ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Transthoracic Repair Of Left-Sided Partial Anomalous Pulmonary Venous Connection
Partial anomalous pulmonary venous connection of the left upper lobe to a vertical vein is a rare congenital anomaly which can give rise to significant left-to-right cardiac shunting. We present the surgical technique employed in addressing this lesion through a left thoracotomy and include a video demonstration of the procedure.
Introduction
Partial anomalous pulmonary venous connections (PAPVC) are found in less than 1% of patients with congenital heart disease [1]. The classic description of the anomaly is a right upper lobe vein draining into the right atrium or superior vena cava in a young male patient with an atrial septal defect (ASD). [2,3]. In patients who present with an isolated PAPVC of the left upper lobe or entire left lung to a vertical vein, repair via a closed technique through a left thoracotomy is safe and effective.
Technique
Indications
Operative intervention has been recommended for A) the presence of symptoms or B) in an asymptomatic patient with a pulmonary to systemic flow ratio (Qp:Qs) greater than 1.5:1 or enlargement of right heart chambers, to decrease the likelihood of developing right heart failure or pulmonary vascular obstructive disease [4].
Pre-operative Investigations
A history and physical examination followed by a chest x-ray, electrocardiogram and complete transesophageal echocardiogram TEE is performed. Additional imaging with either computed tomography (CT) [5], magnetic resonance imaging (MRI), a ventilation perfusion scan or angiography [6] is warranted if there is uncertainty regarding the diagnosis, the anatomy or the co-existence of associated cardiac pathology.
Preparation
The patient is intubated with a double lumen endotracheal tube or a bronchial blocker to deflate the left lung, and is positioned on the operating room table with the left side elevated 30 degrees. The TEE probe is inserted to confirm the preoperative investigations and to assess all normal and anomalous pulmonary veins. The patient is prepared and draped in a sterile fashion, incorporating the left groin into the operative field.
Surgical Technique
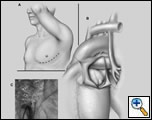
An anterolateral thoracotomy through the left fourth intercostal space is carried out with left lung deflated and a ratcheted retractor is placed (Figure 1A). The left vertical vein is exposed from the hilum to the innominate vein and any systemic tributaries are ligated and divided. The pericardium is opened posterior to the phrenic nerve and retracted anteriorly with 2-0 silk stay sutures (Figure 1B & C). After 5000 units per kilogram of heparin is given, the left pulmonary artery is exposed and is snared or clamped. A Satinsky clamp is placed just below the insertion of the vertical vein into the innominate vein and a small bulldog clamp is placed at least 4 cm proximally on the vertical vein (Figure 2A). The vertical vein is transected and the vertical vein-innominate confluence is repaired using 4-0 or 5-0 Prolene (Figure 2B). A side-biting clamp is placed at the base of the left atrial appendage, the tip of which is opened and the trabeculae trimmed. The sutured connection between the vertical vein and the opened appendage is planned using either an end to end (left upper lobe to vertical vein) or an end to side (left upper plus lower lobe to vertical vein) configuration. Stay sutures are placed at the superior and inferior margins, and the back wall of the anastomosis is created using a running 5-0 Prolene suture (Figure 2C). Stay sutures are removed and the anterior wall anastomosis is performed using interrupted stitches (Figure 2D). The clamp on the proximal vertical vein is removed and air is aspirated with fine needle, after which the left atrial appendage clamp and the left pulmonary artery clamps are removed in sequence (Figure 2E & F). The left lung is expanded. An invasive pressure monitoring line is used to measure the trans-anastomotic gradient. A gradient greater than 3 mm Hg warrants revision of the anastomosis. The pericardium is loosely approximated inferiorly but left open superiorly to prevent obstruction of the anastomosis. Two chest tubes are placed and the patient can be extubated as appropriate and sent to a cardiac surgical floor when stable.
Pitfalls
The co-existence of associated cardiac anomalies such as additional anomalous venous connections (particularly right-sided) or an ASD contraindicate use of the left thoracotomy approach.
Discussion
Most series have reported a prevalence of PAPVC of 0.4-0.7%, predominantly in children and young adults. These anomalies are usually right-sided (90%), with large shunts and associated atrial septal defect(s) (80-90%). A review of 45 children and adults from this institution, studied by transesophageal echocardiography, found that 82% of PAPVC originated from the right lung [6]. A recent retrospective study of adult chest computed tomography (CT) scans detected the presence of an asymptomatic PAVC in 0.2% of patients; which was left-sided in 79% and associated with an ASD infrequently (<3%) [5].
The physiologic effect of a PAPVC is the creation of a left to right shunt caused by drainage of one or more pulmonary veins either directly into the right heart, or via a systemic vein. The severity of symptoms correlates with the number of segments involved, the site(s) of connection, the presence of other pulmonary vascular abnormalities or associated cardiac defects [6,7]. Patients more frequently present with symptoms when associated anomalies are present and may require repair using cardiopulmonary bypass [7]. Those with an isolated PAPVC (without an ASD) of the left upper lobe to a vertical vein draining into the left innominate vein, can undergo safe and effective surgical correction via a closed approach utilizing a left thoracotomy.
References
- Healey J: An anatomic survey of anomalous pulmonary veins: their clinical significance. J Thoracic Surg 1952;23:433.
- Brody H: Drainage of the pulmonary veins into the right side of the heart. Arch Pathol 1942;33:221-240.
- Senocak F, Ozme, S, Bilgic, A: Partial anomalous pulmonary venous return-evaluation of 51 cases. Jpn Heart J 1994;35:43-50.
- Toyoshima M, Sato, A, Fukumoto, Y: Partial anomalous pulmonary venous return showing venous return to the azygos vein. Intern Med 1992;31:1112-1116.
- Haramati L, Moche I, Rivera V, Patel P, Heyneman L, McAdams H, Issenberg H, White C: Computed tomography of partial anomalous pulmonary venous connection in adults. J Comput Assist Tomogr. 2003;27:743-9.
- Ammash N, Seward J, Warnes C: Partial anomalous pulmonary venous connection: diagnosis by transesophageal echocardiography. J Am Coll Cardiol 1997;29:1351-1358.
- Friedman W, Congenital heart disease in infancy and childhood, in Heart Disease: A Textbook of Cardiovascular Medicine, E. Braunwald, Editor. 1992, WB Saunders: Philadelphia. pp887–965.