ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Moving the Needle: A Guide to Solving the Global Cardiac Surgery Puzzle for Surgeons, Societies, Students, and Researchers
Vervoort D. Moving the Needle: A Guide to Solving the Global Cardiac Surgery Puzzle for Surgeons, Societies, Students, and Researchers. February 2020. doi:10.25373/ctsnet.11872425
Traditionally, global health has concerned itself about infectious diseases and maternal and child health, disregarding access to surgical services when needed for the world’s population (1). In 2015, the Lancet Commission on Global Surgery and the World Health Organization’s World Health Assembly Resolution WHA68.15 positioned surgery as an indivisible, indispensable part of health care (1-3). However, until today, cardiac surgery has been largely neglected within global health and global surgery. Global cardiac surgery can be defined as “an area for study, research, practice, and advocacy that places priority on improving health outcomes and achieving health equity for all people worldwide who are affected by cardiac surgical conditions or have the need for cardiac surgical care,” first raised in 2018 (4). Disturbingly, although cardiovascular diseases constitute the world’s largest cause of mortality worldwide, over six billion people lack access to safe, timely, and affordable cardiac surgical and interventional services when needed (5). Traditionally, fly-in fly-out missions were considered the gold standard of providing cardiac surgical care for the world’s poorest populations, yet the lack of efficiency and sustainability thereof requires a change of mindset towards holistic health systems strengthening.
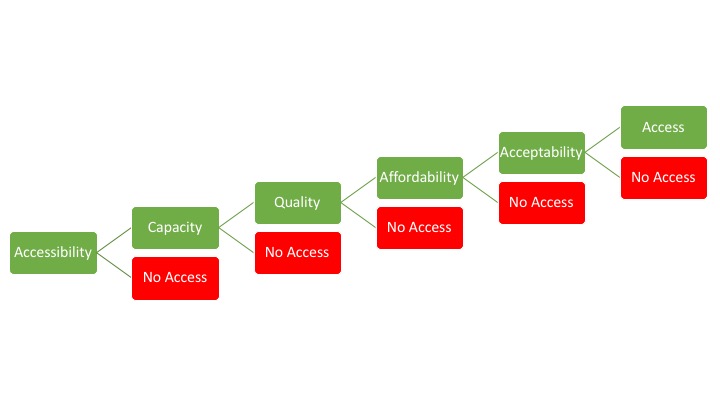
The reasons for the lack of access to cardiac surgical services are five-fold (Figure 1): geographical accessibility, material and human capacity, quality of care delivery, episodic affordability, and, importantly, social favorability. Around the world, countries have started developing health systems-based approaches to strengthen the surgical ecosystem within a country to facilitate the delivery of increasingly complex procedures at increasing volumes, under the umbrella of National Surgical, Obstetric, and Anesthesia Plans (6). Unfortunately, cardiac care has largely been neglected within this movement. Nevertheless, an adaptation of the framework allows for a dissection of the problem areas for the provision of high-quality, high-volume cardiac surgical services in low- and middle-income countries (LMICs), as summarized in Figure 2. Importantly, better understanding gaps in the workforce (including sex-based disparities within entire cardiac teams), cardiac centers, surgical volume, and operational cost and cost-effectiveness data will be instrumental to systemically change the paradigm.
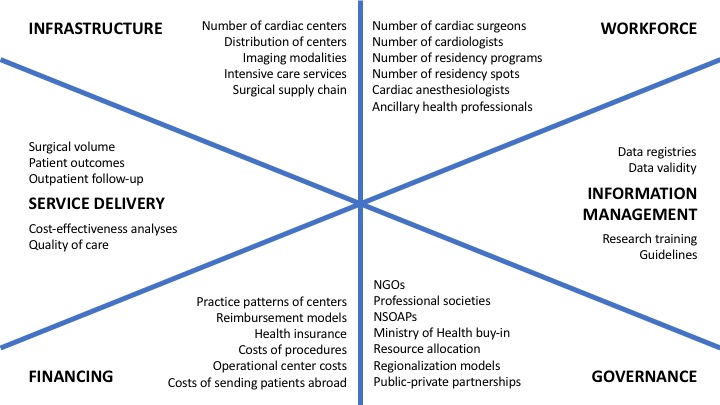
Figure 2. Knowledge gaps in the expansion and provision of cardiac surgical services in low- and middle-income countries using the six pillars of the National Surgical, Obstetric, and Anesthesia Planning framework. NGOs = Non-governmental organizations; NSOAPs = National Surgical, Obstetric, and Anesthesia Plans.
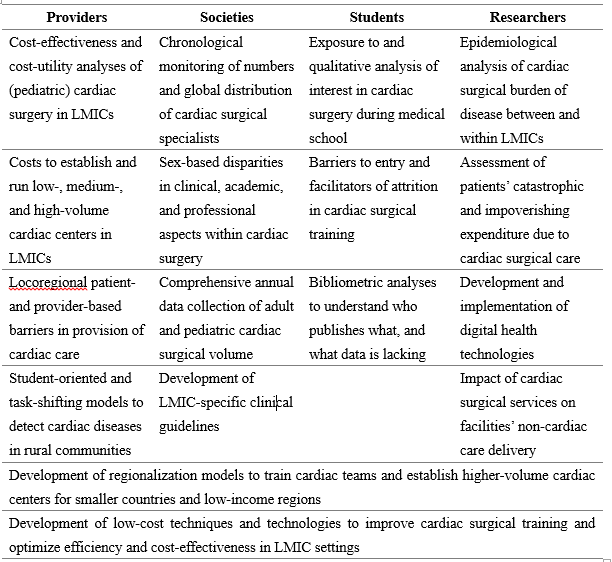
We cannot manage what we don’t measure, yet many countries lack the infrastructural and financial capacity to systematically collect data on an ongoing basis. For example, although still growing, South America has a relatively robust network of cardiac surgical care delivery supported by countries’ universal health coverage models, yet not one country has a national data registry for cardiac surgical care. Moreover, in LMICs around the world, data surrounding workforce, surgical volume, and expenses for surgical care are only limitedly collected. Health care professionals, professional societies, medical and public health students, and researchers can play an instrumental role in moving the needle towards greater equity to ensure that no cardiac patient is left behind (Table 1).
Table 1. Global cardiac surgery research action items for health care professionals, professional societies, medical and public health students, researchers, and other stakeholders. Note: this list is non-exhaustive. LMICs = low- and middle-income countries.
Surgeons and Other Health Care Professionals
As a result of a limited provision of cardiac surgical care in LMICs, few studies pertaining to global cardiac surgery have arisen in recent decades. In 2018, the first cost-effectiveness analysis of pediatric cardiac surgery in LMICs, albeit as a mission-based model, showed favorable cost-effectiveness of pediatric cardiac surgery ($171 per disability-adjust life year averted), even more so than common public health priorities such as oral rehydration therapy for diarrhea and anti-retroviral therapy for HIV/AIDS (7, 8). Despite many a provider’s altruistic sense to care for patients, money makes the political world go round and thus a better understanding of cost-effectiveness and operational costs of LMIC-based (ie, not mission-model) centers is required to leverage political buy-in and ensuing funding. Moreover, the diversity of LMICs, as a result of differences in human development index, political stability, and cultural nuances, leads to a diversity in barriers for patients to access care and providers to deliver care. In order to mitigate such barriers to access to care and improve care delivery, an evaluation thereof may present gaps otherwise unaddressed. Lastly, as half of the LMIC population lives in rural areas (ie, away from specialist cardiac care), the development of models to timely detect cardiac diseases in rural communities (eg, through targeted medical student or non-clinician health care professional training) will prove vital to prevent late-stage presentations (9).
Professional Societies
In 2018, the Society of Thoracic Surgeons (STS), American Association for Thoracic Surgery (AATS), the European Association for Cardio-Thoracic Surgery (EACTS), the Asian Society Cardiovascular and Thoracic Surgery (ASCVTS), the Pan-African Society of Cardiac and Thoracic Surgeons (PASCaTS), and the World Heart Federation collectively established the Cardiac Surgery Intersociety Alliance (CSIA) (10). The goal of the CSIA is to empower surgeons and cardiac centers in LMICs to scale their clinical and long-term academic capacity through financial support. Nevertheless, many opportunities arise:
- Workforce mapping: substantial disparities exist in the availability and distribution of cardiac surgical providers around the world. Low-income countries possess only 0.04 adult and 0.07 pediatric cardiac surgeons per million population, whereas high-income countries have 7.15 adult and 9.51 pediatric cardiac surgeons per million population (11). In other words, high-income countries have 179 times more adult cardiac surgeons and 134 times more pediatric cardiac surgeons than low-income countries. Improving the accuracy of these data and chronologically monitoring them is necessary to ensure that societies and countries can appropriately develop training programs and fill gaps in the availability of surgical providers.
- Gender equity: in high-income countries, comparably few female cardiothoracic surgeons are practicing, making cardiothoracic surgery one of the most disproportionate subspecialties in medicine. For example, in the United States, only 3% of accredited cardiothoracic surgeons are female (12). These disparities may be even larger in LMICs, as non-cardiac surgical subspecialties appear to indicate (13). Female surgeons face significantly more barriers than men regarding pay gaps, unconscious biases, academic performance and advancement, and family planning (14). Societies can and should take the lead in better understanding sex-based barriers in their countries and regions and should lead the way in moving towards gender equity.
- Training programs: the centralization and high costs of cardiac surgery training programs create significant barriers for the training of LMIC providers. Where high-income countries are already frugal in the training of cardiac surgeons due to the importance of hands-on training time and a relatively low need (compared to other specialties) of providers per million population, LMICs often lack existing training programs. For example, most aspiring cardiac surgeons in sub-Saharan Africa are required to leave their country, as training programs in the region only exist in Northern Africa, South Africa, Ghana, and Kenya – more often than not only having one or two spots available each year for foreign trainees. The move to North America, Europe, or Australasia is generally hard because of language barriers, visa regulations, or accreditation and examination requirements. The development of more regional training programs, as spearheaded by the College of Surgeons of Eastern, Central, and Southern Africa (COSECSA) and the West African College of Surgeons (WACS) for non-cardiac surgical subspecialties, will allow for a broader and standardized development of skilled cardiac surgeons in the region and mitigate potential brain drain (15).
Students, Researchers, and Other Stakeholders
In recent years, interest in the pursuit of a career in cardiac surgery has seen a reduction in high-income countries, in part due to the increase in minimally invasive cardiovascular procedures (commonly performed by interventional cardiologists) and resulting decline in cardiac surgical procedures (16, 17). Although delayed in time, the cardiac surgical community is now increasingly embracing a hybrid culture, whereby surgeons train in both open heart and endovascular procedures. However, limited early exposure to the field during medical school and negative perceptions of surgeons’ work-life balance deters students from entering the field (18). Medical students are uniquely positioned to examine existing barriers to enter the field among their peers, which would allow institutions and societies to better inform younger generations and to address entry barriers and attrition factors in cardiac surgical training.
In turn, it is estimated that 32% of cardiovascular diseases will require surgical care at least once across their lifetime, yet region- and disease-specific needs remain unknown (19). Researchers possess the technical knowledge to analyze the cardiac surgical burden of disease between and within LMICs, which helps to understand the global met and unmet need of cardiac care. Similarly, they are capable of assessing patients’ financial hardship as a result of receiving cardiac care. Around the world, 81 million people are pushed (further) into poverty every year due to requiring surgical care (20). Due to the high and often out-of-pocket costs for cardiac care, many patients requiring surgery are forced to sell assets, loan money, or even refrain from receiving lifesaving or life-changing care; however, the exact burden is unknown, yet knowledge thereof can better inform macro- and microeconomic arguments in favor of countries’ investments in cardiac care. Lastly, designing and evaluating the implementation of digital health technologies to improve access to cardiac care (eg, telecardiology) ensures a reduced need of patients’ costly transportation towards cardiac centers for follow-up and less use of already constrained resources (21).
Ultimately, interdisciplinary and intersectoral collaborations between all stakeholders will be needed to develop effective regionalization models for the training of LMIC cardiac teams and to develop low-cost technologies to improve training and care delivery in LMIC settings. In a field as complex and costly as cardiac surgery, the need to reduce costs and increase procedural volume (per provider and per center) to optimize patient outcomes is ever so high (22).
Moving the Needle
Gross inequities persist in the provision of cardiac care around the world. In a day and age where North American and European professionals continue the pursuit of the most innovative technologies to improve patient outcomes, LMICs struggle to provide conventional open heart surgery for those in need at the rates they need it. As professional societies, providers, researchers, and advocates, we have the moral imperative to get rid of cardiac surgery’s invisible stepchild of global health moniker (23). Six billion people worldwide lack access to safe, timely, and affordable cardiac surgical care when needed, and their fate should not be determined by the country or prosperity in which they were born.
References
- Farmer PE, Kim JY. Surgery and global health: A view from beyond the OR. World J Surg. 2008; 32: 533–536.
- Meara JG, Leather AJM, Hagander L, Allkire BC, Alonso N, Ameh EA, et al. Global surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015 Aug 8;386(9993):569-624.
- World Health Organization. WHA68.15: Strengthening emergency and essential surgical care and anaesthesia as a component of universal health coverage. 2015. apps.who.int/gb/ebwha/pdf_files/wha68/a68_r15-en.pdf.
- Vervoort D. Global cardiac surgery: a wake-up call. Eur J Cardio-Thoracic Surg. 2019; 55: 1022–1023.
- Reichert HA, Rath TE. Cardiac surgery in developing countries. J Extra Corpor Technol. 2017; 49: 98–106.
- Sonderman KA, Citron I, Mukhopadhyay S, Albutt K, Taylor K, Jumbam D, et al. Framework for developing a national surgical, obstetric and anaesthesia plan. BJS Open. 2019; 3: 722–732.
- Cardarelli M, Vaikunth S, Mills K. Cost-effectiveness of humanitarian pediatric cardiac surgery programs in low- and middle-income countries. JAMA Netw Open. 2018; 1: 1–12.
- Grimes CE, Henry JA, Maraka J, Mkandawire NC, Cotton M. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014; 38: 252–263.
- World Bank. Rural population (% of total population). World Bank Data. 2019. https://data.worldbank.org/indicator/SP.RUR.TOTL.ZS?locations=XO (accessed Jan 4, 2020).
- Boateng P, Bolman III RM, Zilla P. Cardiac surgery for the forgotten millions: the way forward. Cardiac Surgery Intersociety Alliance (CSIA) Site Selection Criteria. Eur J Cardio-Thoracic Surg. 2019; 56: 217.
- Vervoort D, Meuris B, Meyns B, Verbrugghe P. Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 2019 Apr 26. pii: S0022-5223(19)30935-3.
- Antonoff MB, Brown LM. Work-life balance: the female cardiothoracic surgeon’s perspective. J Thorac Cardiovasc Surg. 2015; 150: 1416–1421.
- O’Flynn E, Andrew J, Hutch A, Kelly C, Jani P, Kakande I, et al. The Specialist Surgeon Workforce in East, Central and Southern Africa: a situation analysis. World J Surg. 2016; 40: 2620–2627.
- de Costa J, Chen-Xu J, Bentounsi Z, Vervoort D. Women in surgery: challenges and opportunities. IJS Glob Heal. 2018; 1. https://journals.lww.com/ijsgh/Fulltext/2018/07000/Women_in_surgery__cha....
- Hutch A, Bekele A, O’Flynn E, Ndonga A, Tierney S, Fualal J, et al. The brain drain myth: retention of specialist surgical graduates in East, Central and Southern Africa, 1974-2013. World J Surg. 2017; 41: 3046–3053.
- Vanderby SA, Carter MW, Latham T, Ouzounain M, Hassan A, Tang GH, et al. Modeling the cardiac surgery workforce in Canada. Ann Thorac Surg. 2010; 90: 467–473.
- Preece R, Ben-David E, Rasul S, Yatham S. Are we losing future talent? A national survey of UK medical student interest and perceptions of cardiothoracic surgery. Interact Cardiovasc Thorac Surg. 2018; 27: 525–529.
- Coyan GN, Kilic A, Gleason TG, Schuchert MJ, Luketich JD, Okusanya O, et al. Medical student perceptions of a career in cardiothoracic surgery: Results of an institutional survey. J Thorac Cardiovasc Surg. 2019; : S0022-5223(19)31483-31487.
- Rose J, Chang DC, Weiser TG, Kassebaum NJ, Bickler SW. The role of surgery in global health: Analysis of United States inpatient procedure frequency by condition using the global burden of disease 2010 framework. PLoS One. 2014; 9. DOI:10.1371/journal.pone.0089693.
- Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Heal. 2015; 3 Suppl 2: S38-S44.
- Vervoort D, Kpodonu J. Using technology and innovation to address the three delays in access to cardiac surgery. African Ann Thorac Cardiovasc Surg. 2018; 13(1): 5–10.
- Kalfa D, Chai P, Bacha E. Surgical volume-to-outcome relationship and monitoring of technical performance in pediatric cardiac surgery. Pediatr Cardiol. 2014; 35: 899–905.
- Zheleva B, Atwood JB. The invisible child: childhood heart disease in global health. Lancet. 2017; 389: 16–18.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.