Introduction
Endovascular approaches are being increasingly utilized to treat a variety of thoracic aortic pathologies, including aneurysms, dissections, and transections [1-5]. Ongoing challenges to endovascular strategies for thoracic aortic pathology include relatively restricted endoprosthesis configurations, lack of FDA-approved devices of appropriate size for the small thoracic aorta, and problems associated with endovascular access. Here we present a case of a descending thoracic aortic pseudoaneurysm treated with a tapered endoprosthesis that illustrates a number of these challenges.
Case Presentation
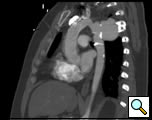
The patient is a 33 year old male with a history of juxtaductal coarctation who underwent a repair early in infancy. The patient had a recurrence of the coarctation and underwent a second open repair and left diaphragm plication at 2 years of age. He was lost to follow-up until recently when he presented to an emergency room with a several week history of hemoptysis and left back pain. The patient’s physical exam was remarkable only for a well-healed left thoracotomy incision. The patient was afebrile with equal blood pressures in all 4 extremities. The patient’s white count was normal. A CT scan of the chest demonstrated a saccular aneurysm of the proximal descending thoracic aorta measuring approximately 6cm in diameter (Figure 1). The patient was transferred to the Oregon Health and Sciences University for further management.
At our institution a dedicated CT angiogram of the chest was obtained to better define the morphology of the patient’s arch and aneurysm. This confirmed the finding of a saccular aneurysm just distal to the left subclavian artery takeoff. Because of the patient’s prior history of coarctation recurrence and repair, this was felt most likely to represent a pseudoaneurysm, possibly at the site of a patch repair. Aortic reconstructions of the CT angiogram showed no evidence for recurrence of the coarctation (Figure 2). There was, however, a size discrepancy in the diameter of the aorta above and below the aneurysm. The diameter of the aortic arch between the left carotid and left subclavian arteries was 13mm. The diameter of the descending thoracic aorta distal to the aneurysm was 23mm.
Because of the patient’s prior coarctation repairs and the morphology of the pseudoaneurysm, an endovascular repair was felt to be desirable. Based on preoperative measurements of the CT angiogram, a tapered endoprosthesis 9.5cm in length with 16mm proximal diameter and 20mm distal diameter (W.L. Gore & Associates, Inc.), originally marketed as an iliac limb, was selected for use. The patient was taken to the operating room. After induction of general anesthesia, percutaneous right femoral artery access was obtained and a measuring pigtail catheter was advanced into the distal aortic arch. An aortogram was performed which demonstrated the aortic arch and pseudoaneurysm morphology (Figure 3).
The length of the delivery catheter of the selected tapered endoprosthesis to be used for pseudoaneurysm repair was noted to be 55cm. Based on patient measurements using the right femoral measuring pigtail catheter, it was clear that the endoprosthesis delivery catheter was of insufficient length to allow deployment from the left common femoral artery. A 3cm transverse incision was therefore made over the left external iliac artery. The left external iliac artery was controlled and the patient was heparinized. An 18 Fr sheath was advanced from the left external iliac artery into the distal aorta.
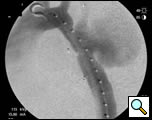
Selective angiography of the left subclavian artery was performed to confirm an intact posterior cerebral circulation. The proximal left subclavian artery was occluded with two 10mm Amplatzer vascular plugs which were introduced via the left external iliac sheath. An angiogram of the distal aortic arch and descending thoracic aorta was then performed to obtain a roadmap of the proximal and distal landing zones (Figure 4).
The tapered endoprosthesis was passed through the left external iliac sheath, positioned appropriately under fluoroscopic guidance, and deployed. An arch angiogram showed good endoprosthesis placement. Because of the relatively short proximal landing zone length (1cm), a 10 x 40mm Palmaz stent was placed and ballooned to 16mm proximally to achieve good radial fixation. The distal end of the endoprosthesis was ballooned. Completion angiography showed occlusion of the left subclavian artery and exclusion of the pseudoaneurysm (Figure 5).
The patient had an uneventful postoperative course. He had no left arm symptoms. A postoperative CT scan showed good placement of the endoprosthesis and vascular plugs and no endoleak (Figure 6). The patient was discharged to home on postoperative day 2.
Comment
This case illustrates a number of unique challenges faced by physicians attempting to treat thoracic aortic conditions with endovascular approaches. Problems with relatively restricted endoprosthesis configurations, lack of FDA-approved devices of appropriate size for the small thoracic aorta, and access and delivery issues all were encountered in this patient’s management. Selection of a tapered endoprosthesis marketed as an iliac limb allowed us to accommodate the size discrepancy between the proximal and distal landing zones with a single device. Selection of the iliac limb also enabled us to treat this patient’s relatively small aorta, which would not have accommodated currently available FDA-approved thoracic endoprostheses. An external iliac artery cutdown was necessary to provide more proximal vascular access to deploy the shorter delivery system of the tapered endoprosthesis. Awareness of these issues and access to the full spectrum of endovascular and surgical approaches allowed successful management of this patient using a minimally invasive approach.
References
- Dagenais F, Shetty R, Normand JP, Turcotte R, Mathieu P, Voisine P. Extended applications of thoracic aortic stent grafts. Ann Thorac Surg 2006;82:567-72.
- Kaya A, Heijmen RH, Overtoom TT, Vos JA, Morshuis WJ, Schepens MA. Thoracic stent grafting for acute aortic pathology. Ann Thorac Surg 2006;82:560-65.
- Saccani S, Busi M, Fragnito C, et al. Surgical repair and stent positioning for type A acute aortic dissection: a step forward? Ann Thorac Surg 2005;79:1761-63.
- Tehrani HY, Peterson BG, Katariya K, et al. Endovascular repair of thoracic aortic tears. Ann Thorac Surg 2006;82:873-78.
- Wheatley GH, III, Gurbuz AT, Rodriguez-Lopez JA, et al. Midterm outcome in 158 consecutive Gore TAG thoracic endoprostheses: single center experience. Ann Thorac Surg 2006;81:1570-77.