ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Highlighting Recent Research: Preoperative Renal Functional Reserve Predicts Risk of Acute Kidney Injury After Cardiac Surgery
Research published recently in The Annals of Thoracic Surgery suggests a new approach for evaluating a patient’s risk for acute kidney injury before they undergo cardiac surgery. Acute kidney injury (AKI) is a major complication of cardiac surgery, occurring in up to a third of patients (Kuitunen, 2006; Xie, 2017). Although patients with the highest risk can be identified with current screening measures, many patients who are not identified ahead of surgery go on to develop kidney injury. To evaluate a new approach for predicting postsurgical kidney injury risk in patients without underlying chronic kidney disease, Husain-Syed and colleagues tested preoperative renal functional reserve (RFR) in patients with normal resting glomerular filtration rates (Husain-Syed, 2018). The authors sought to determine the value of preoperative RFR in predicting postoperative AKI in these lower-risk patients. RFR is the difference between the resting glomerular filtration rate (GFR), the commonly accepted standard measure of renal function, and the highest measured GFR under the stress of a high protein load. Because GFR is not maximal in an unstressed healthy kidney, RFR represents the capacity of the kidney to increase filtration from baseline in response to stimuli (Sharma, 2014). The senior author of the study, Claudio Ronco of San Bortolo Hospital in Vicenza, Italy, emphasized that “current predictors only identify a selected group of patients. This new predictor raises the warning in a previously-considered ‘low risk’ population.”
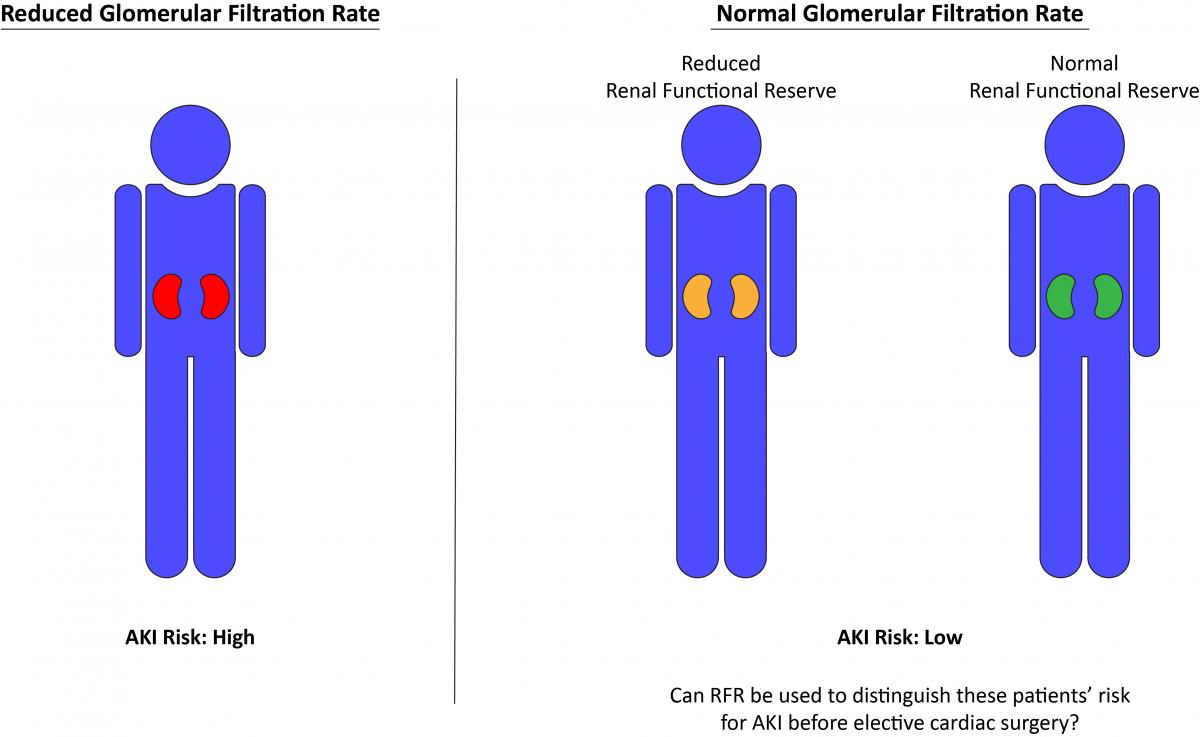
In this prospective observational study, the authors measured RFR using a high oral protein load test in 110 patients undergoing elective on-pump cardiac surgery. Importantly, all patients had GFR ≥60 ml/min/1.73 m2 and therefore would not be considered to have a high risk for AKI after surgery. Reduced preoperative RFR, defined as <30 ml/min/1.73 m2, was found in the majority of patients, with 4.5% having severe reduction (<10 ml/min/1.73 m2), 21.8% moderate reduction (≥10 and <20 ml/min/1.73 m2), and 46.4% mild reduction (≥20 and <30 ml/min/1.73 m2). Following surgery, 13.6% of patients developed AKI. Preoperative RFR was lower in patients who developed AKI than in those who did not, with the likelihood of AKI increasing with greater RFR reduction, and the authors found a cut-off RFR value of 15 ml/min/1.73 m2 to have good sensitivity (67%) and specificity (94%) for predicting postoperative AKI. Additionally, although preoperative biomarker levels did not differ between patients who did and did not develop AKI, postoperative levels of TIMP-2 and IGFBP7 were higher between 30 minutes and 12 hours after bypass in patients who developed AKI. Dr Ronco commented that the finding that reduced RFR predicted AKI was very important. “We can identify patients at risk that were considered normal before. This will have an impact on future practice, and at the same time it may explain different incidence in populations considered similar before.”
The authors suggest that RFR could be a novel indicator of increased risk for AKI following cardiac surgery. It is possible that reduced RFR could be employed ahead of nonurgent procedures to identify patients who might benefit from alternate surgical techniques such as off-pump surgery or to determine which patients should be more closely followed with biomarker testing after surgery. Dr Ronco encouraged cardiothoracic surgeons to collaborate with their hospital’s nephrologist. The take home message, he said, is that “chronic kidney disease does not start when creatinine rises but much earlier. The subclinical phase may be long and last years. In these years, however, the kidneys are not normal and they are more susceptible to exposures or insults.” For more discussion of the importance of the results, you can view this edition of Cappuccino with Claudio Ronco.
References
Husain-Syed F, Ferrari F, Sharma A, et al. Preoperative Renal Functional Reserve Predicts Risk of Acute Kidney Injury After Cardiac Operation. Ann Thorac Surg. 2018;105(4):1094-1101.
Kuitunen A, Vento A, Suojaranta-Ylinen R, Pettila V. Acute renal failure after cardiac surgery: evaluation of the RIFLE classification. Ann Thorac Surg. 2006;81(2):542-546.
Sharma A, Mucino MJ, Ronco C. Renal functional reserve and renal recovery after acute kidney injury. Nephron Clin Pract. 2014;127(1-4):94-100.
Xie X, Wan X, Ji X, et al. Reassessment of acute kidney injury after cardiac surgery: a retrospective study. Intern Med. 2017;56(3):275-282.