ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Aortic Root Remodelling, Debranching of Arch, Ascending Aorta Replacement (Lupiae) and CABGX3 Prior TEVAR for Type B Aortic Dissection
Raheel FA, Ahmed A, Mariscalco G. Aortic Root Remodelling, Debranching of Arch, Ascending Aorta Replacement (Lupiae) and CABGX3 Prior TEVAR for Type B Aortic Dissection. August 2020. doi:10.25373/ctsnet.12762068
The first aortic arch surgery was performed in 1957 as a resection of fusiform aneurysm of aortic arch with replacement by homograft (1). However, during the last 63 years, there were significant developments in terms of operative techniques, prosthesis materials, and imaging techniques with digital technology. Subsequently, the endovascular stent-grafts across the primary entry tear, for the management of acute aortic dissection originating in the descending thoracic aorta, was introduced in 1999 (2, 3).
Aortic cardiac surgeons encounter various aortic pathologies with aortic dissections. There are many combinations, and surgeon management of these conditions depends on the clinical scenario. Stanford type A aortic dissection is typically treated surgically, while Stanford type B is primarily treated conservatively, and complicated type B dissection is frequently treated with emergency EVAR stent (4). Furthermore, chronic type B aortic dissection with aneurysmal degeneration was treated safely with TEVAR (5). DeBakey type I aortic dissection is a catastrophic event that can be managed with combined surgical and endovascular treatment with arch preservation (6), though TEVAR in type B dissection may lead to retrograde type A dissection (7).
Hybrid aortic arch debranching procedures are a safe alternative to open repair (8, 9). In the treatment of acute Stanford type A aortic dissection, patients older than 60 years undergoing hybrid debranching surgery had shorter hospital lengths of stay, lower rates of neurologic events and renal insufficiency, and a higher mid-term survival rate compared with the total arch replacement procedure (10). Therefore, no single technique is ideal as no two aortas and their pathology are the same.
Concomitant aortic root aneurysm is usually treated with either modified Bentall technique of root replacement or valve-conserving techniques, Yacoub (11) or Tirone David (12). Leon introduced a simple technique of aortic root remodeling without the handling of coronary ostia that involved the excision of most of the aortic root wall except around the coronary ostia (13). The elderly patients with concomitant coronary artery disease, technical challenges like previous aortic stent in distal arch in Ishimaru's zone 2, as in this case; fragile tissues as well as lack of experience preclude cardiac surgeons to do ascending aorta and aortic root operation after type B aortic dissection repaired with the stent. The authors demonstrate, in this video, a technique to manage complex aortic pathology with coronary artery disease.
Patient Selection
The authors have been using the Lupiae technique for several years in aortic arch pathology. Patients were identified during preoperative work-up for aortic valve surgery or as incidental diagnosis or presented with the A or type B aortic dissection, as in this case. They selected those patients whose aortic arch was aneurysmal with or without ascending aorta/root aneurysm and came under the European Society of Cardiology guidelines. All patients had preoperative CT scan, echocardiogram, and immediate pre- and postoperative TOE that confirmed the diagnosis and repair.
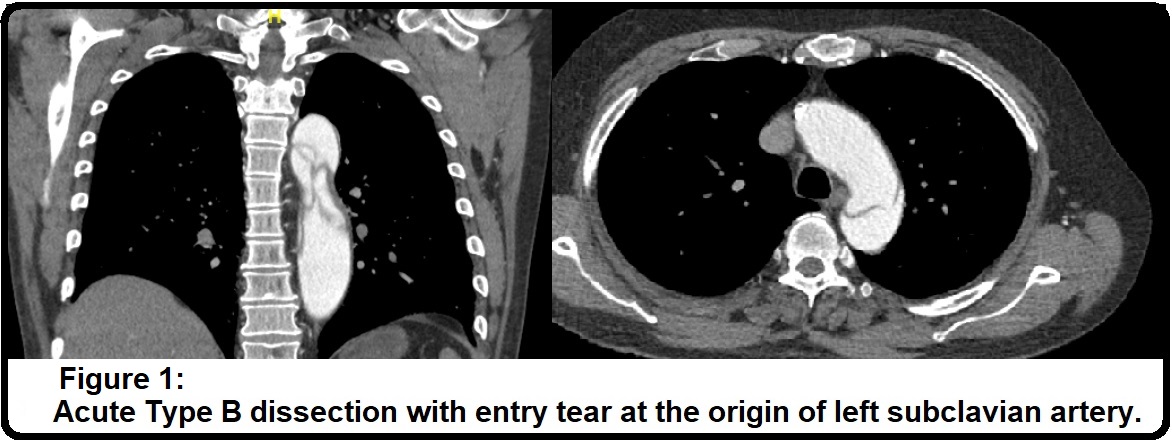

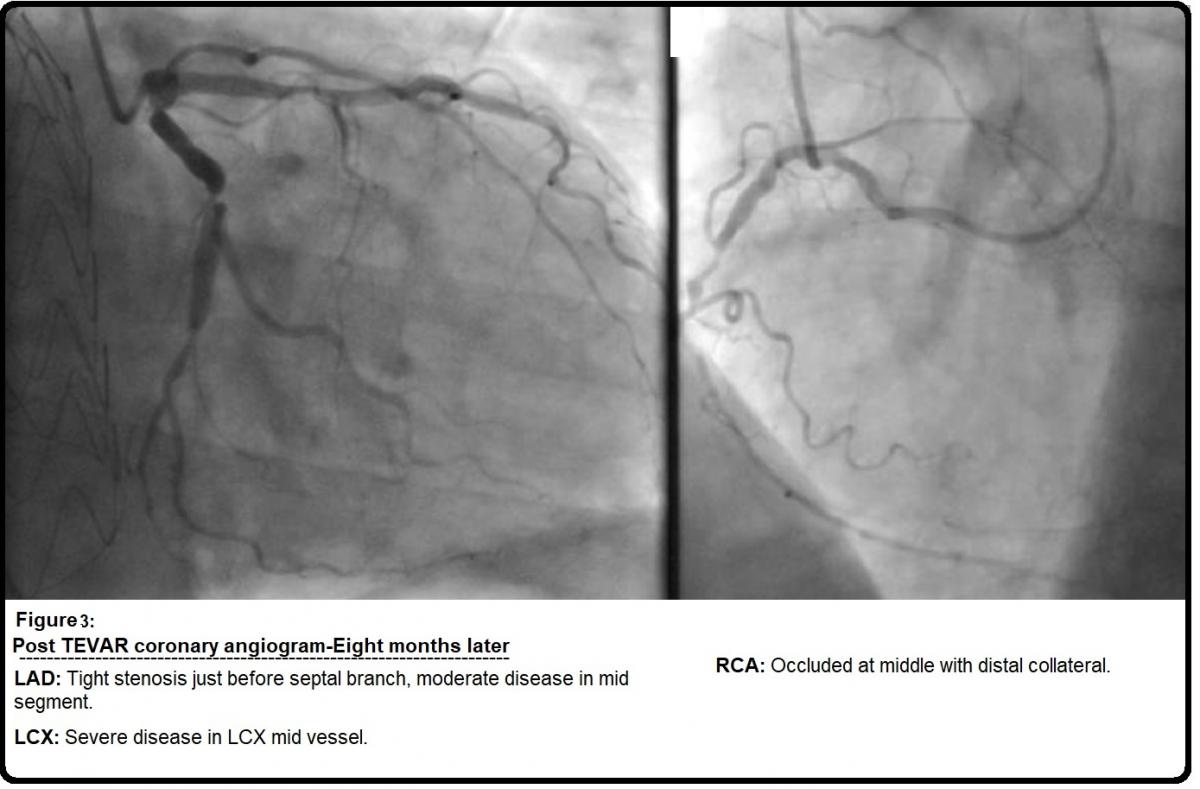
The patient in this video was a 69-year-old man who presented to the emergency department with sudden onset of chest and back pain. He was a smoker, otherwise there was no significant comorbidity, however, on admission he was markedly hypertensive. CT aorta revealed an acute type B dissection with an entry tear at the origin of the left subclavian artery; left kidney was malperfused and true lumen was significantly compressed by the false lumen (Figure 1). He developed acidosis that was a sign of organs ischaemia. He underwent emergency procedures that included left carotid-subclavian arteries bypass graft with 6 mm Dacron graft and percutaneous thoracic endovascular arterial repair in Ishimaru's zone 2, 3, 4 (TEVAR-Stent; Conformable GORE® Thoracic Endoprosthesis) (Figure 2). He was discharged on the sixth postoperative day in good condition. Subsequent CT scan showed the diameter of the ascending aorta 53 mm, while coronary angiogram revealed LAD stenosis (tight stenosis just before septal branch, moderate disease in mid segment), LCX stenosis (severe disease in LCX mid vessel), and RCA stenosis (Occluded at middle with distal collateral) (Figure 3). Transthoracic echocardiogram showed trivial aortic regurgitation, 39 mm sinus diameter and normal LV & RV systolic function.
Taking consideration of his recent type B dissection, aortic dimensions, and three vessels coronary disease, he was offered surgery that he accepted. Lupiae technique for aortic arch debranching was chosen as percutaneous thoracic endovascular arterial repair involved Ishimaru's zone 2. Eight months later of TEVAR-Stent, he underwent resuspension of aortic valve with remodelling of the aortic root, debranching of aortic arch, replacement of proximal ascending aorta (Lupiae technique), and concomitant triple coronary artery bypass graft (SVG-LAD, SVG-OM1, and SVG-RCA). Operative findings: The ascending aorta was frankly dilated up to the origin of the innominate artery; the arch portion close to the innominate artery was calcified, while the aortic root mainly effaced at the noncoronary sinus. Cumulative bypass time was 230 minutes; cumulative cross clamp time was 146 minutes. He was admitted one day before the operation and was discharged on the seventh postoperative day with very good recovery.
Operative Steps: Total 40 clips composed in this videos
- Median sternotomy and pericardiotomy as routine. Extend skin incision as T shaped at the upper part of the midline skin incision. This will allow accessing the brachiocephalic artery and left common carotid artery. Dissect ascending aorta, as much as can easily be done, especially distally and in the aortopulmonary window. Pass the Nylon tapes around the brachiocephalic vein and artery.
- Expose the right axillary artery with the oblique incision starting below the lateral and mid third of the clavicle, expose the axillary artery, pass two nylon tapes around the axillary artery, and make an end to side anastomosis with 8 mm Dacron tube graft with the 5 zero proline suture. Give heparin as usual.
- Join the arterial tube of cardiopulmonary circuit with three PVC tubes that require three Y connectors. Join one limb of the arterial tube with the Dacron tube graft that was anastomosis with the right axillary artery.
- Pass two stage venous cannula through the right atrium. Then, place the purse-string in the right atrium and pass the retrograde cardioplegia cannula. Now establish cardiopulmonary bypass as routine for aortic valve surgery.
- Pass Nylon tape around the ascending aorta and mark the site of distal aortic anastomosis. Pass LV vent through the purse-string suture in the right upper pulmonary vein.
- Pass the aortic root vent cannula in the ascending aorta. Apply aortic cross clamp; infuse antegrade cardioplegia. Then perform three distal coronaries anastomosis as routine.
- Excise the aorta; 2 cm distal to the coronary ostia and 1 cm proximal to the aortic cross clamp.
- Resuspension of aortic valve and aortic root remodelling.
- Pass a 4-0 proline pledged suture through the adjacent aorta, keep pledged just above the commissure between left and non-coronary cusp.
- Similarly, pass a 4-0 proline pledged suture through the aorta, keep pledged just above the commissure between left and right cusp.
- Similarly, pass a 4-0 proline pledged suture through the aorta, keep pledged just above the commissure between right and non-coronary cusp.
- Take two teflon strips. Place one strip at the outer surface of the aorta edge, circumferentially.
- Secure this strip with those three proline sutures that were passed through the aorta above the commissure. Tie these sutures but do not cut as they will work as stay sutures. Further trim the noncoronary sinus; just left the aorta equal the width of the Teflon strip.
- Cut two small pieces from the other Teflon strip and place them inside the noncoronary side of the aorta. Fix them with the 4-0 proline suture, as shown in the video. Select the appropriate diameter of Lupiae prosthesis, in this case size 30 mm diameter was selected. Trim the Lupiae prosthesis up to 2 cm from the first side branch of the graft. Then suture Lupiae prosthesis to the aortic root with a running suture of propylene 4/0; start from the posterior wall and finish anteriorly.
- Trim the distal Lupiae prosthesis; infuse antegrade cardioplegia through the graft and at the same time check the hemostasis.
- Reinforce the any leakage with proline 4/0 pledged sutures.
- Reinforce the distal aorta with the two Teflon strips, one internal and the other external. Trim the distal Lupiae prosthesis to the appropriate length, as seen in the video.
- Then suture Lupiae prosthesis to the distal aorta with a running suture of propylene 4/0; start from the posterior wall and finish anteriorly.
- Attach the cardioplegia line with the lateral 10 mm side branch of the Lupiae prosthesis; infuse antegrade cardioplegia through the graft and at the same time check the haemostasis.
- In full cross clamp, the vein graft for the first obtuse marginal and right coronary artery are anastomosed to proximal portion of the Lupiae prosthesis. While the vein graft for the left anterior descending artery is anastomosed to the proximal part of the vein, graft for the first obtuse marginal as "Y" graft.
- De-air the heart and the aorta. Remove aortic cross clamp and the retrograde cardioplegia cannula and tie the purse-string suture. Attach atrial and ventricular epicardial pacing wires.
Debranch the aortic arch and anastomosis with the Lupiae prosthesis. - Join the second limb of the arterial line with the lateral 10 mm side branch of the Lupiae prosthesis for arterial blood return from the cardiopulmonary bypass pump. Clamp and divide the left common carotid artery. Pass 8 mm lateral branch of the Lupiae prosthesis underneath the brachiocephalic vein and divide to an appropriate length. Anastomose the left common carotid artery with the 8 mm lateral branch of the Lupiae prosthesis by using 5 zero proline suture, as seen in the video. Check carefully the suture line.
- Dissect, mobilize, and pass a tape around the brachiocephalic artery; then clamp and divide the artery. Antegrade cerebral perfusion flow maintained through the axillary artery cannulation. Pass 10 mm lateral branch of the Lupiae prosthesis underneath the brachiocephalic vein and divide to an appropriate length. Anastomose the brachiocephalic artery with the 10 mm lateral branch of the Lupiae prosthesis by using 5 zero proline suture, as seen in the video. Prior to tie the suture, release the proximal clamp from the 10 mm lateral branch of the Lupiae prosthesis, de-air the artery, then tie the suture. Then release the distal clamp from the brachiocephalic artery.
- Adjust the lie of the lateral branches of the Lupiae prosthesis that were anastomosed with the brachiocephalic artery and the left common carotid artery.
- Check the hemostasis; de-air the aorta with couple of 25-gauge needles.
- Wean off the cardiopulmonary bypass as routine; remove the venous pipe and tie the side branch of the Lupiae prosthesis.
- See the final image of debranching of the aortic arch, resuspension of the aortic valve, aortic root remodelling, replacement of the proximal ascending aorta, and coronary artery bypass graft X 3 post type B aortic dissection treated with TEVAR.
Tips and Pitfalls
- Convert midline incision to T-shaped incision after the sternotomy, at the level of the left brachiocephalic vein. This will allow for good exposure of the aortic arch branches.
- Pass nylon tape around the left brachiocephalic vein and dissect to free this vein from the surrounding soft tissues. This will further expose the aortic arch and branches.
- De-airing: Connect the vent suction tube with one of the side branches of the Lupiae prosthesis that can work as root vent. Fill the heart, then use a size 25-gauge needle to puncture the Dacron tube graft. Once air bubble is stopped, remove the aortic cross clamp.
- Continuously monitor the cerebral oximeter to keep the saturation of both sides, right and left, around 50%.
- Check and recheck the aortic suture lines; use extra interrupted sutures with/without piece of Teflon, if any leakage more than needle holes.
Acknowledgement
Thank you to Maaz A Khan, Saad A Khan, and Zabreen Ahmed for video narration.
References
- De Bakey ME, Crawford ES, Cooley DA, Morris Jr. GC. Successful resection of fusiform aneurysm of aortic arch with replacement by homograft. Surg Gynecol Obstet. 1957 Dec;105(6):657-664.
- Dake MD, Kato N, Mitchell RS, Semba CP, Razavi MK, Shimono T, et al. Endovascular stent-graft placement for the treatment of acute aortic dissection. N Engl J Med. 1999 May 20;340(20):1546-1552.
- Nienaber CA, Fattori R, Lund G, Dieckmann C, Wolf W, von Kodolitsch Y, et al. Nonsurgical reconstruction of thoracic aortic dissection by stent–graft placement. N Engl J Med. 1999;340:1539–1545.
- Ternes Rech JV, Martins Pereira de Moura Ternes C, Busch Justino G, Narciso Franklin R, Do Nascimento Galego G. Endovascular approach to severe acute type B aortic dissection. Cureus. 2019 Dec 31;11(12):e6528.
- Scali ST, Feezor RJ, Chang CK, Stone DH, Hess PJ, Martin TD, et al. Efficacy of thoracic endovascular stent repair for chronic type B aortic dissection with aneurysmal degeneration. J Vasc Surg. 2013 Jul;58(1):10-7.e1.doi:10.1016/j.jvs.2012.12.071. Epub 2013 Apr 3.
- Hsu CP, Huang CY, Chen HT. Combined surgical and endovascular treatment with arch preservation of acute DeBakey type I aortic dissection. J Chin Med Assoc. 2019 Mar;82(3):209-214.
- Misfeld M, Nötzold A, Geist V, Richardt G, Sievers HH. [Retrograde type A dissection after endovascular stent grafting of type B dissection]. Z Kardiol. 2002 Mar;91(3):274-277.
- Papakonstantinou NA, Antonopoulos CN, Baikoussis NG, Kakisis I, Geroulakos G. Aortic arch reconstruction: are hybrid debranching procedures a good choice? Heart Lung Circ. 2018 Nov;27(11):1335-1349.
- Shirakawa Y, Kuratani T, Shimamura K, Torikai K, Sakamoto T, Shijo T, et al. The efficacy and short-term results of hybrid thoracic endovascular repair into the ascending aorta for aortic arch pathologies. Eur J Cardiothorac Surg. 2014 Feb;45(2):298-304.
- Shi F, Wang Z. Acute aortic dissection surgery: hybrid debranching versus total arch replacement. J Cardiothorac Vasc Anesth. 2019 Dec 11.
- Yacoub M. Valve-conserving operation for aortic root aneurysm or dissection. Oper Tech Card Thorac Surg. 1996;1(1):57-67.
- David TE. Remodeling the aortic root and preservation of the native aortic valve. Oper Tech Card Thorac Surg. 1996;1(1):44-56.
- Raheel FA, Ahmed A, Hadjinikolaou L. Replacement of the ascending aorta with aortic root remodeling without coronaries ranastomosis. CTSNet. May 2019. doi:10.25373/ctsnet.8069369.
Disclosure
Furqan Raheel, Aamer Ahmed, and Giovanni Mariscalco currently work at Glenfield Hospital, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom.
Disclaimer
The information and views presented on CTSNet.org represent the views of the authors and contributors of the material and not of CTSNet. Please review our full disclaimer page here.





Comments