ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Combined Minimally Invasive Left-Sided Open Heart Surgery and Bypass Grafting Through Right Minithoracotomy
Introduction
The authors performed a combined atrial myxoma resection with bypass grafting, using a right minithoracotomy approach. The case demonstrates the feasibility of combined minimally invasive heart surgery procedures (MICS).
Case Report
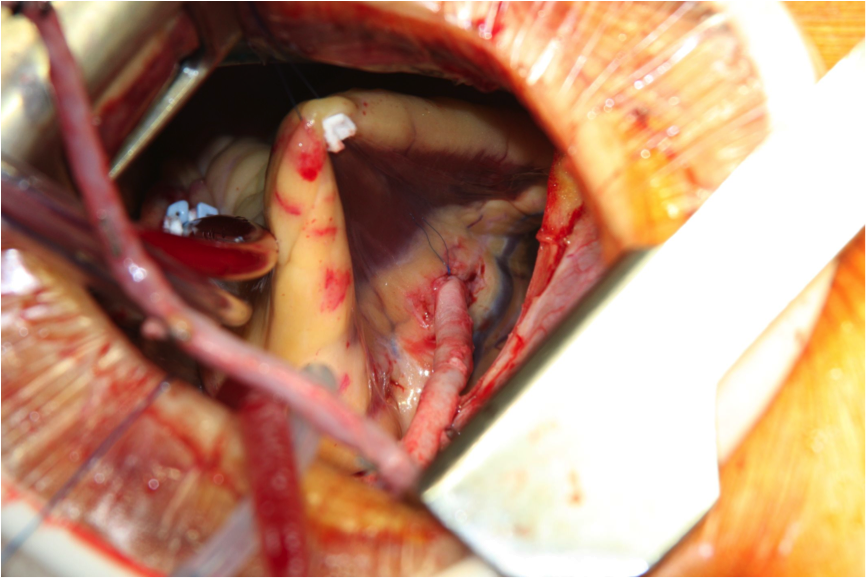
Figure 1: Following suspension of the RV acute margin. The visibility and access to the RCA through the right minithoracotomy is unobstructed and easy.
A 62-year-old patient presented to the community hospital with an incident of stroke and resulting dysphasia. Following a cardiac screening for the source of the event, a large 3x5 cm, pedunculated, and largely mobile left atrial mass was detected by 2D echocardiography. The patient was scheduled for surgery soon after the mass was discovered. Three days prior to surgery, another stroke occurred with worsening dysphasia and speech incongruence. The authors made the decision to operate on the patient immediately. Routine preoperative angiography revealed a 70% stenosis of the mid-portion of the right coronary artery (RCA), and right dominant pattern. The procedure was planned in a minimally invasive fashion via right minithoracotomy.
Femoral cannulation was carried out using 20 Fr arterial and 22 Fr venous multistage cannulas. A right minithoracotomy measuring 6 cm was performed, with an anterior orientation, reaching from the anterior axillary line to the mid-clavicular line. Following exposure, as described by Glauber, the aorta was cross-clamped using the Chitwood clamp and custodiol cardioplegia was given (1). Core temperature was maintained at 32 degrees C. The left atrium was opened and the main bulk of the LA mass (a myxoma, confirmed by histology) was removed under meticulous suction. The stalk was broadly based and was excised along with a 5x10 mm piece of interatrial septum at its base. The defect was closed primarily. Next, the atriotomy was closed using 3.0 Prolene suture. The acute margin of the RV was suspended on a pledgeted 4-0 Prolene suture and pulled towards the work-incision and then out. This helped to lift the RV very comfortably, and provided excellent access to the entire length of the RCA and posterior descending artery (PDA). A 15 cm saphenous vein was previously harvested in an endoscopic fashion. The authors proceeded with the distal anastomosis first, using 7-0 Prolene, followed by the proximal anastomosis on the still-arrested heart and cross-clamped aorta. Following re-warming, the heart was de-aired both through the LA (vent) and the aorta (punched aortic orifice for the graft anastomosis), the cross-clamp was released, and the suture completed. The heart resumed immediate sinus rhythm and good contractility. The saphenous graft flow was measured to be over 60 ml/min via MiraQ™ Cardiac (Medistim, Norway). On intraoperative, post-procedural echocardiography there was no ASD and good ubiquitous contractility. The total cross-clamp time was 75 minutes.
The patient was extubated a few hours later and no additional neurological deficits were found. He was fully mobile and recovered when he was discharged on the fourth postoperative day.
Discussion
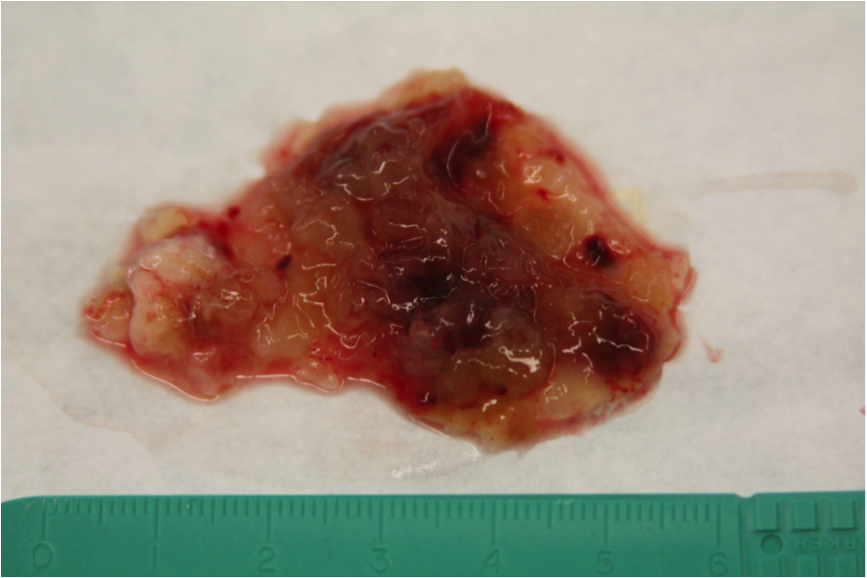
Figure 2: Removed myxoid left atrial mass measuring 5x3 cm.
Combined procedures have long been a deterrent to proceeding with a minimally invasive approach. While some double valve surgery, such as mitral and tricuspid valve, is now increasingly being reported, a concurrent heart-valve or left-sided open heart procedure and bypass grafting have only been anecdotally reported (2, 3). With novel technology and advances in the surgical armamentarium, the modern cardiac surgeon is more daring in addressing the full cardiac pathology. Many such procedures, mostly surgical valve procedures and same-stop coronary interventions, are being reported as hybrid cases executed in the same session by the cardiologist and heart surgeon (4, 5). These procedures have been facilitated by better-quality new generation stents and more specific anticoagulation regimens within the operation theater, such as pre-incision administration of Clopidogrel to provide stent protection following reversal of Heparin by the surgeon. This was not necessary in this particular case, as the bypass graft was planned on the RCA. The authors were encouraged by the ease of access to the entire length of the RCA and RPDA on the arrested (vacuum-assisted), evacuated heart. Normal anastomotic instruments were utilized.
The authors presume that more complex and extensive concomitant procedures can be accomplished through a somewhat anteriorized minithoracotomy, for better access to the coronary tree. Upon positional testing, the authors were also able to twist the heart towards the surgeon so as to be able to visualize the LAD. While such combined procedures are not common, and rather likely to stay low in number and be surpassed by same-stop, valve-PCI hybrid procedures, they can be possible in patients who are potential candidates.
One limitation to this surgery is extreme anatomy. This is not rare in Asia, where there are a large number of very flat-chested patients with verticalized hearts, which tend to flip over the spine to the left hemithorax upon evacuation. This renders the entire minimally invasive approach extremely difficult. Advanced coronary disease, with diffuse stenotic pattern or very small targets, may not be amenable for the above combined approach either.
As a committed minimally invasive and hybrid cardiac surgery team, the authors’ envision and expect more combined and hybrid procedures to develop, offering the patient complete treatment of all cardiac pathologies.
References
- Glauber M, Karimov JH, Farneti PA, Cerillo AG, Santarelli F, Ferrarini M, Del Sarto P, Murzi M, Solinas M. Minimally invasive mitral valve surgery via right minithoracotomy. Multimedia Man Cardiothorac Surg doi: 10.1510/mmcts.2008.003350
- Santana O, Pineda AM, Cortes-Bergoderi M, Mihos CG, Beohar N, Lamas GA, Lamelas J. Hybrid approach of percutaneous coronary intervention followed by minimally invasive valve operations. Ann Thorac Surg. 2014 Jun;97(6):2049-55.
- Smit PJ, Shariff MA, Nabagiez JP, Khan MA, Sadel SM, McGinn JT Jr. Experience with a minimally invasive approach to combined valve surgery and coronary artery bypass grafting through bilateral thoracotomies. Heart Surg Forum. 2013 Jun;16(3):E125-31.
- Umakanthan R, Leacche M, Petracek MR, Zhao DX, Byrne JG. Combined PCI and minimally invasive heart valve surgery for high-risk patients. Curr Treat Options Cardiovasc Med. 2009 Dec;11(6):492-8.
- Schroeyers P, Farhat F, Van Praet F, Vermeulen Y, Vanermen H. Video-assisted Port-Access combined mitral valve and CABG surgery. J Heart Valve Dis. 2000 Nov;9(6):783-5.





Comments