ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Surgical Stabilization of Severe Flail Chest
Patient Selection
Flail chest complicates about 10% to 20% of patients with blunt chest trauma and is associated with a mortality rate ranging from 10% to 35% [1-4]. The management of severe flail chest has gradually changed over years, as a consequence of improved ventilatory techniques and better understanding of the pathophysiology of the complex traumatic acute respiratory failure syndrome. At present, it is widely accepted that respiratory impairment in flail chest patients is only partially due to inefficient ventilation related to the paradoxical movement of the chest wall, but is significantly influenced by other associated thoracic injuries, in particular pulmonary contusion and atelectasis [1,5]. In the last decade, the mainstay of treatment of severe flail chest has shifted from the treatment of the flail segment to the management of associated thoracic injuries with particular attention to pulmonary contusion [5].
Internal pneumatic stabilization with mechanical ventilation is the standard treatment for patients with flail chest and respiratory failure, or when associated head and/or abdomen injuries require mechanical ventilation [1,5]. Even though volume-limited ventilation has reduced mortality of patients with severe flail chest [2], ventilator-associated pneumonia often occurs after prolonged ventilation [6].
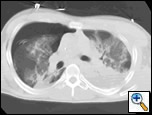
Although surgical management of patients with severe flail chest is at present controversial, we think that surgical stabilization is strongly indicated in specific clinical situations. The effectiveness and the ideal timing of chest wall stabilization in patients on mechanical ventilation is related to the degree of the pulmonary parenchymal damage [7,8]. The presence of extensive pulmonary contusion (Figure 1) is a relative contraindication to surgical stabilization. These patients require prolonged ventilation, and an early surgical stabilization would not provide benefit [7,8]. However, a surgical procedure can be proposed if the patient fails to wean from the ventilator once a partial resolution of pulmonary contusion is achieved [9,10].
In patients with isolated blunt chest trauma who have severe flail chest without significant pulmonary contusion, prolonged internal pneumatic stabilization is not suitable because of the risk of ventilator-related infectious complications. Moreover, mechanical ventilation is not always successful in preventing chest wall deformities that may result in a subsequent respiratory restrictive dysfunction [10,11]. In patients with mild or no pulmonary contusions (Figure 2), early surgical stabilization (within few days of internal pneumatic stabilization) may result in shorter intensive care unit stay with lower morbidity and prevention of pulmonary restrictive complications resulting in working incapacity [9].
Another indication for surgical stabilization is the presence of an extensive antero-lateral flail chest in a young patient even in the absence of severe respiratory failure. The primary end point for this clinical situation is the prevention of late chest restriction due to an anatomically deformed spontaneous stabilization. Surgical stabilization of a flail chest is also mandatory when the trauma patient is undergoing a thoracotomy for associated thoracic lesions. In this situation, chest wall stabilization does not add significant surgical morbidity.
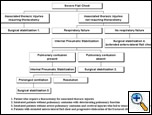 |
| Figure 3.: Algorithm for the treatment of severe flail chest. |
As proposed by other authors [7-9], we recognize the following clinical situations in which the surgical stabilization of a flail chest is indicated:
- Patient who require a thoracotomy because of associated thoracic injuries;
- Patients with deteriorating pulmonary function despite aggressive clearance of bronchial secretions and adequate analgesia, requiring internal pneumatic stabilization and without pulmonary contusion (candidates for early surgical stabilization);
- Intubated patients with previous severe pulmonary contusion and cerebral injuries, in order to reduce the duration of internal pneumatic stabilization when the patient fails to wean from the ventilator;
- Patients with extensive antero-lateral flail chest and progressive dislocation of the fractured ribs in order to prevent late chest wall deformity and a consequent restrictive disorder.
The algorithm in Figure 3 summarizes the indications to surgical stabilization of severe flail chest.
Operative Steps
Anesthesia
Surgical stabilization of a flail chest is performed under general anesthesia with a double lumen endotracheal tube in order to obtain a selective pulmonary exclusion that allows exploration of the pleural cavity and lung parenchyma.
Position of the patient and incisions
 |
| Figure 4. Surgical incision for an antero-lateral flail chest. |
The position of the patient and surgical incisions are related to the flail chest location. Antero-lateral flail chest injuries are approached with an antero-lateral thoracotomy with the patient in a supine position with both arms abducted 90 degrees. For pure lateral flail chest, we prefer a lateral thoracotomy, with the patient in lateral decubitus position and the arms abducted 90 degrees on a rest and carefully padded. Incisions are conducted over the fractured area. Surgical incisions must be large enough to allow a good exposure of all fractured ribs (Figure 4). We generally try to avoid significant muscle division in order to preserve respiratory function as much as possible. The serratus anterior muscle insertions on the chest wall are generally the only muscle fibers that are divided for anterolateral injuries. For lateral chest wall injuries the anterior aspect of latissimus dorsi is dissected.
Before starting with the stabilization of the chest wall, a thoracotomy in the middle of the flail segment is performed and the pleural cavity and lung parenchyma are explored. Fluid or partially clotted hemothoraces are adequately drained. Pulmonary lacerations are sutured. Associated pulmonary parenchymal lesions are treated in a conservative way whenever possible. Only largely destroyed lobes or segments are resected.
Osteosynthesis
The primary end point of surgical stabilization of a flail chest is the resolution of the paradoxical movement of the involved chest segments. Whenever it is possible, both fracture lines of a double fractured rib are fixed. This achieves optimal chest wall stabilization. The fixation of all fractures sites is mandatory in cases of flail chest with substantial dislocation of the chest wall. However, for less extensive flail segments, a physiological stabilization of the chest wall can be obtained with the fixation of only one fracture line for each involved rib (conversion from double fractured to single fractured rib). The fixation of posterior fracture sites is less important for chest wall integrity than is fixation of the anterior ones. The exposure of posterior fracture lines is also more challenging because of the presence of large muscle fibers (latissimum dorsi, trapezius, rhomboids, paraspinous muscles). Osteosynthesis should be conducted in a centripetal way, from the more distant fractured ribs to the ones immediately above and below the thoracotomy space. Fractured ribs from T4 to T10 are always fixed when involved. We do not routinely fix ribs between T1 and T 3 because of the risk of injury of subclavian vessels. T11 and T12 are never fixed because they are not involved in significant paradoxical movement.
The ribs that are to be fixed are adequately exposed in order to obtain a good placement of the metal fixation plates. When fractured ribs are exposed (Figure 5), the more dislocated segments are manually reduced. Excessive skeletization of the target ribs, that would increase the risk of pseudarthrosis and significant respiratory compromise, should be avoided. For these reasons, intercostal muscles are dissected only in the site where metal plates will be placed, trying to preserve as many intercostal muscles fibers as possible. Maximal care is taken to avoid stripping periosteum from the ribs.
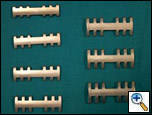
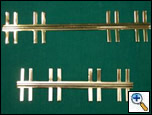
Once both ends of a fracture line are exposed, osteosynthesis is accomplished with metal plates. Judet plates (Cremascoli & Iris®, Milano, Italy) [12] are the most frequently used in our experience. These plates have lateral hooks at different angles on each side. They are available in different length and sizes, in order to be adapted to every fracture site and size (Figure 6). When the two rib ends are adequately reduced, a Judet plate of proper dimension is placed over the fracture line and anchored with the metallic hooks to each fracture segment (Figure 7). The more angled hooks are anchored to the inferior edge of the rib. The metal hooks are grasped with suitable forceps (Figure 8). Angled forceps are useful to anchor plates deep in the surgical field, such as the posterior fracture line of a lateral flail chest. Judet plates are ideal for simple fractures in which the two rib segment are conserved and they can be adequately reduced. In case of comminuted fractured ribs with loss of chest wall integrity, we prefer Sanchez-Lloret plates (Figure 9; no manufacturer’s name or location currently available) [13]. These plates are ideal when chest wall continuity must be restored (Figure 10). The length of the plates and the metal hooks must be carefully chosen to adapt to the rib size. Sanchez-Lloret plates are secured to the rib segment stretching the lateral hooks as previously described for Judet plates. Once a metal plate is placed, it is reinforced with a heavy adsorbable polyfilament suture at each anchoring site.
Drain placement and closure
The pleural cavity is routinely drained with two or three chest tubes. We generally put one or two 32 Fr chest drains in the lower hemithorax, and one 28 Fr tube directed to the apex. A smaller tube is generally placed in subcutaneous region (Figure 11).When closing the interspace of the thoracotomy, particular care must be taken not to displace the metal plates on the fixed rib on either side of the interspace. Two non-absorbable sutures are passed under the two ribs. The surgeon and the assistant should pull the sutures tight at the same time to avoid rib dislocation. When the chest wall is closed, the muscles and skin are sutured in the usual manner.
Postoperative course
Patients who undergo surgical fixation of a flail chest should be gradually weaned from the ventilator in order to prevent early displacement of the fixed ribs. In our experience mechanical ventilation is usually continued for 36 to 48 hrs postoperatively. The patient is discharged after radiographs (Figure 12) show resolution of traumatic pleuro-pulmonary injuries and after clinical evaluation demonstrates the absence of paradoxical movement of the chest wall. The metal plates do not need to be removed after healing has occurred.
Preference Card
- General anesthesia with double-lumen endotracheal tube
- Judet plates of different size and length
- Sanchez-Lloret plates of different length
- Grasping forceps with different angles
Tips & Pitfalls
- Use large skin incisions to expose all fractured sites but minimize muscle dissection to preserve pulmonary function
- All fractures of ribs 4-10 should be fixed; osteosynthesis of only the anterior fracture site of a double fractured rib is acceptable in certain circumstances.
- Intercostal muscles should be dissected only in the region where the metallic hooks of the plaques will be grasped. Maximal care is taken to preserve the periosteum.
- Judet plates are ideal if the two fractured rib segments can be easily reduced. Sanchez-Lloret plates are useful when comminuted fractures are present. Once a plate is fitted to the rib, the fixation should be secured with suture
- Care should be taken when closing the thoracotomy to avoid early displacement of fixed ribs.
Results
The optimal treatment for severe flail chest is far from standardized and many controversies still exist as to whether surgical stabilization and mechanical ventilation should be employed. The majority of studies reported in literature in this regard are retrospective and involve few patients [7-9,12-13,17]. From these uncontrolled studies it appears that surgical stabilization may provide an early restoration of chest wall contour and result in a significant reduction in the duration of ventilatory support. Mortality rates of 10% favorably compare to the reported overall mortality of flail chest patients. Moreover, long-term postoperative pulmonary function seems to be better preserved after surgical stabilization.
In the Division of Thoracic Surgery of the University of Modena and Reggio Emilia, from a total of 2974 blunt chest trauma victims, we have diagnosed 134 patients (4.5%) with flail chest. Severe flail chest requiring internal pneumatic stabilization and/or surgical stabilization was present in 79 patients. Twenty three were treated with internal pneumatic stabilization alone because of associated cerebral injuries or massive pulmonary contusions. In 56 patients surgical stabilization was performed with metal plates as described. Indications for surgical treatment were as follow: 13 patients required thoracotomy because of associated thoracic injuries; 12 non-intubated patients had a extended antero-lateral flail chest; 23 patients without pulmonary contusion presented with impaired pulmonary function despite a few days (median 3 days) of internal pneumatic stabilization (early surgical stabilization); 8 patients treated with internal pneumatic stabilization failed to wean from the ventilator after partial resolution of pulmonary contusion. The 30-day mortality for surgically treated patients was 5% (3/56 patients). The median intensive care unit stay was 6.5 days. Infectious complications occurred in 6% (4/56 patients). A satisfactory stabilization of the chest wall was obtained in all surgically treated patients. In the 23 patients treated with internal pneumatic stabilization alone, mortality was 37% (8/23 patients), the infectious complication rate was 44% (10/23 patients), and the median intensive care unit stay was 18 days.
The retrospective nature of our analysis does not allow us to compare the outcomes between different therapeutic strategies. However, we can assert that, when a surgical stabilization of a flail chest is performed in patients with mild or no significant pulmonary contusion, acceptable results in terms of intensive care unit stay, infectious complications, and resolution of paradoxical movement can be expected.
A randomized trial comparing surgical stabilization to conservative treatment in patients undergoing internal pneumatic stabilization has recently been published [16]. This study demonstrates that surgical stabilization using Judet struts reduces the incidence of nosocomial pneumonia, length of intensive care unit stay, and medical costs. Moreover, pulmonary function is favorably affected by osteosynthesis, which results in a quicker return to work. Even if some doubts can be raised concerning the methodology of this work (disparity in the number of patients of the two randomized arms, criteria for assessment of pulmonary contusion degree not clear), at present it is the only controlled study on the management of severe flail chest. We conclude that surgical stabilization of severe flail chest with metallic plates is a safe and effective therapy in properly selected patients.
References
- Davignon K, Kwo J, Bigatello LM. Pathophysiology and management of the flail chest. Minerva Anestesiol 2004;70:193-9.
- Beg MH, Reyazuddin, Ansari MM. Conservative management of flail chest. J Indian Med Ass 1990;88:186-187.
- Gaillard M, Herne C, Mandin, Raynaud P .Mortality prognosis factors in chest injury. J Trauma 1990;30:93-6.
- Ciraulo DL, Elliott D, Mitchell KA, Rodriguez A. Flail chest as a marker for significant injuries. J Am Coll Surg 1994;178:466-70.
- Gabram SG, Schwartz RJ, Jacobs LM, Lawrence D, Murphy MA, Morow JS, Hopkins JS, Knauft RF. Clinical management of blunt trauma patient with unilateral rib fractures: a randomized trial. World J Surg 1995;19:388-393.
- Campbell DB. Trauma to the chest wall, lung, and major airways. Semin Thorac Cardiovasc Surg 1992;4:234-240.
- Voggenreiter G, Neudeck F, Aufmkolk M, Obertacke U, Schmit-Neuerburg KP. Operative chest wall stabilization in flail chest: outcomes of patients with or without pulmonary contusion. J Am Coll Surg 1998;187:130-138.
- Richardson JD, Adams L Flint LM. Selective management of flail chest and pulmonary contusion. Ann Surg 1982;196:481-487.
- Lardinois D, Krueger T, Dusmett M, Ghisletta M, Gugger N, Ris HP. Pulmonary function testing after operative stabilization of the chest wall for flail chest. Eur J Cardiothorac Surg 2001;20:496-501.
- Tzelepis GE, McCool FD, Hoppin Jr FG. Chest wall distortion in patients with flail chest. Am Rev Respir Dis 1989;140:31-37.
- Fleming WH, Bowen JC. Early complications of long term respiratory support. J Thorac Cardiovasc Surg 1972;64:729-738.
- Ahmed Z, Mohyuddin Z. Management of flail chest injury: internal fixation versus endotracheal intubation. J Thorac Cardiovasc Surg 1995;110:1676-1680.
- Mouton W, Lardinois D, Ferrer M Regli B, Ris HB. Long-term follow-up of patients with operative stabilization of a flail chest. Thorac Cardiovasc Surg 1997;45:242-3.
- Judet R. Osteosynthesee costale. Rev Chir Orthop 1973;59 (suppl 1):334-5.
- Sanchez-Lloret J, Letang E, Calleja MA, Canalis E. indication and surgical treatment of the traumatic flail chest syndrome: an original technique. Thorac Cardiovasc Surg 1982:30:294-7.
- Tanaka H, Yukioka T, Yamaguti Y, Shimizu S, Goto H, Matsuda H, Shimazaki S. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma 2002;52:727-732.
- Balci AE, Eren S, Cakir O, Eren MN. Open fixation in flail chest: review of 64 patients. Asian Cardiovasc Thorac Ann 2004;12:11-5.