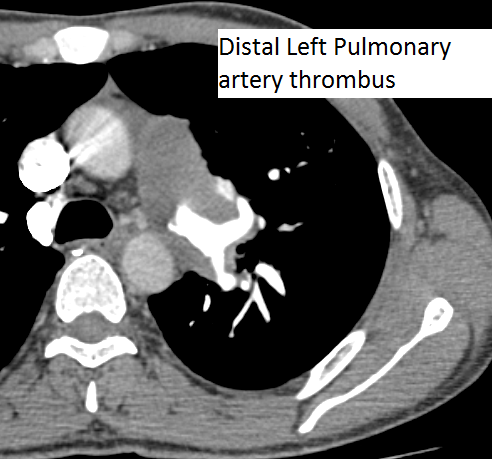
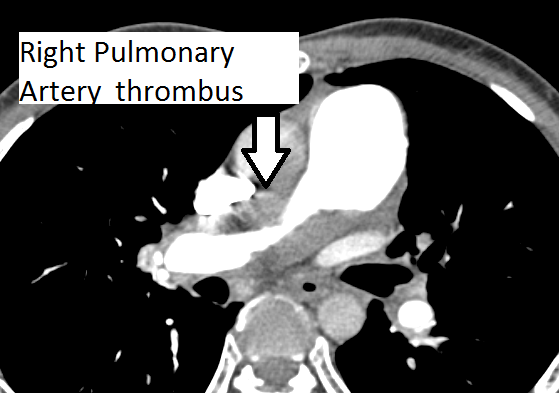
The authors present a case of CTEPH. The patient was a 35-year-old man presenting as an outpatient with complaints of severe progressive dyspnea. He was diagnosed with pulmonary embolism in the past and has been on anticoagulation for more than three years. He has had CT scans and chest x-rays in between. Multiple transthoracic echocardiograms have been performed with evidence of slowly declining right ventricular function. This time, he presented to the cardiac surgery service with a severely dilated and dysfunctional right ventricle. He had been on diuretics and vasodilator treatment but had mild to no improvement. After a thorough review, the authors decided to perform a pulmonary thromboembolectomy. The CT scan images show a dilated RV and intravenous contrast reflux in the inferior vena cava (Figures 1-4). The thrombus can be seen starting in the main pulmonary artery and almost completely occluding it. The thrombus extends into the bilateral pulmonary arteries.
Surgical Techniques
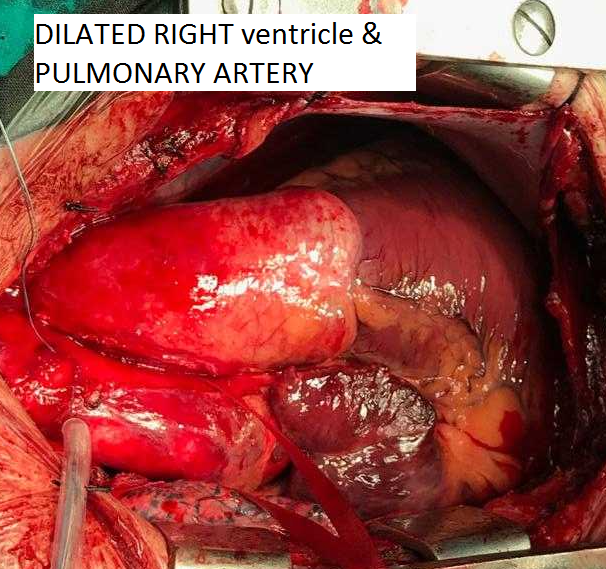
The authors stopped the patient’s oral anticoagulation preoperatively. During surgery the patient had general anesthesia induced, and a standard midline sternotomy was performed. After heparinization the patient was put on cardiopulmonary bypass with aorto-bicaval bypass. Before going on bypass, both pulmonary arteries were dissected laterally to the start of branching. A dilated RV and pulmonary arteries could be visualized (Figure 5). On the right side, the underside of the aorta and superior vena cava (SVC) were completely dissected to have a clear view of right pulmonary artery (RPA). Moderate hypothermia was induced in order to be prepared if the authors needed to decrease the flow.
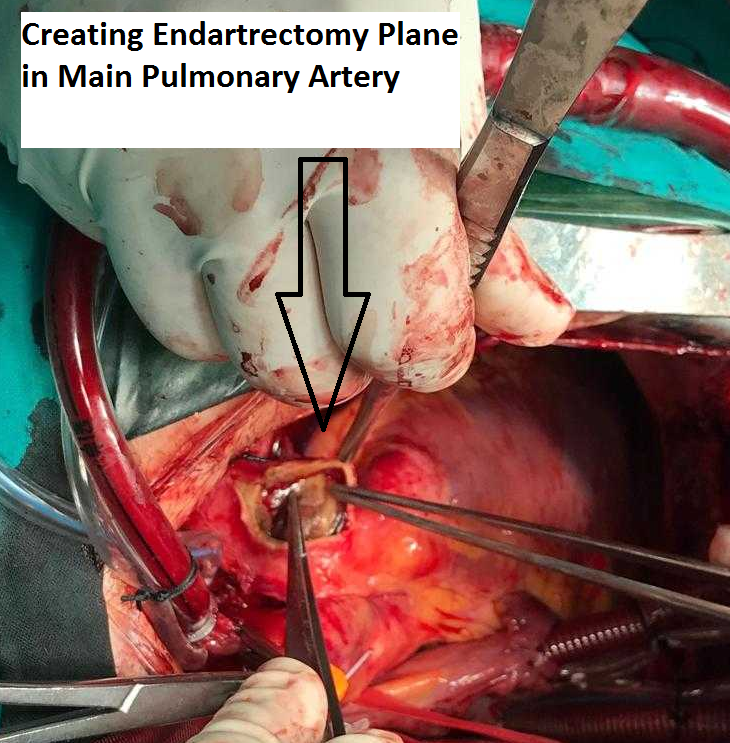
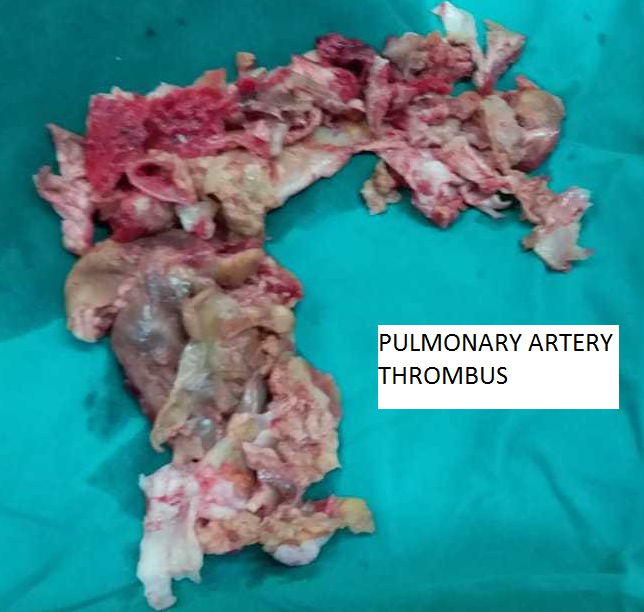
After arresting the heart, the main pulmonary artery was opened and the incision was advanced to the left pulmonary artery (LPA). An endarterectomy plane was created (Figure 6), and the thrombus was circumferentially followed to the branches of LPA. The thrombus was extracted from the branches of the pulmonary arteries using gentle tension. The RPA incision was then extended posteriorly to the aorta and under the SVC. For this part of the procedure, the surgeon was standing on the left side of the patient. After creating the plane circumferentially, the thrombus was lifted and followed to the branches of the RPA. Saline irrigation was used to flush all the branches of pulmonary artery, and all debris was removed (Figure 7). The pulmonary valve and RV outflow tract were spared from the thrombus. The pulmonary artery was primarily closed. The patient was weaned off after adequate de-airing. The patient was decannulated and the incision was closed in a standard fashion.
The patient had an uneventful recovery and discharge. He was started on anticoagulation postoperatively, and continued on oral anticoagulation and medical treatment for pulmonary hypertension.
References
- Jaff MR, McMurtry MS, Archer SL, et al; American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; American Heart Association Council on Peripheral Vascular Disease; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension: a scientific statement from the American Heart Association. Circulation. 2011;123(16):1788-1830.
- Klok FA, van Kralingen KW, van Dijk AP, Heyning FH, Vliegen HW, Huisman MV. Prospective cardiopulmonary screening program to detect chronic thromboembolic pulmonary hypertension in patients after acute pulmonary embolism. Haematologica. 2010;95(6):970-975.
- Guérin L, Couturaud F, Parent F, et al. Prevalence of chronic thromboembolic pulmonary hypertension after acute pulmonary embolism. Thromb Haemost. 2014;112(3):598-605.
- Fedullo PF. Chronic thromboembolic pulmonary hypertension: medical treatment. https://www.uptodate.com/contents/chronic-thromboembolic-pulmonary-hypertension-medical-treatment. Updated February 15, 2018. Accessed December 10, 2018.