ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Highlighting Recent Research: Impact of Minimally Invasive Extracorporeal Circuits on Octogenarians Undergoing CABG
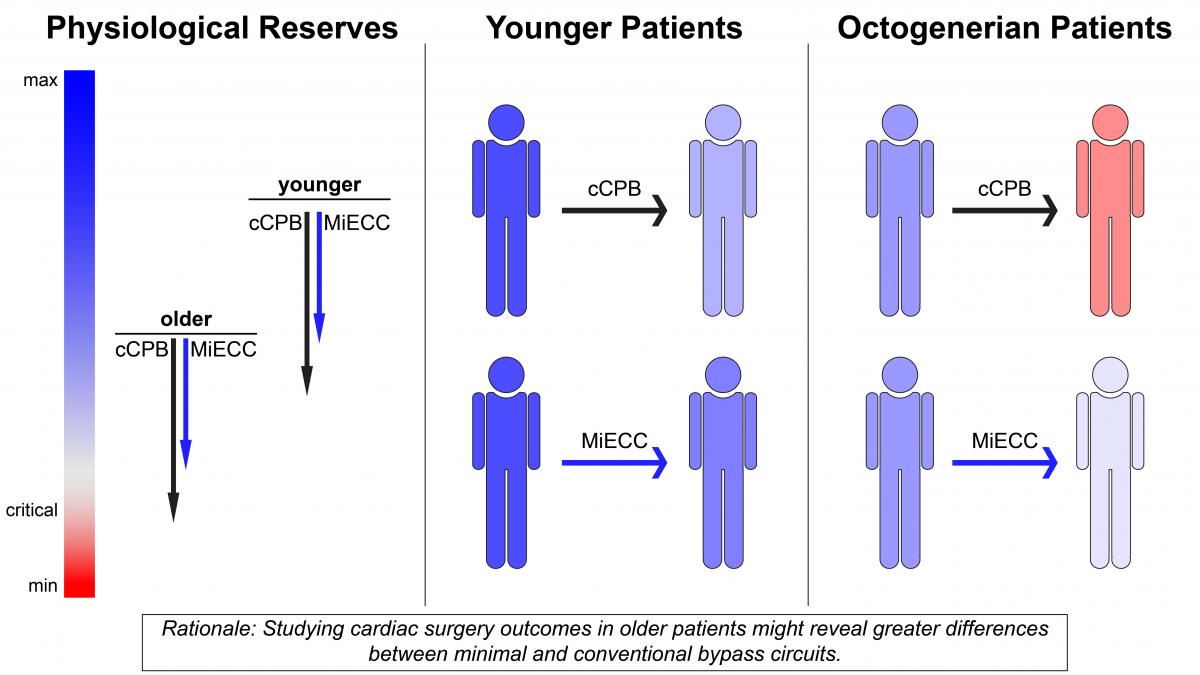
The authors retrospectively analyzed records for 324 octogenarians who had undergone coronary artery bypass surgery (CABG) at their institution over eight years (El-Essawi, 2017). The two groups had similar EuroSCOREs, 16 ± 13 and 14 ± 11 for MiECC and cCPB, respectively. The group that underwent CABG on MiECC had a greater proportion of patients with reduced left ventricular ejection fraction, a higher incidence of renal dysfunction, a lower incidence of unstable angina, and was older than the group who underwent surgery with cCPB. After propensity matching to account for these differences, 30-day mortality in patients who had MiECC was 2.4%, significantly lower than 9.5% for matched patients who had cCPB (p = 0.02). More surprising to the authors, however, was that this survival benefit was apparent prior to propensity matching: 3.5% with MiECC versus 9.0% with cCPB (p = 0.04). “We interpreted this finding as follows,” said Dr El-Essawi, “the minimal invasive concept has the potential to compensate even for an unbalanced distribution of [preoperative] risk factors, which we see as a strong argument for the validity of the concept.” Also prior to matching, no patients in the MiECC group had low cardiac output after surgery, whereas seven patients (5.6%) did in the cCPB group. Finally, transfusion rates and red blood cell transfusion quantity per patient were significantly lower in the MiECC group, both before and after matching.
The authors plan to continue their research to provide evidence for a broader application of MiECCs. “We will continue trying to identify other groups of patients that are expected to profit most from the concept,” says Dr El-Essawi. “Our goal is to increase the evidence for a shift in concept, in which the MiECC is the standard approach for extracorporeal circulation and conventional systems are the exception, [used only] for specific indications.”
Visit the European Journal of Cardio-Thoracic Surgery to read the full article: Impact of minimally invasive extracorporeal circuits on octogenarians undergoing coronary artery bypass grafting. Have we been looking in the wrong direction?
References
Anastasiadis K, Antonitsis P, Haidich AB, Argiriadou H, Deliopoulos A, Papakonstantinou C. Use of minimal extracorporeal circulation improves outcome after heart surgery; a systematic review and meta-analysis of randomized controlled trials. Int J Cardiol. 2013;164(2):158-169.
Baikoussis NG, Papakonstantinou NA, Apostolakis E. The "benefits" of the mini-extracorporeal circulation in the minimal invasive cardiac surgery era. J Cardiol. 2014. Jun;63(6):391-396.
El-Essawi A, Breitenbach I, Haupt B, Brouwer R, Baraki H, Harringer W. Impact of minimally invasive extracorporeal circuits on octogenarians undergoing coronary artery bypass grafting. Have we been looking in the wrong direction? Eur J Cardiothorac Surg. 2017;52(6):1175-1181.
Wang C, Hua K, Yin L, Wang Y, Li W. A Meta-Analysis of Miniaturized Versus Conventional Extracorporeal Circulation in Valve Surgery. Ann Thorac Surg. 2016;102(6):2099-2108.





