ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
A Guide to Robotic Assisted Single Vessel Coronary Artery Bypass Graft Surgery
Rehman A. A Guide to Robotic Assisted Single Vessel Coronary Artery Bypass Graft Surgery. November 2022. doi:10.25373/ctsnet.21469671.v1
In the era of advancing structural heart procedures and increasing percutaneous interventions, minimally invasive coronary artery bypass graft (CABG) surgery is a must-learn for current and aspiring surgeons. It can be approached with left internal mammary artery (LIMA) takedown through a left anterior minithoracotomy using special retractors or with robotic assistance. The procedure may be used for a single or multivessel CABG.
This article will only concentrate on robotic assisted takedown of LIMA with distal LIMA to left anterior descending artery (LAD) anastomosis through a 4 to 5 centimeter left anterior minithoracotomy. The steps outlined are for the purpose of starting a robotic assisted coronary artery bypass (R-CAB) program, or for current surgeons looking for a different perspective.
Patient Selection
This procedure can be applied in complex lesions, ostial stenosis, chronic total occlusion (CTO) of LAD, or in cases with comorbidities precluding a sternotomy, such as radiation therapy for single vessel disease CABG. In cases of multiple vessel disease, R-CAB may be utilized in a staged or simultaneous hybrid approach whereby R-CAB is used for LIMA to LAD, and non-LAD vessels are revascularized through percutaneous coronary intervention. Ideal patients will have a BMI less than 35, FEV1 more than 80 percent predicted value, EF greater than 50 percent, and CTO of LAD.
Anesthesia
General anesthesia with a double lumen endotracheal tube (ETT) is recommended for this procedure. Although single lumen ETT with an ipsilateral bronchial blocker works in normal lungs, double lumen ETT has an added advantage of positive-end expiratory pressure (PEEP) on contralateral lung in marginal pulmonary mechanics. Double lumen ETT is either removed at end of case for extubation or changed to a single lumen tube over a tube changer at end of case.
Vascular Access
A central venous access alone is sufficient in most cases. In patients with lower ejection fraction or pulmonary hypertension, a Swan Ganz catheter is beneficial. In addition, a radial or brachial arterial line is needed.
Patients should also have a 4 Fr sheath inserted in each common femoral artery and vein under US ultrasound guidance. This serves as access for any emergent or urgent need for peripheral cardiopulmonary bypass. The majority of patients either do not need it or have planned peripheral femoral arterial (Edwards OptiSite 16Fr or 18Fr) and venous (Liva Nova 22Fr or 25Fr) cannulation with US guided access and placement under fluoroscopic guidance. In this scenario, the femoral artery is perclosed with Perclose devices.
Positioning
The left side of the patient is raised at a 30 degree angle with a bean bag. Then, the patient is positioned to the left of table so that the left arm is supported and able to drop next to the table. These techniques help to drop the left shoulder so that it does not interfere with robotic arms. Next, the robot is positioned on the right side of patient. The sterile trays and scrub are on left side of patient, and the cardiopulmonary bypass machine is on right side of patient, toward the foot. In case of planned need for cardiopulmonary bypass, the machine will stay near the right lower extremity, and the robot can be docked at chest level. In case of urgent/emergent need (which is not common), the robot can undocked, cannulation will be facilitated by previously placed 4 Fr sheaths, cardiopulmonary bypass instituted, and robot redocked as the case proceeds as planned.
Robotic Trocar Positioning and Arm Docking
The middle, or camera port, trocar is first one to be inserted. This is followed by a trocar in the left subclavicular area, just anterior to the anterior axillary line. Again, its positioning is critical to prevent robotic arm conflict with left shoulder, which eventually affects its reach in takedown of distal LIMA. It is preferred to use a long trocar to prevent extrusion during the procedure. Lastly, the left lower trocar is inserted in left seventh interspace, in midclavicular line. Both trocars are inserted with direct robotic camera viewing.
The robot is then docked with camera arm only. The camera inserted and focused at the operative site for targeting of other arms (this step only applies to Da Vinci Xi). The other two arms are then docked.
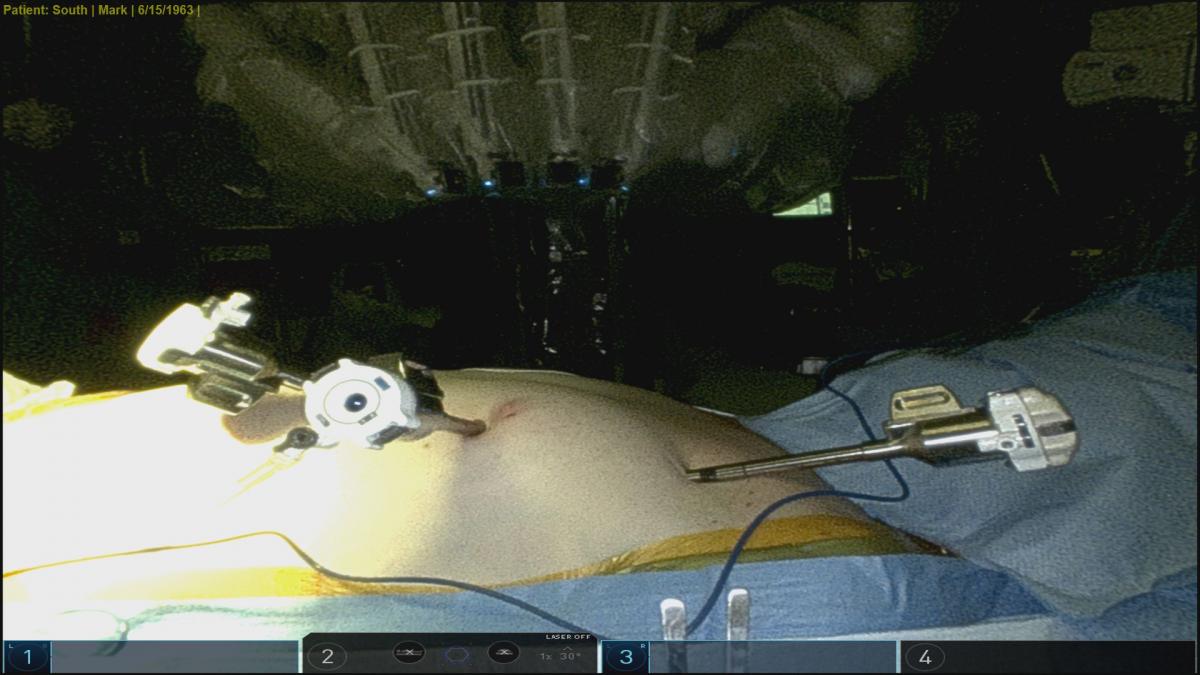
Port position

Robot docked
LIMA Takedown
As a first step, it is good practice to check the robot arms’ range of motion and review any conflicts. It is recommended to use a Bovie spatula in the right hand and Micro Diamond fine forceps in the left hand. Clips and scissors are used as needed. Later, the surgeons will switch to DeBakey forceps for taking down pericardial fat and opening up the pericardium. LIMA takedown is performed with robotic scope in 30 degrees up.
The whole length of visible LIMA and areas that are intramuscular are then looked at, and the takedown follows the same steps as for an open case. The whole length is not skeletonized, except the distal end, to facilitate flow measurements at the end. The rest of LIMA has a vein on each side, but fascia is completely off.
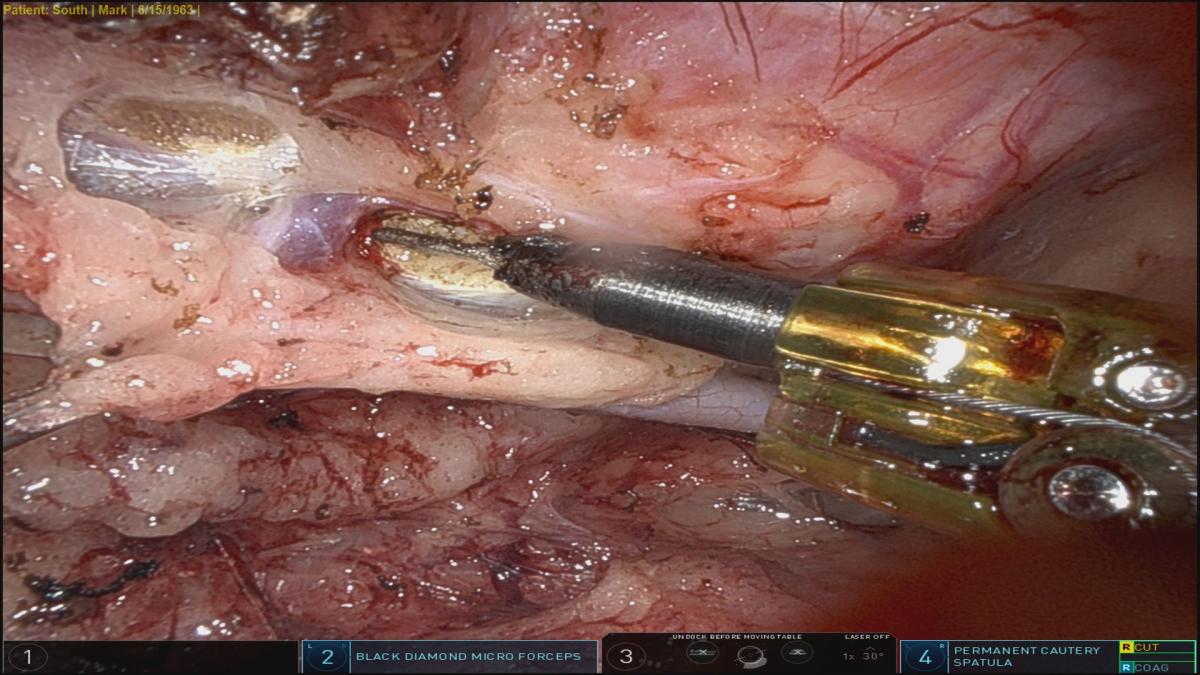
The whole length is visualized, and fascia taken down. Next, the spatula is used to perform sharp dissection, along with blunt dissection on inferior aspect of inferior vein. The superior vein is pulled down and dissection carried superior to it, exposing arterial and venous branches. Generally, a few branches are exposed, their LIMA end clipped, and anterior chest wall end of vessels electrocauterized. This process begins in the middle and moves proximally, beyond first cartilage, and just above the phrenic nerve, so that LIMA can drop down well with no proximal kink. It also ensures adequate length each time. Once proximal LIMA is dissected circumferentially, the mid- to distal end is approached. Once in the right plane, a lot may be dissected bluntly. The last 4 to 5 cm is completely skeletonized to facilitate clipping the distal end for flow measurements, until the vessel bifurcates or dives medially. Three clips are placed distally, one proximal, and then the distal LIMA is divided with scissors. The divided end is then clipped to anterior chest wall.
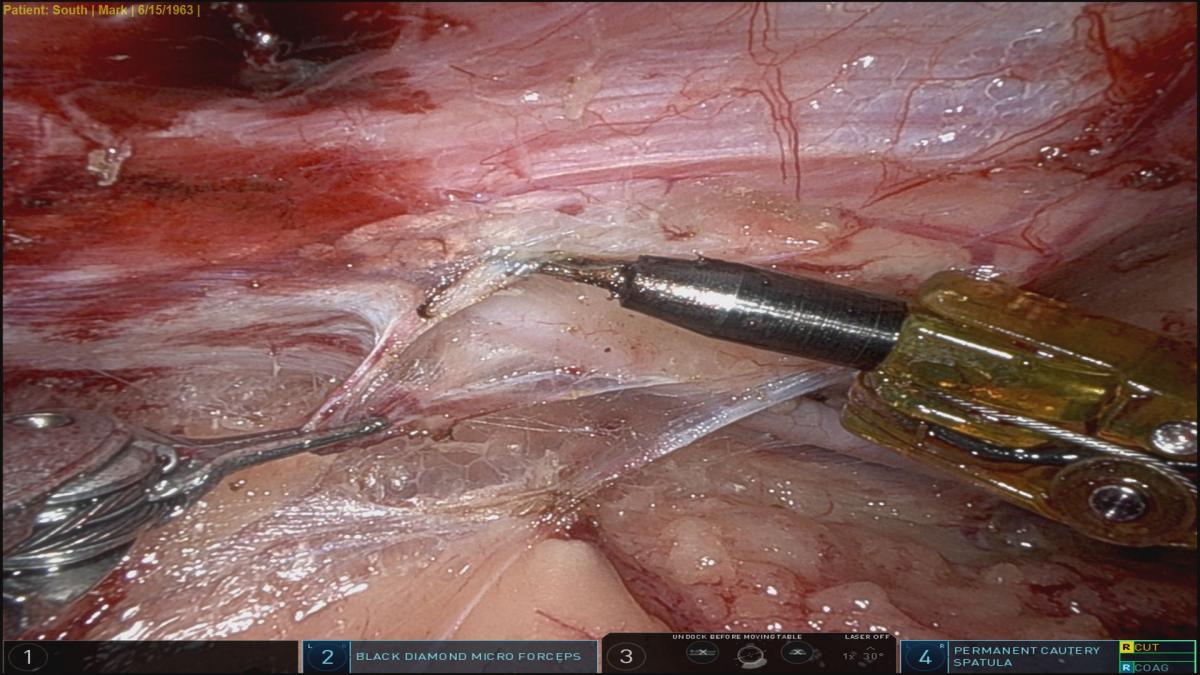
Dissecting fascia
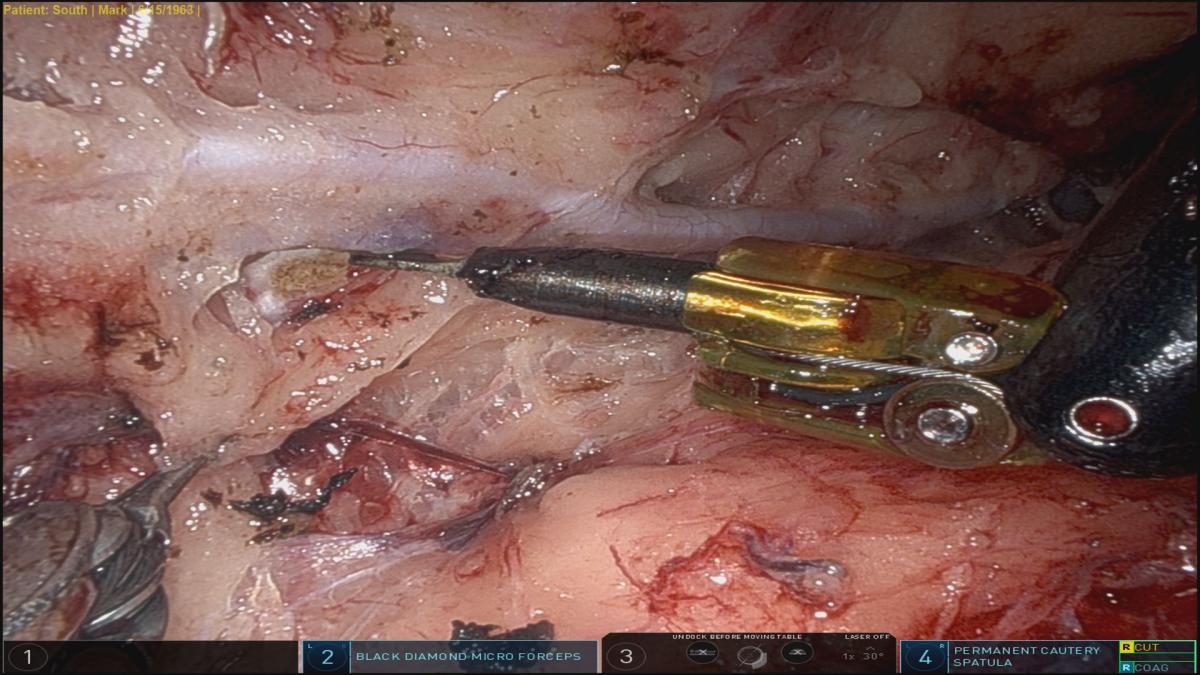
Dissecting inferiorly below mammary vein from end to end
Dissecting superiorly above mammary artery, end to end
Dissection of Subxiphoid Space
Next, the subxiphoid dissection with electrocautery is performed to facilitate the insertion of Medtronic Nuovo stabilizer rod.
Pericardial Fat and Pericardial Dissection
The Micro Diamond forceps are then switched to DeBakey forceps in the left hand, and pericardial resection is performed from medial to lateral to just above the phrenic nerve. Camera orientation is changed to 30 degrees down at this time, and a small lateral rent is made in the pericardium above the phrenic nerve. This facilitates insertion of a drop sucker during distal anastomosis and later for egress of blood or pericardial fluid into left pleural space postoperatively. Next, the anterior pericardium is opened from distal medial reflection to ascending aorta. On inferior aspect, the incision is not extended over the apex of heart, lest there be potential cardiac herniation. The ability to open the pericardium robotically is a critical advantage, since it gives the surgeon a bird’s-eye view of the anterior epicardial surface of the heart. Thus, one could ascertain, the course of LAD—whether it is on the surface, intramyocardial, only visible distally, or has large diagonal branches—is to plan a minithoracotomy incision, identify LAD correctly, perform distal anastomosis accordingly, and avoid any potential complications. Since the heart is being pushed medially, and because of CO2 insufflation, the exact location of structures may not be possible.
Insertion of Stabilizer Rod
Next, all instruments are removed and the camera is pointed toward the subxiphoid space. In thin patients, one can clearly see the site for external incision in the subxiphoid area externally, by illumination from the camera. The incision is generally a centimeter or two from the subxiphoid area and, initially, a Kelley forceps is inserted under robotic vision. This is followed by insertion of a stabilizer rod.
CO2 insufflation is then stopped, all ports are removed, and the right port site is closed in layers.
Minithoracotomy
A 4-5 cm minithoracotomy is made in left fourth intercostal space, generally by extension of camera port. However, if the patient is obese or has larger breast tissue, the camera port incision is closed and a separate 4-5 cm is made medially. The pericardial space exposed. A soft tissue retractor is inserted, followed by insertion of minimally invasive rib spreader. In the case of thinner patients and a shallow chest, one may not even need a rib spreader and exposure is good enough with a tissue spreader alone.
Preparation of LIMA
Next, LIMA is pulled into the incision. Orientation of LIMA is confirmed by looking at the entire length of the vessel. A 6-0 Prolene suture is inserted on each vein to keep the orientation of LIMA. Next, the distal end is prepared. LIMA is confirmed for good blood flow, and a proximal bulldog clamp is applied.
Distal Anastomosis
A suction tube is inserted through the left camera port site, and a foot plate is attached to a Nuovo stabilizer rod. LAD is then stabilized at the planned anastomotic site. If LAD is not CTO, a proximal encircling silastic tape is inserted. This facilitates an arteriotomy and insertion of a shunt. It also helps with flow measurement later, differentiating cases of competitive flow and retrograde flow in case of distal obstruction.
An arteriotomy is performed, followed by an appropriately sized shunt, and the proximal snare is released. Distal anastomosis is completed between the end of LIMA and side of LAD using running 7-0 Prolene. The bulldog clamp is removed and good hemostasis of anastomosis confirmed. The stabilizer and rod are then removed. Flow measurement is checked with and without proximal snare for excellent flow and low pulsatility index. The proximal snare is removed and a topical hemostatic agent applied to distal anastomosis.
Chest Tube Insertion and Lung Expansion
Next, a single right chest tube is inserted through the left port site and positioned in the left costophrenic space just above the diaphragm. The left pleural space is suctioned actively, and a 14 Fr endotracheal suction is inserted in the chest tube. The soft tissue retractor and rib spreader are removed. The superior end of the incision is lifted with a Richardson or Army/Navy retractor, the whole length of LIMA is visualized, and appropriate orientation is confirmed. Next, a Yankaeur suction tip (with no suction attached) is placed on top of LIMA. The left lung is inflated and its expansion above LIMA is visualized under direct vision.
Chest Closure and ETT
Finally, the chest wall incision is infiltrated with a long-acting local anesthetic and closed in layers. Generally, the patient is extubated in the OR. Otherwise, the double lumen tube is changed to a single lumen endotracheal tube over a tube changer.
Postoperative Course
The patient’s pain is controlled with a mixture of narcotics, Gabapentin, and in some cases, Ketorolac for twenty-four hours only. The patient is mobilized by end of day. If chest tube output is minimal, it is removed on postoperative day one, or later as necessary, and the patient is discharged home.
Final Tips
• In order to practice robotic LIMA takedown and eventual pericardial dissection, the surgeon could perform robotic LIMA takedown on planned sternotomy CABG patients. Port sites may be used for chest tube insertions.
• Practice off-pump distal anastomosis on standard sternotomy CABG patients as well.
• Ideally, antiplatelet agents and other anticoagulants must be stopped at least five days prior to surgery. However, in case of a hybrid approach, if PCI is performed first and LAD has to be intervened upon prior to stopping dual antiplatelet therapy (DAPT)—as newer coronary stents may have DAPT stopped in one month—switch to Clopidogrel and Aspirin to proceed with surgery, although patients have operated multiple times with Aspirin and Ticagrelor with no overt bleeding. One must be particular about LIMA bed and port sites in addition to pericardial dissection and distal anastomosis.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.





Comments