ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
Pulmonary Alveolar Microlithiasis: A Rare Indication for Pulmonary Transplantation
Brito DM, Kindelan AA, Casado PM, et al.. Pulmonary Alveolar Microlithiasis: A Rare Indication for Pulmonary Transplantation. October 2018. doi:10.25373/ctsnet.7185017.
Background
Pulmonary alveolar microlithiasis (PAM) is a rare lung disease characterized by widespread intra-alveolar accumulation of calcium phosphate deposits called microliths. Since the first macroscopic description of the disease by Malpighi almost 300 years ago, approximately 1,000 cases have been described worldwide, mainly in Asia and Europe, without clear gender predilection (1). PAM has a significant association with an autosomal recessive mutation of the SLC34A2 gene encoding NaPi-II transporter protein, the only phosphate transporter expressed in type II pneumocytes. This fact explains the accumulation of phosphate as a product of the degradation of pulmonary surfactant and the consequent formation of microliths. PAM is considered to be an autosomal recessive disorder because it is associated with consanguinity. Familial aggregation has been reported in 32% to 61% of cases (2). The diagnosis can be made before clinical manifestations by screening the family of the index patient or by using chest x-rays (CXR) or computed tomography (CT) scan in selected populations. The clinical course is not uniform and may be rapid or slow; the reasons for this variability are not yet known. Exertional dyspnea appears with progression of the disease. Cough may occur at any stage of disease and even the expectoration of microliths has been reported. Cor pulmonale and pulmonary fibrosis are terminal manifestations that lead to fatal respiratory or cardiac failure (3). In general, pharmacologic treatments seem to be ineffective for PAM. Lung transplantation is the only treatment that has been demonstrated to be effective in the current management of advanced stages of the disease. Currently, 17 procedures have been described worldwide, with results similar to those performed for other indications (4).
Case
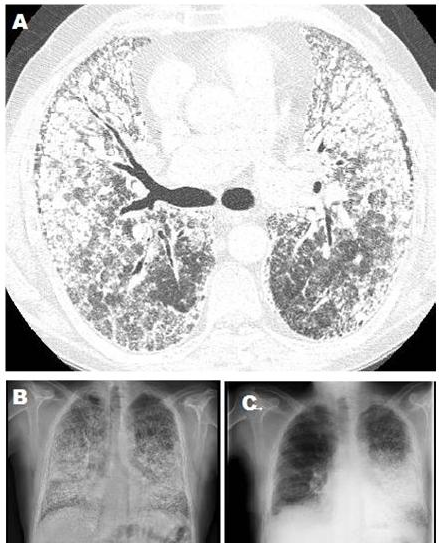
Figure 1. A) CT scan shows PAM findings. B) Chest X-rays previous to SLT. C) Chest X-rays 6° month follow-up right SLT.
The authors report the case of a 58-year-old nonsmoking man, with a medical history of bronchial asthma, who was otherwise healthy and who had a sister diagnosed with PAM. In 2007 he presented with progressive dyspnea. His CXR showing generalized nodular opacities and a CT scan showed multiple nodules of calcium density with an alveolar distribution that affected all lobes, septal and reticular thickening with predominance in the pulmonary bases, and small subpleural cysts (Figures 1A and 1B). After a nine-year period of medical management and follow-up with evidence of progression of respiratory dysfunction, the patient was referred for pretransplant evaluation with Medical Research Council grade III dyspnea. Respiratory function tests indicated a FVC 61%, FEV1 65%, Tiffenau index 105%, TLC 65%, and DLCO 32%. Resting arterial blood gas values on room air included pH 7.45, pCO2 32 mm Hg, pO2 59 mm Hg, HCO3 22 mmol/L, and SatO2 93%. The patient’s six-minute walk test distance was 330 m with O2 at 6 L/min, initial SatO2 was 98% and final SatO2 was 79%. Echocardiogram reported no pulmonary hypertension, a right ventricle ejection fraction of 51%, and a left ventricle ejection fraction of 67%. The CXR diameters were 19 cm right vertical, 21 cm left vertical, and 29 cm horizontal. Perfusion scintigraphy showed 54% of flow to the right lung. The authors decided to perform a single lung transplant (SLT). After 160 days on the waiting list, a right SLT was performed through a clamshell approach, finding a brownish and indurated lung parenchyma with marked bone metaplasia (Figure 2). A right pneumonectomy was performed after a pulmonary artery clamping test. The bronchial anastomosis was performed with continuous anterior and posterior nontelescoped sutures, and the vascular anastomoses were performed with monofilament running suture according to usual technique. During the reperfusion, there were no incidents and the ischemia time was 285 minutes. The patient was extubated after 24 hours and stayed in the intensive care unit for seven days. The postoperative clinical and radiological course was favorable with no incidents or complications, and the patient was discharged after 30 postoperative days in good condition. Clinical and radiological follow-up six months after transplant were satisfactory (Figure 1C).
Discussion
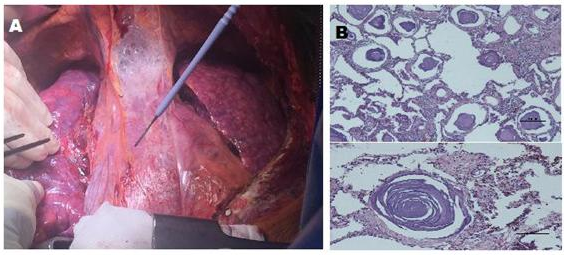
Figure 2. A) Intraoperative picture SLT (explanted right lung). B) Histopathological slide showing intra-alveolar accumulation of calcium deposits.
PAM is a rare genetic lung disease with an autosomal recessive trait caused by mutation of the SLC34A2 gene. PAM is characterized by accumulation of calcium microliths in the alveolar spaces. This is a progressive and terminal disease. The clinical course is not uniform and may be rapid or slow; the reasons for this variability are not yet known. The etiology, epidemiology, clinical findings and typical radiological images related to PAM have been thoroughly documented (2). In this case, the patient had a sister with the same diagnosis but the authors do not know her status. This patient had nine years of clinical follow-up from the diagnosis to pretransplant evaluation. Currently, lung transplant is the only effective therapy for PAM. At the current time, guidelines for the decision as to when transplantation should be undertaken have not been created due to the lack of well-defined prognostic indices and the insidious nature of PAM. When either right heart failure or severe respiratory failure requiring oxygen is present, transplantation should be considered (1). The first transplant in a patient with PAM was in 1992 in France by Bonnette and colleagues (5). At the present time, 17 worldwide lung transplants for PAM have been described; 12 were bilateral, four were single, and in one case the type of transplant was not reported (4). Some authors prefer bilateral transplant in patients with PAM because a single lung transplant could favor the appearance of persistent shunting of blood through the native lung. However, patients undergoing SLT for PAM have outcomes at 12 months to 15 years with comparable results to those undergoing bilateral lung transplant for PAM and transplant performed for others causes (6-9). To date, no recurrence after transplantation has been reported in single or bilateral lung transplant. The authors consider transplant to be an accepted and effective treatment in patients with advanced-stage PAM. Single lung transplant is a safe procedure with satisfactory and reproducible results, comparable to transplant performance for other pulmonary diseases.
Conclusion
PAM is a rare, progressive, and potentially fatal disease. Currently, lung transplant is the only accepted treatment option for selected patients in the final stages of the disease. The authors present their experience in the first case of transplant for PAM reported in Spain.
References
- CasA0 tellana G, Castellana G, Gentile M, Castellana R, Resta O. Pulmonary alveolar microlithiasis: review of the 1022 cases reported worldwide. Eur Respir Rev. 2015;24(138):607-620.
- Saito A, McCormack FX. Pulmonary alveolar microlithiasis. Clin Chest Med. 2016;37(3):441-448.
- Kashyap S, Mohapatra PR. Pulmonary alveolar microlithiasis. Lung India. 2013;30(2):143-147.
- Klikovits T, Slama A, Hoetzenecker K, et al. A rare indication for lung transplantation - pulmonary alveolar microlithiasis: institutional experience of five consecutive cases. Clin Transplant. 2016;30(4):429-434.
- Bonnette P, Bisson A, el Kadi NB, et al. Bilateral single lung transplantation. Complications and results in 14 patients. Eur J Cardiothorac Surg. 1992;6(10):550-554.
- Raffa H, El-Dakhakhny M, Al-Ibrahim K, Mansour MS. Single lung transplantation for alveolar microlithiasis: the first clinical report. Saudi J Kidney Dis Transpl. 1996;7(2):189-193.
- Jackson KB, Modry DL, Halenar J, L'abbe J, Winton TL, Lien DC. Single lung transplantation for pulmonary alveolar microlithiasis. J Heart Lung Transplant. 2001;20(2):226.
- Shadmehr MB, Arab M, Pejhan S, et al. Eight years of lung transplantation: experience of the National Research Institute of Tuberculosis and Lung Diseases. Transplant Proc. 2009;41(7):2887-2889.
- Borrelli R, Fossi A, Volterrani L, Voltolini L. Right single-lung transplantation for pulmonary alveolar microlithiasis. Eur J Cardiothorac Surg. 2014;45(2):e40.




