ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Video-Assisted Thoracoscopic Lobectomy for Giant Congenital Bulla of the Left Upper Lobe: A Case Report
Trong VT, Le Quang T, Trong LK, Hoang HN. Video-Assisted Thoracoscopic Lobectomy for Giant Congenital Bulla of the Left Upper Lobe: A Case Report. August 2019. doi:10.25373/ctsnet.9693596.
A 17-year-old woman was admitted to the authors’ hospital with left chest pain, cough, and dyspnea. Computed tomography (CT) scan showed a giant bulla of the left upper lobe. Lobectomy was performed with video-assisted thoracic surgery (VATS). After the operation, the patient was stable, and chest CT showed good expansion of the left lower lobe. Pathological result showed a cyst lesion of the lung. VATS lobectomy is a safe and effective technique to approach young patients with a giant congenital bulla.
Background
A bulla is an emphysematous area with extensive destruction of lung tissue producing an airspace bigger than 1 cm in diameter. A giant bulla is defined as a bulla occupying at least one-third of the hemithorax (2). Bullae are associated with malignancy and can cause a pneumothorax (9). Because giant bullae do not participate in oxygen exchange and often compress the surrounding normal lung parenchyma, they can cause chest pain, cough, dyspnea, and infection.
Computed tomography is the important preoperative evaluation because it can evaluate the quantity, location, and size of bullae, as well as the quality of the surrounding lung tissue. CT also allows for the evaluation of coexisting problems such as bronchiectasis, coinfected cysts, pulmonary artery enlargement, and pneumothorax (5, 3, 10).
Surgery is indicated on a preventive basis when lesions occupy more than one-third of the hemithorax, when there is a compression of healthy adjacent lung tissue, and when the size of a bulla shows to have increased at follow-up. It is also indicated for patients who have complications related to bullous disease, such as infection or pneumothorax (3). Surgery for resection of giant bullae is an effective procedure for improving airflow, limiting gas exchange, and limiting exercise dynamic hyperinflation over time (6, 7). Video-assisted thoracic surgery is chosen for the treatment of the giant bulla because the patients have quicker recovery and less pain compared to thoracotomy (3).
The authors present a case of a young patient with a giant congenital bulla that was successfully treated with VATS lobectomy.
Case Presentation
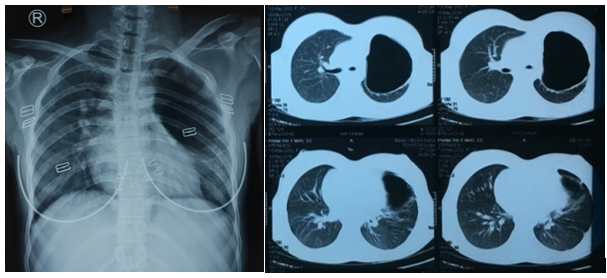
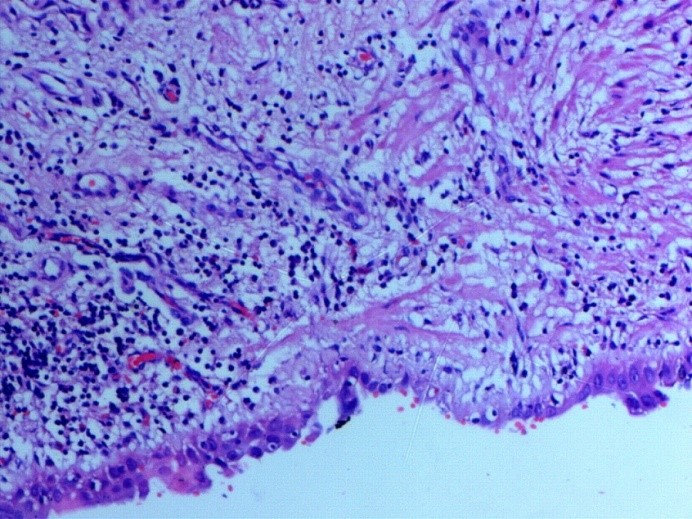
Figure 1. Chest x-ray and CT scan showing a giant bulla of the left upper lobe with compression of the remaining lung parenchyma.
A 17-year-old woman was admitted to the Thoracic Surgery Department of Da Nang Hospital in Vietnam with left chest pain, cough, and dyspnea. The medical history of this patient revealed a persistent cough for several months when she was 10 years old. Physical examination demonstrated decreased breath sounds in the left thorax. There were no other abnormal clinical findings. A routine chest x-ray and computed tomography confirmed the presence of a giant bulla of the left upper lobe (Figure 1).
The patient underwent VATS left upper lobectomy. Surgery was performed under general anesthesia with double lumen endotracheal intubation and single lung ventilation. The patient was positioned in the right lateral position. First the authors divided the lesion from the chest wall and mediastinum, which was very difficult due to adhesions between the chest wall and the left upper lobe. They then transected the branches of the upper lobe pulmonary artery. Following this, they transected the left upper lobe vein; they didn't transect the vein first because it could lead to vascular engorgement and increased bleeding. Finally, they transected the left upper lobe bronchus. After completion of the fissure, the left upper lobe was extracted (Figure 2). The total operative time was around 2 ½ hours.
After the operation, the patient was stable. A postoperative chest CT scan showed good expansion of the left lower lobe. Pathological result showed a cystic lesion of the lobe (Figure 3). The patient was discharged five days after surgery.
Discussion
There are various methods for treating giant bullae, such as thoracoscopic endoloop ligation, intracavitary bulla drainage, laser bullous ablation, bullous fibrin glue treatment, the Brompton technique, VATS bullectomy, etc (11). Currently, VATS is considered a suitable and effective surgical technique for treating giant bullae (4).
Bullectomy is appropriate when the bulla is large and is causing compression collapse of the neighboring lung. Lobectomy can be considered when the bulla occurs either in or adjacent to a bronchiectatic lobe (1). Better results are obtained in patients in whom plication or bullectomy can be performed compared to those requiring lobectomy (8). In this case, the giant bulla occupied the entire left upper lobe and compressed the surrounding normal lung parenchyma. It was also adjacent to bronchiectatic tissue, so the authors decided a lobectomy including the giant bulla with VATS was more suitable than bullectomy.
Bullae are associated with malignancy and can cause a lot of complications, such as pneumothorax and infection (9). In the authors’ study, pathology showed a cystic lesion of the lung. Lobectomy was indicated not only for treatment of the giant bulla, but also for the prevention of complications and malignant transformation.
Some complications may occur during the postoperative period such as prolonged air leak, atrial fibrillation, the need for mechanical ventilation, pneumonia, etc. Postoperative prolonged air leak is one of the major causes that prolongs hospital length of stay and increases the opportunity of infection of the thoracic pleural space (2). In this case, no serious complications occurred in the postoperative course.
Conclusion
In the authors’ case, the entire left upper lobe had lost function owing to a congenital giant bulla. VATS with lobectomy was a safe and effective treatment.
References
- Allison PR. Giant bullous cysts of the lung. Thorax. 1947;2:169.
- Cui Y, Yin Y, Song R, Tang T, Li F, Zhou Y. Video-assisted thoracoscopic lobectomy of a giant bulla: a case report. Clin Surg. 2016;1:1098.
- Greenberg JA, Singhal S, Kaiser LR. Giant bullous lung disease: evaluation, selection, techniques, and outcomes. Chest Surg Clin N Am. 2003;13(4):631-649.
- Menconi GF, Melfi FMA, Mussi A, Palla A, Ambrogi MC, Angeletti CA. Treatment by VATS of giant bullous emphysema: results. Eur J Cardiothorac Surg. 1998;9(1):66–70.
- Morgan MDL, Strickland B. Computed tomography in the assessment of bullous lung disease. Br J Dis Chest. 1984;78(1):10-25.
- Neviere R, Catto M, Bautin N, Robin S, Porte H, Desbordes J, et al. Longitudinal changes in hyperinflation parameters and exercise capacity after giant bullous emphysema surgery. Thorac Cardiovasc Surg. 2006;132(5):1203.
- Palla A, Desideri M, Rossi G, Bardi G, Mazzantini D, Mussi A, et al . Elective surgery for giant bullous emphysema: a 5-year clinical and functional follow-up.Chest. 2005;128(4):2043.
- Potgieter PD, Benatar SR, Hewitson RP, Ferguson AD. Surgical treatment of bullous lung disease. Thorax. 1981;36:885-890.
- Roemers R, Patberg K, van de Wauwer C, Nguyen T, Shahin G. Robot-assisted thoracoscopic lobectomy as treatment of a giant bulla. J Cardiothorac Surg. 2017;12:31.
- Sharma N, Justaniah AM, Kanne JP, Gurney JW, Mohammed TL. Vanishing lung syndrome (giant bullous emphysema): CT findings in 7 patients and a literature review. J Thorac Imaging. 2009;24(3):227-230.
- Urschel JD, Dickout WJ. Thoracoscopic intracavitary drainage for pneumothorax secondary to bullous emphysema. Can J Surg. 1993;9(6):548–550.