ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
COVID-19: Safe Thoracic Surgery
Barr J, Internullo E, West D, Krishnadas R, Batchelor T, Saftic I. COVID-19: Safe Thoracic Surgery. April 2020. doi:10.25373/ctsnet.12200786
Providing lung cancer surgery during the COVID-19 crisis presents many challenges. Cancer services must minimize exposure to health care workers and manage the higher risks associated with surgery during the pandemic, while also contending with reduced elective operating and intensive care capacity (1).
COVID-19 has proved to be highly infectious and has infected more people in a shorter time period than other coronavirus outbreaks (SARS-CoV and MERS-CoV) (2). The lungs are the primary organ affected by COVID-19, and transmission is caused by respiratory droplets, airborne transmission, and direct contact, making lung cancer surgery high risk for healthcare worker infection (2).
Guidelines from the British Thoracic Society advise consideration of stereotactic ablative radiotherapy (SABR) in patients with tumors under 2 cm and prioritizing surgical management for patients with higher stage cancers which are likely to become unresectable if treatment is delayed (3). The advice from NHS England is clear and states that essential and urgent cancer treatments must continue (4).
As well as the surgical risk of infection to health care workers, there is also the risk of aerosolization of the virus from a chest drain with an air leak. Anecdotal reports from other thoracic units suggest that this is a problem, with reports of entire wards being infected after a postoperative patient was found to have COVID-19. The authors are unaware of any specific guidance on chest drain management during the COVID-19 pandemic. Under normal working conditions, NICE recommends the use of Thopaz drains following lung resection. However, after contacting the manufacturer, these drains do not have a viral filter (5). Extrapolating advice from NHS England on ventilator circuits which should be protected by a high efficiency filter such as a heat and moisture exchange (HME) filters, the authors have developed a method of providing chest drainage with a viral filter (6). The authors have previously described the idea of the attachment of viral filters to Rocket bottles (7). In this article, the authors aim to improve it further and update on some of the pitfalls with this new set-up.
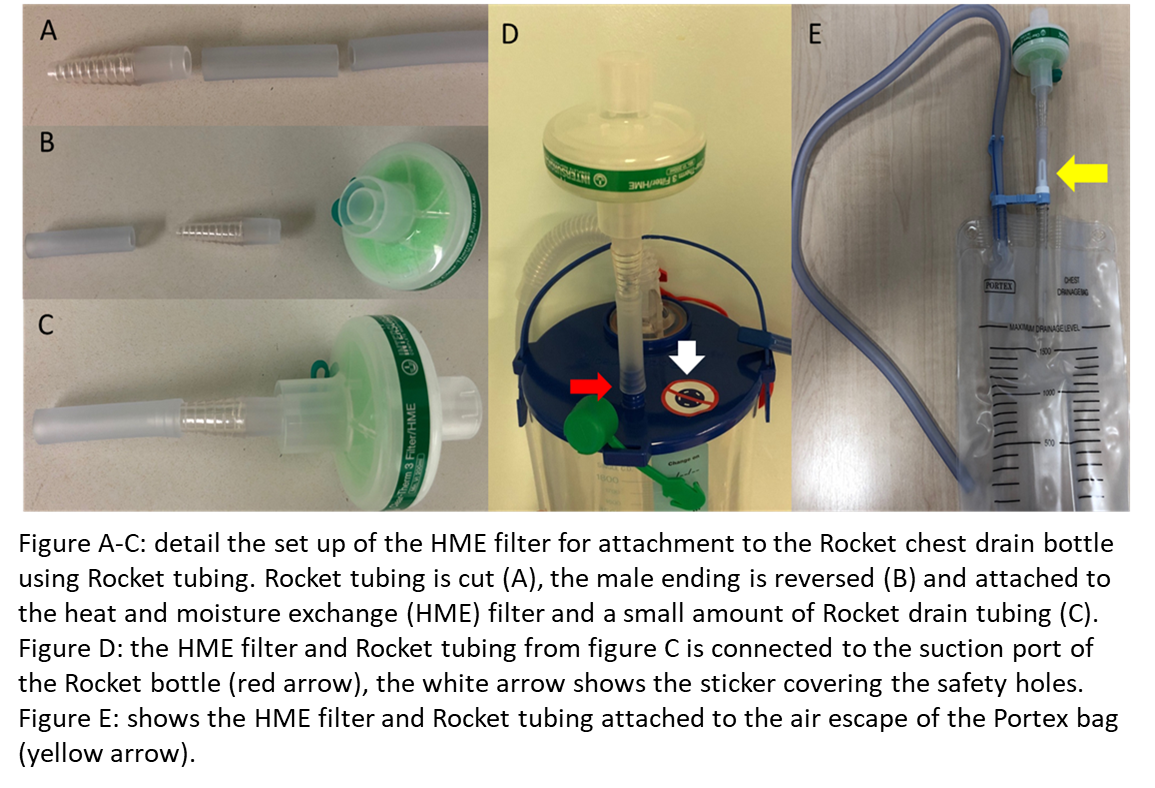
The set-up is simple and uses equipment that is easily available (Rocket bottle with tubing and a Therm 3 HME filter or alternatively a high efficiency heat filter [Figure 1]). In addition to the suction port, the Rocket bottle has additional safety holes that provide a mechanism for air to escape should the suction become blocked (Figure 1D). If the Rocket bottle is to be used with a viral filter, then these must be covered to prevent the virus being aerosolized through this lower resistance mechanism. This can be done easily with stickers which are provided with the bottle. However, covering these holes puts the patient at risk of developing a tension pneumothorax should the viral filter block or if attached incorrectly.
Checking the viral filter must be part of standard nursing checks for all patients with chest drains. The air leak is monitored and any sudden changes in air leak mandate a medical review. The authors have tested the resistance to flow of the HME filter on a ventilator up to a flow rate of 30 L/min, and even at this flow rate resistance is trivial. This has correlated with their clinical experience that the presence of a filter does not impede the air flow out of the chest in patients with air leaks as demonstrated by the chest radiograph showing no pneumothorax. Filters are changed daily as per manufacturer recommendation or sooner if there is any gross contamination. This is done wearing full personal protective equipment (PPE). Additionally, PPE is worn for changing Rocket bottles and for chest drain removal. The same filter system can also be applied to a Portex bag (Figure 1E), which aims to facilitate mobilization on the ward.
In addition to this chest drain management, the authors developed a number of ways of minimizing the risk of COVID- 19 transmission. Patients are admitted on the morning of surgery and immediately taken for a low dose computerized tomography (CT) scan of the chest as per guidelines from the Royal College of Surgeons (8). Chinese studies have shown that chest CT has sensitivity as high as 97% for COVID-19 detection (9). Even in asymptomatic patients with COVID- 19, CT abnormalities were found in 95% of cases (10). The authors aim to start taking viral swabs two days prior to surgery in addition to the CT scan in keeping with Royal College of Surgeons recommendations (11). Providing the CT scan is negative for COVID-19 changes, then the operation is performed with all theatre staff wearing full PPE. Every effort is made to minimize air leaks, intra-operatively lung tissue is stapled and air leaks assessed at the end of the case with underwater testing and repaired where possible. The chest drain is connected at the end of the procedure and the air leak is assessed, the viral filter is placed, and the safety holes are covered.
This multifaceted strategy allows the authors to continue to provide thoracic surgery during the COVID-19 crisis and minimize risks to patients and staff. Future work would be to ascertain the viral load in chest drains of COVID-19 patients who require chest drainage. This method serves as an interim method of lowering the risk of viral exposure to the other patients and staff in hospitals.
References
- Li YK, Peng S, Li LQ, Wang Q, Ping W, Zhang N, et al. Clinical and transmission characteristics of Covid-19 - A retrospective study of 25 cases from a single thoracic surgery department. Curr Med Sci. 2020 Mar 30.
- Meo SA, Alhowikan AM, Al-Khlaiwi T, Meo IM, Halepoto DM, Iqbal M, et al. Novel coronavirus 2019-nCoV: prevalence, biological and clinical characteristics comparison with SARS-CoV and MERS-CoV. Eur Rev Med Pharmacol Sci. 2020 Feb;24(4):2012-2019.
- Matthew Evison, Seamus Grundy, Simon Bailey, Richard Booton, Rajesh Shah, Neil Bayman, et al. Lung cancer and mesothelioma service guidance during the COVID‐19 pandemic. NHS England Clinical Expert Group on Lung Cancer.
- https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0119-_Maintaining-cancer-services-_-letter-to-trusts.pdf Accessed 3.4.20
- Thopaz+ portable digital system for managing chest drains
Medical technologies guidance [MTG37] Published date: 21 March 2018
https://www.nice.org.uk/guidance/mtg37. Accessed 3.4.20 - NHS England: Clinical management of persons admitted to hospital with suspected COVID-19 infection. Published https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/clinical-management-of-persons-admitted-to-hospita-v1-19-march-2020.pdf. Accessed 3.4.20
- Bilkhu R, Viviano A, Saftic I, Billè A. COVID-19: Chest drains with air leak – the silent ‘super spreader’?. CTSNet April 2020. https://www.ctsnet.org/article/covid-19-chest-drains-air-leak-%E2%80%93-silent-%E2%80%98super-spreader%E2%80%99. Accessed 13.4.20
- Intercollegiate guidance for pre-operative chest CT imaging for elective cancer surgery during the COVID-19 pandemic UPDATE | RCSEd. https://www.rcsed.ac.uk/news-public-affairs/news/2020/april/intercollegiate-guidance-for-pre-operative-chest-ct-imaging-for-elective-cancer-surgery-during-the-covid-19-pandemic-update. Accessed 18.4.20
- Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020 Feb 26:200642.
- Meng H, Xiong R, He R, Lin W, Hao B, Zhang L, et al. CT imaging and clinical course of asymptomatic cases with COVID-19 pneumonia at admission in Wuhan, China. J Infect. 2020 Apr 12. pii: S0163-4453(20)30211-5.
- Royal College of Surgeons Guidance on COVID-19. https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update. Accessed 21.4.20
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.




