ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
The Dark Side of the Aortic Valve
Introduction
Alkaptonuria is a rare genetic disorder of tyrosine metabolism (1). The most common clinical features are urine discoloration, tissue pigmentation, and ochronotic arthropathy. Less common manifestations include renal, urethral, and prostate calculi, and cardiovascular abnormalities, especially valvular disease (2). The authors present the case of a patient with alkaptonuria, diagnosed only during open heart surgery due to aortic stenosis.
Case Report
A 55-year-old female patient was referred for heart surgery due to aortic valve stenosis. She had a history of early onset spondyloarthropathy without any known etiology, despite a broad range of diagnostic tests. A bluish coloration of the sclera and ears was evident during a physical examination.
The pre-surgery echocardiogram revealed severe aortic stenosis (medium gradient = 79 mmHg, functional area = 0.6 cm2), left ventricular hypertrophy, and diastolic dysfunction. The coronary angiography showed no significant coronary disease.
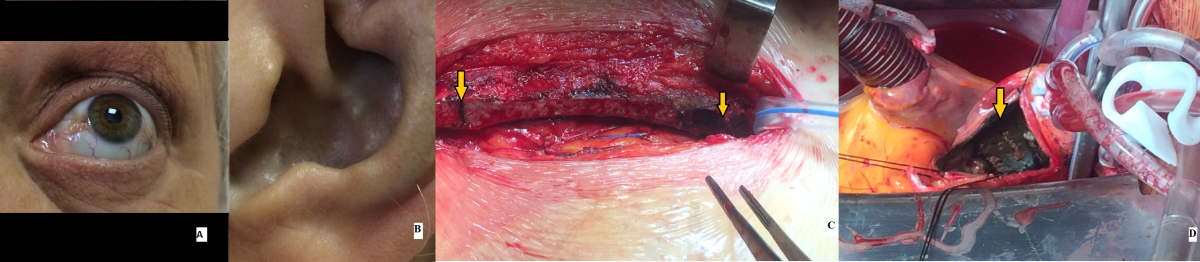
An operation was performed to replace the aortic valve with a mechanical valve prosthesis. After the sternotomy, darkening of the sternal joints was observed. After the aortotomy, intense calcification of the aorta was noted on palpation and dark pigment deposition on the whole interior aspect of the aortic wall was observed (Figure 1). Severe calcification and thickening of a three-leaflet aortic valve was found. The aortic valve cusps and mitral valve chords were discolored with a dark pigment. The procedure went on with standard techniques and no complications occurred during or after surgery.
Figure 1 – A: Bluish coloration of the sclera is evident. B: Bluish coloration of the ears. C, D: Surgical findings. C - Darkening of the sternum joints (arrows). D – The interior aspect of the aortic wall (arrow) is completely dark (ochronotic).
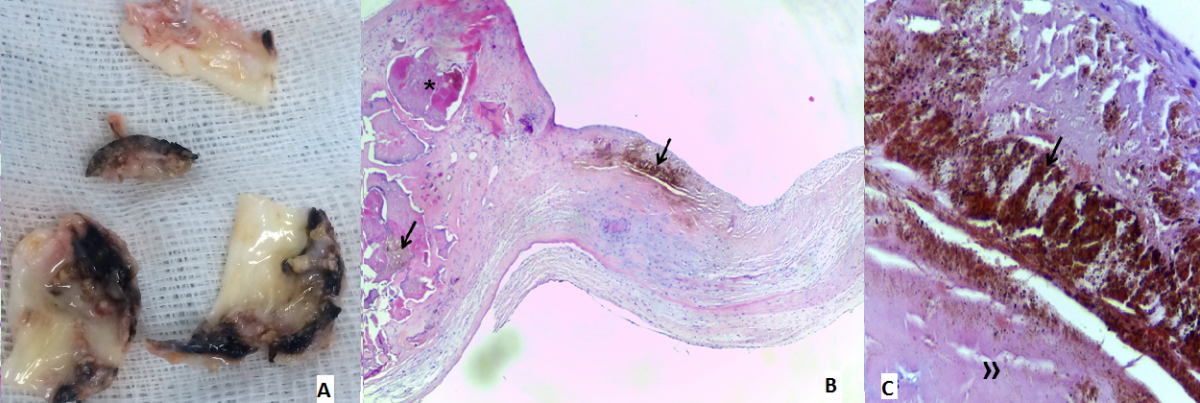
The histopathological examination described the cusps as having mainly “melanin-like” ochre-colored pigment extracellular deposits, possibly corresponding to oxidated homogentisic acid, as well as myofibroblastic proliferation and macrophages. The pigment deposits favored/induced fibrosis, deposition of acid mucopolysaccharides, and very prominent dystrophic calcification. Further characterization was performed using histochemical (including negative Prussian Blue staining) and immunohistochemical (negative S100 protein and HMB45 expression) techniques (Figure 2).
Figure 2 - A: Macroscopic aspect of the excised aortic valve. B, C: Histopathological features (light microscopy). B - Deformed aortic valve leaflet with abundant deposits of ochre-colored homogentisic pigment (arrow) and calcifications (*) [H/E x40]. C - High magnification of one pigmented (arrow) area and the underlying collagen (») [H/E x400].
The patient´s spinal X-Ray revealed calcification of the intervertebral disks and shortening of the intervertebral spaces. All of the findings pointed to alkaptonuria with ochronotic aortic valvulopathy. However, the urine test for homogentisic acid had a negative result.
Discussion
Alkaptonuria is a rare autosomal recessive genetic disorder that occurs with an incidence of 1 case in 250,000 – 1 million live births (3). It is a disorder of phenylalanine and tyrosine metabolism caused by deficiency in homogentisate 1, 2-dioxygenase (HGO) activity, an enzyme responsible for tyrosine degradation, normally present in the liver and kidney (2, 4). Homogentisic acid (HGA) accumulation and deposition in large amounts occurs as ochronotic pigment in several tissues and organs, causing bluish-black pigmentation and tissue injury (2).
The human HGO gene locus has been mapped to chromosome 3q21-q23.2. Alkaptonuria is characterized by a remarkable allelic heterogeneity that reflects the disorder’s clinical variability (2, 3).
The accumulation of HGA and its metabolites causes the classic clinical triad:
- Homogentisic aciduria presenting at birth, with the pathognomonic sign of urine darkening on standing when oxidized/alkalinized
- Gradual development of ochronosis after 20 years of age
- Degenerative ochronic arthropathies usually in the fourth decade of life (2).
Clinical manifestations of alkaptonuric ochronosis are usually delayed, because aging decreases homogentisic acid renal clearance. Ochronotic spondyloarthropathy is the most common serious complication, affecting large weight bearing joints. Radiographic changes with intervertebral cartilages calcification are typical and almost pathognomonic. The arthritis resembles, and may be confused with, osteoarthritis (2, 4).
Externally, ochronosis is manifested by ear cartilage and sclera pigmentation (4). Cutaneous features are considered as diagnostic hallmarks and should alert the clinician to look for further organ involvement (5).
Cardiovascular involvement is rare. Ochronosis has been associated with pigmentation of various cardiovascular structures including valves, endocardium, pericardium, arterial walls, and atherosclerotic plaques. Deposition of ochronotic pigment in the vascular endothelium probably leads to the initial injury responsible for atheroma and coronary artery disease genesis in this setting (1).
Valve disease preferentially occurs in middle age, as pigment accumulates and induces secondary lesions (mainly fibrosis and calcifications). Thus, the pathogenesis of aortic valve calcification and aortic stenosis is most likely related to the extensive extracellular deposits of ochronotic pigment (4). Pigment is usually more prominent at the valve cusp/leaflet base, extending into the valve annulus. The aortic valve has the highest incidence of calcifications and stenosis, followed by the mitral and pulmonary valves, but involvement of multiple valves may be observed (1).
The patient had a history of spondyloarthropathy, but it was only during aortic valve replacement that the diagnosis of alkaptonuria was first suspected, due to previously described surgical findings.
Presence of high levels of HGA in the urine, blood, and other tissues is the standard reference for diagnosis (5). Histopathological examination of the different affected tissues can be performed. However, it is neither necessary nor specific for the diagnosis, as the accumulated pigment is difficult to distinguish, namely from melanin and ferric pigment (5).
Although this patient had several clinical and pathologic characteristics of alkaptonuria, the urine levels of HGA were not elevated in two separate analyses performed in the same laboratory. No alternative diagnosis appeared to explain this patients´ pathology as alkaptonuria did. This may have been a case of false negative result (perhaps due to technical error or inappropriate handling of the sample), or a rare case of alkaptonuria with no HGA detection in urine. No similar results were found in literature.
Currently there is no specific and effective treatment for alkaptonuria. The aim of treating the alkaptonuric patient is to prevent/minimize vital complications. Alkaptonuria-associated arthritis is treated symptomatically (1, 2). In advanced cases, surgical replacement of joints and aortic valves result in significant improvement (2).
This patient underwent aortic valve replacement. She was under pharmacological control of joint pain.
Although no effective treatment for alkaptonuria exists, prognosis is relatively good (1). However, complications are unavoidable. Arthropathy may be severely debilitating, and cardiovascular or renal impairment can involve vital prognosis. Therefore, organ assessment and follow-up after the fourth decade of life are highly recommended (5).
In conclusion, cardiac ochronosis is a very rare disease. Nevertheless, cardiac surgeons and pathologists should be aware of it since they may be confronted with the typical signs during surgery and histopathological examination of excised specimens (1).
References
- Steger CM. Aortic valve ochronosis: a rare manifestation of alkaptonuria. BMJ Case Rep 2011;2011.
- Fisher AA, Davis MW. Alkaptonuric ochronosis with aortic valve and joint replacements and femoral fracture: a case report and literature review. Clin Med Res 2004;2:209-15.
- Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21.
- Ffolkes LV, Brull D, Krywawych S, Hayward M, Hughes SE. Aortic stenosis in cardiovascular ochronosis. J Clin Pathol 2007;60:92-3.
- Khaled A, Kerkeni N, Hawilo A, Fazaa B, Kamoun MR. Endogenous ochronosis: case report and a systematic review of the literature. Int J Dermatol 2011;50:262-7.