ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Highlighting Recent Research: Prognosis of Severe Asymptomatic Aortic Stenosis With and Without Surgery
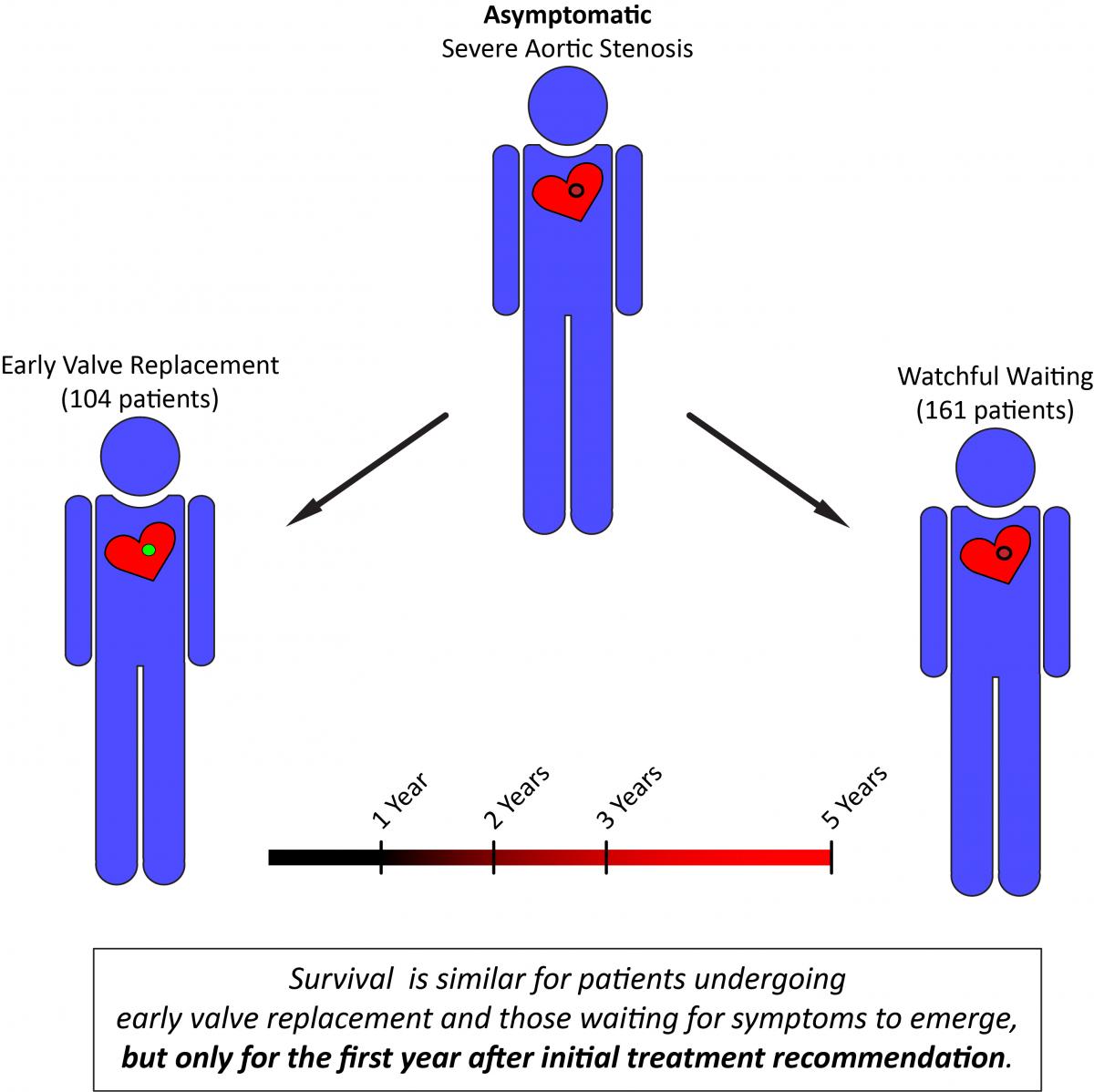
Campo and colleagues (2019) retrospectively analyzed the outcomes of 265 asymptomatic patients, with early AVR recommended for 104 patients and watchful waiting recommended for 161. Baseline characteristics differed between the two groups, with patients recommended for surgery being younger with smaller valve area, higher Vmax, and higher mean transvalvular pressure gradient. Unsurprisingly, the indications for surgery also differed between the groups, with concomitant cardiac disease and rapid progression of AS being the most common surgical indications for patients recommended early AVR (48% and 34%, respectively) and onset of symptoms being the most common indication for patients recommended watchful waiting (60%). Although all-cause mortality was similar in the first year after recommendation, survival curves for the two groups began to diverge after two years. Mortality in the early AVR group was 7.5% and 9.0% at 2 and 3 years, respectively. By contrast, mortality for patients in the watchful waiting group was 16.1% at 2 years and 21.1% at 3 years (p = 0.044 and p = 0.011 versus early AVR, respectively). Given the rate at which watchful waiting patients underwent AVR, only 56% of these patients were still alive and without valve replacement by two years after the initial treatment recommendation.
When evaluating outcomes for patients of both groups who underwent AVR, overall survival was similar at one, three, and five years after surgery. The authors suggest that the primary risk of watchful waiting is the possibility that subsequent intervention is not sufficiently timely after symptoms finally present. Additionally, the authors report that a relatively small proportion of patients underwent stress testing: 18% of the AVR group and 37% of the watchful waiting group. Dr Malaisrie emphasized that the study’s message for clinicians is that they should use stress testing in patients with severe AS. “The stress test supervised by a cardiologist poses no risk to the patient,” he says, “and is a key differentiator [between] patients who need early surgery versus patients who can be followed with watchful waiting.”
The authors acknowledge the retrospective nature of their study, noting the differences in baseline characteristics between the two groups and the challenges of accurately determining asymptomatic status from the patient’s electronic health record. With the goal of further addressing this topic, they are participating in the Early TAVR trial (ClinicalTrials.gov Identifier: NCT03042104), which has the goal of enrolling over 1000 patients with asymptomatic severe AS who will be randomized to either transcatheter AVR or watchful waiting. Additionally, the randomized AVATAR trial (ClinicalTrials.gov Identifier: NCT02436655) is also seeking to clarify the optimal treatment approach for asymptomatic AS.
References
Baumgartner H, Falk V, Bax JJ, et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2017;38(36):2739-2791.
Campo J, Tsoris A, Kruse J, et al. Prognosis of severe asymptomatic aortic stenosis with and without surgery [published online ahead of print March 21, 2019]. Ann Thorac Surg. doi:10.1016/j.athoracsur.2019.01.031.
Généreux P, Stone GW, O'Gara PT, et al. Natural history, diagnostic approaches, and therapeutic strategies for patients with asymptomatic severe aortic stenosis. J Am Coll Cardiol. 2016;67(19):2263-2288.
Lim WY, Ramasamy A, Lloyd G, Bhattacharyya S. Meta-analysis of the impact of intervention versus symptom-driven management in asymptomatic severe aortic stenosis. Heart. 2017;103(4):268-272.





