ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Robotic-Assisted Left Upper Lobectomy in Non-Small Cell Lung Cancer With N1 Disease
Herrera LJ. Robotic-Assisted Left Upper Lobectomy in Non-Small Cell Lung Cancer With N1 Disease. April 2018. doi:10.25373/ctsnet.6123011.
This video demonstrates a procedure performed for a 56-year-old woman with a cT1BN1M0 stage IIB adenocarcinoma of the left upper lobe. She underwent endobronchial ultrasound for mediastinal staging, which ruled out N2/N3 disease and confirmed the diagnosis by guided sampling of a level 10L node in the left hilum. A robotic-assisted approach can be helpful to complete the lymph node dissection during lobectomy and compares favorably to video-assisted thoracoscopic approaches (1). Here, the author demonstrates a left upper lobectomy using the da Vinci Xi Surgical System™ with robotic stapling.
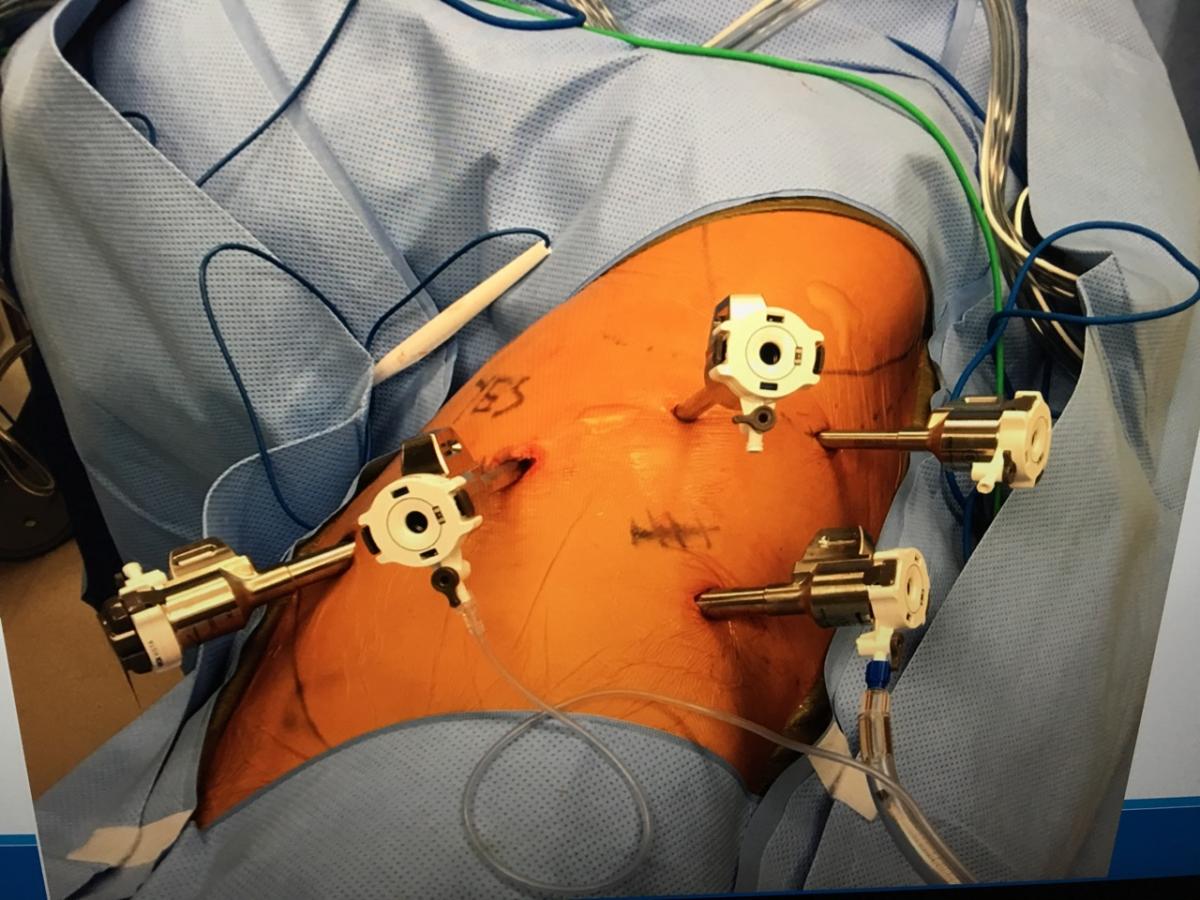
The case is performed with standard thoracoscopic setup, double lumen intubation, and lateral position flexed at the hip. Trocar placement consists of one 12 mm robotic trocar in the seventh intercostal space (ICS) anterior axillary line, next to the costal margin. This is followed by three 8 mm robotic trocars placed in the same seventh ICS, spacing them 8 cm apart. A second 12 mm robotic trocar for the assistant and for posterior placement is then placed in the ninth ICS posterior axillary line, directly inferior to the trocar in arm three, in order to share the robotic arm during stapling maneuvers (Figure 1). The instruments consist of a tip-up grasper in arm four, a curved bipolar dissector in arm three, the 8 mm Xi camera in arm two, and a Cadiere forceps in arm one.
The procedure starts with the lymph node dissection. The author begins by dividing the inferior pulmonary ligament, reflecting the lung anteriorly, and dissecting the posterior hilum and the posterior level 10L and 11L nodes. The focus is then on resecting the known N1 disease on the more proximal 10L nodes along the left main bronchus. The fissure is divided if well-developed, and the artery is visible. The author then divides the posterior segment pulmonary artery branch, and dissects the hilar nodes further to expose the apical and lingular arteries. The lingular artery is then divided with a vascular staple load, which then facilitates dividing the anterior aspect of the fissure. At this point, the lung is reflected posteriorly in order to isolate and divide the superior pulmonary vein, using the assistant 12 mm trocar to obtain a posterior stapling access. Lastly, the first branch of the pulmonary artery is divided to isolate and divide the left upper lobe bronchus with a green load robotic stapler. The author completes the node dissection, resecting the level 5 aortopulmonary window nodes.
One chest tube and one small pigtail catheter were placed, and the main chest tube was removed on postoperative day one. The accessory drain, which was left clamped, was removed on postoperative day two, and the patient was discharged home. Final pathology showed a pT1cN1M0 stage IIB non-small cell lung cancer, with 4 of 14 nodes positive in the 10L and 11L station.
Reference
- Velez-Cubian FO, Rodriguez KL, Thau MR, et al. Efficacy of lymph node dissection during robotic-assisted lobectomy for non-small cell lung cancer: retrospective review of 159 consecutive cases. J Thorac Dis. 2016;8(9):2454-2463.
Dr Herrera is a speaker and instructor for Intuitive Surgical, Inc.