ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Uniportal Left Upper Trisegmentectomy (S1+2+3)
del Campo J, Galvez Munoz C, Maroto S, et al. Uniportal Left Upper Trisegmentectomy (S1+2+3). December 2019. doi:10.25373/ctsnet.11116700.
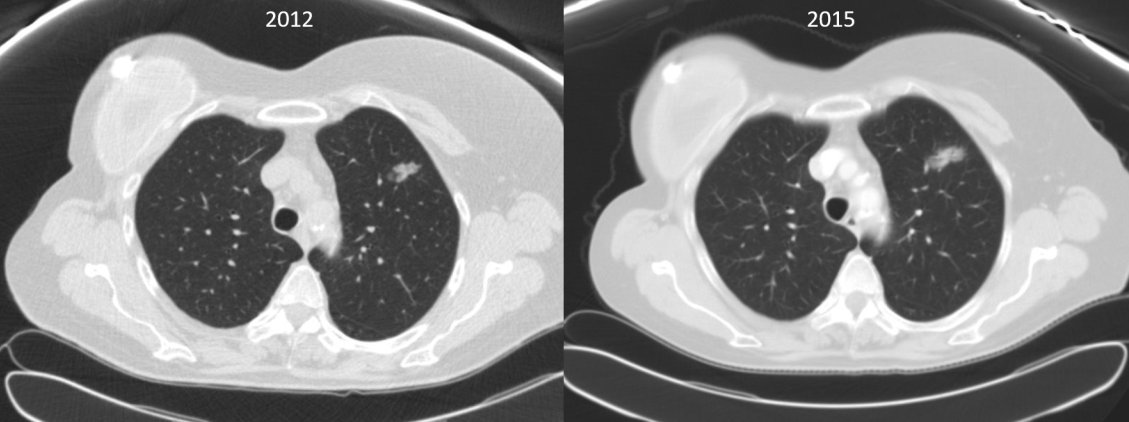
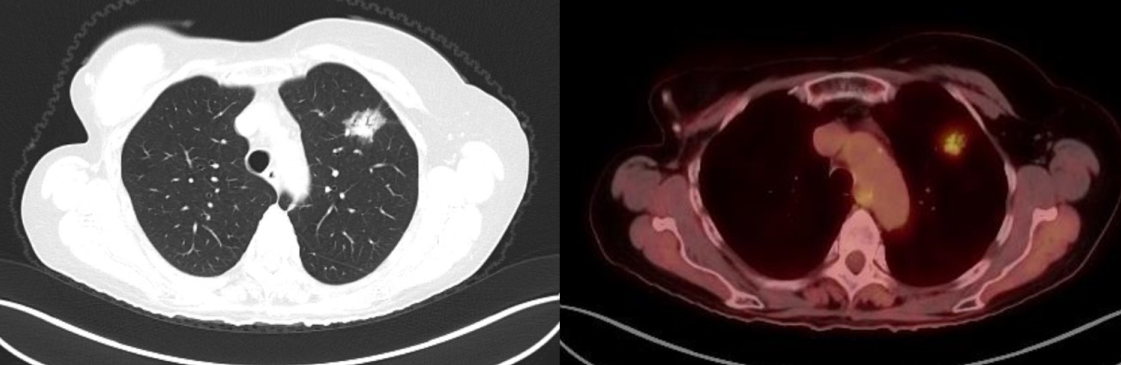
A 70-year-old woman with a past history of breast cancer in 2004 also had a nonperipheral pseudonodular ground glass appearance lesion in the left upper lobe since 2010, a core-needle biopsy in 2012 and 2015, and a diagnosis of benign pneumocytoma (Figure 1). Since 2018, the lesion had a growth of the solid component in chest computed tomography scan, so a positron emission tomography scan was performed, which showed an increased metabolic uptake in the lesion (SUV max 2.77) (Figure 2).
Figure 1
Figure 2
With the suspicion of malignant growth within the lesion (probable lepidic adenocarcinoma), a sublobar anatomical resection was indicated to avoid a left upper lobectomy.
In 2019, a left apical trisegmentectomy preserving lingula was performed through a 4 cm incision placed in the fifth left intercostal space, under intercostal blockade, in 120 minutes, as described in the video. All of the arterial branches were divided using endoscopic clips and bipolar advanced energy. An intraoperative frozen section reported a benign lesion without evidence of malignancy. With moderate suspicion of malignancy in the final exam, the authors performed a systematic lymphadenectomy.
There was no postoperative air leak, and the chest tube was removed during the first postoperative day. The patient was discharged on the second postoperative day with normal chest x-ray (Figure 3). Final pathologic exam reported a 2.1 cm lepidic adenocarcinoma with free margins, and all the lymph nodes were negative for malignancy, so the final pathologic stage was pT1cN0-IA3.
Sublobar anatomical segmentectomies are indicated for specific early stage primary lung cancer, as well as pulmonary metastasis and some benign conditions. The main benefits are preserving more lung parenchyma and decreasing postoperative complications. These procedures can be performed by dividing segmental pulmonary vessels with endoscopic clips and advanced energy devices, thus safely avoiding the use of many vascular endostaplers. Preserving lingual in apical left upper lobe lesions compares to performing right upper lobectomies preserving the middle lobe. Experience and segmental anatomical knowledge are mandatory for these procedures in order to avoid complications. Uniportal VATS is a safe and barely invasive approach for these resections and combines a less invasive surgical approach with a lung-sparing procedure.
References
- Bao F, Ye P, Yang Y, Wang L, Zhang C, Lv X, et al. Segmentectomy or lobectomy for early stage lung cancer: a meta-analysis. Eur J Cardiothoracic Surg. 2014;46(1):1–7.
- Liu Y, Huang C, Liu H, Chen Y, Li S. Sublobectomy versus lobectomy for stage IA (T1a) non-small-cell lung cancer: a meta-analysis study. World J Surg Oncol. 2014;12(1):138.
- Dziedzic R, Zurek W, Marjański T, Rudzinski P, Orlowski TM, Sawicka W, et al. Stage I non-small-cell lung cancer: long-term results of lobectomy versus sublobar resection from the Polish National Lung Cancer Registry. Eur J Cardiothoracic Surg. 2017;52(2):363–369.
- Gossot D, Lutz J, Grigoroiu M, Brian E, Sequin-Givelet A. Thoracoscopic anatomic segmentectomies for lung cancer: technical aspects. J Vis Surg. 2016;2:171.






Comments