ALERT!
This site is not optimized for Internet Explorer 8 (or older).
Please upgrade to a newer version of Internet Explorer or use an alternate browser such as Chrome or Firefox.
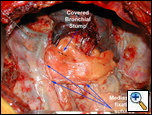
Pericardial Fat Pad Flap Buttress
Patient Selection
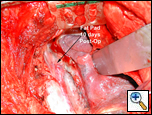 |
| Figure 1: Buttress of esophageal suture line at post-operative day 10. |
Buttressing suture/staple lines in thoracic surgery has been shown to promote healing and prevent breakdown, especially in situations where the native tissues have been compromised. There are a wide variety of tissue flaps that have been used within the chest ranging from pleura, muscle, to omentum [1]. The pericardial fat pad flap is a reliable buttress of a bronchial, pulmonary arterial or esophageal suture line (Figure 1) [2].
A pericardial fat pad flap is indicated for buttressing the bronchial suture/staple lines in various instances where chance of suture line failure may be increased by preoperative variables. These operative procedures include protection of the bronchial suture/staple lines after sleeve resection, or separating the suture lines after a concomitant bronchoplasty and pulmonary arterioplasty. In primary repairs of injuries to the tracheobronchial tree, a pericardial fat pad flap may serve to buttress the repair. Furthermore, it is useful in protecting post-pneumonectomy bronchial suture/staple lines particularly on the right side.
The fat pad is also useful in protecting bronchial suture/staple lines in patients who have undergone
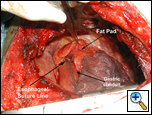 |
| Figure 2: Buttress of esophageal suture line. |
neoadjuvant chemoradiation or have had previous radiation to the bronchus, and in patients who will undergo postoperative radiation of the mediastinum [3]. Lastly, esophageal suture lines may be buttressed using a pericardial fat pad flap (Figure 2).
With adjuvant chemotherapy becoming standard of care for patients undergoing curative lung resections it is not known whether pericardial fat pad buttress of the bronchial staple line should be standard. Patients in whom the pericardial fat pad is not usable are those with infection or necrosis of the mediastinum (mediastinitis), scarring of this area (post-radiation), when a pericardial resection is indicated, and when there is inadequate bulk of the fat pad to be an effective buttress in thin / emaciated patients. If the fat pad is not usable, an alternative may be to use an intercostal muscle flap or a chest wall muscle flap.
Operative Steps
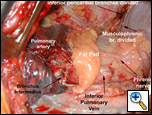
The pericardial fat pad is usually harvested at the completion of the resection; repair of injury, or after the esophageal anastomosis; however it can be performed before resection as well. When a portion of the lung has been removed, mobilization is then technically easier. The pericardial fat pad overlies the anterolateral aspect of the parietal pericardium and extends to include the phrenic nerve (Figure 3). The arterial supply of the fat pad is from the superior, middle and inferior pericardial branches of the internal mammary artery (Figure 4). The musculophrenic artery, a terminal branch of the internal thoracic artery, anastomoses with the inferior pericardial branches and the pericardiophrenic artery which accompanies the phrenic nerve. The vascular pedicle of the fat pad can be tailored according to the size of the fat pad needed and the need to preserve the phrenic nerve. When the anteroinferior portion of the fat pad is sufficient to provide an adequate buttress, the middle and superior branches pericardial branches can be preserved.
 |
 |
 |
| Figure 3a: Pericardial fat pad regions. | Figure 3b: Pericardial fat pad regions. | Figure 4: Blood supply to the pericardial fat pad. |
For larger buttressing needs only, the superior pericardial branches are preserved allowing the entire bulk of the pericardial fat pad to be used. In patients who have had a pneumonectomy the phrenic nerve can be sacrificed and the vascular supply is based on the pericardiophrenic artery and the superior pericardial branches of the internal thoracic artery. This increases the bulk and vascularity of the fat pad improving its reliability [2, 4]. Anecdotally, the paradoxical movement of the diaphragm due to phrenic nerve transection may lead to poor respiratory mechanics and inability to wean from the ventilator. In such cases, diaphragm plication may be necessary to improve respiratory mechanics [5, 6]. However, this is an unusual occurrence and it should not prevent the sacrifice of the phrenic nerve in harvesting the flap. The underlying pericardium can also be mobilized with the fat pad to add further thickness to it (Figure 5).
The pericardial fat pad can be mobilized by either an open or a thoracoscopic technique. Since the
 |
| Figure 5: Pericardial buttresses available after pneumonectomy. |
 |
| Figure 6: Post-pneumonectomy view of pericardial fat pad. |
primary operations where buttressing of a suture/staple line is needed are almost entirely done by an open technique, the indications for thoracoscopic mobilization are infrequent.
The open technique is described herein: Visualization and illumination of the antero-inferior recess of the chest is best obtained by the surgeon standing posteriorly, while wearing a headlight, with the operating table rotated to the opposite side and raised to an appropriate height. Use of a thoracotomy retractor by an assistant with superior blade elevating the lateral chest wall also improves exposure of this area (Figure 6). The cautery is set at 10 or 20 and the dissection is commenced over the diaphragm freeing the inferior most portion of the pericardial fat from the diaphragm. Alternately, sharp dissection can be used. Retraction is obtained by the use of a sponge stick pressing posteriorly or medially as required to facilitate the dissection. Visualized vessels are clipped using medium clips or using a 5 or 10mm endoscopic clip applier whose slim profile and long barrel facilitate access to this part of the chest. These are branches of the musculophrenic vessels.
The dissection is continued anteriorly and exposure is facilitated by the surgeon’s hand or a sponge stick retracting the fat pad posteriorly. Care is taken to avoid injury to the internal mammary vessels. The inferior pericardial branches to the fat pad are clipped and divided. During this stage of dissection it is not unusual for the blood pressure to drop due to compression of the heart and constant communication with the anesthesiologist is important. Cessation of retraction for a few minutes when the systolic pressure is less than 80 mmHg allows for recovery of the blood pressure (Video 1 and Video 2). If a larger bulk of tissue is required then the dissection is continued superiorly to the level of the azygos vein entry into the superior vena cava on the right and to the level of the aortic arch on the left. The middle pericardial vessels are divided during this dissection.
 |
| Figure 7: Pericardial fat pad mobilized. |
Attention is now turned to the deep aspect of the fat pad, which is dissected from the underlying pericardial surface using a combination of sharp and blunt dissection. The fat pad is retracted using either the surgeon’s hand or a ring clamp applied gently. As the fat pad is mobilized from the pericardium the posterior margin is defined either sharply or with cautery. When the phrenic nerve is to be preserved, the line of dissection is maintained anterior to the nerve and it is visualized at all times so the nerve is protected. The superior extent of the dissection is continued to the level of the anterior dissection (Figure 7 and Video 3).
In the case of a pneumonectomy, the pericardiophrenic vessels can be included with the pericardial fat pad, improving the blood supply and bulk of the buttress. The vessels and nerve are clipped and divided as they enter the diaphragm inferiorly and are reflected along with the fat pad as already described. If further thickness of the fat pad is needed, the underlying pericardium can be included with the flap and the resulting defect closed with a 2mm Gore-Tex patch (or Vicryl mesh) using interrupted sutures of 2-0 Prolene or multiple continuous sutures of the same material.
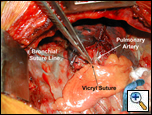
Once the fat pad has been mobilized it is then rotated over the hilum to cover the bronchial staple or suture line. Care is taken to avoid twisting the flap, keeping the mediastinal pleural surface laterally (smooth) and the pericardial surface (rough) medially. If there is tension on the flap then it is further mobilized from its anterior attachments to allow for extra length (Video 4). The distal end of the fat pad is pulled past the bronchial stump so that it is a more proximal portion that provides the buttress and not the most ischemic part of the fat pad. If a circumferential suture line is being buttressed the fat pad is wrapped around the suture line with either the pleural or the pericardial surface being applied to the suture line (Figure 8). The pericardial fat pad is sutured to the wall of the bronchus with interrupted horizontal mattress sutures of 4-0 Vicryl. The sutures are placed so when tied they are in the long axis of the flap and therefore should not interfere with the vascularity of the flap. The flap should form a hood over the staple line. The flap is then fixed at a location more proximally to the mediastinum with horizontal mattress sutures of 4-0 Vicryl to ensure that excessive movement or tension does not occur at the end serving as the buttress (Figure 9 and Video 5).
 |
 |
| Figure 8: Pericardial fat pad covering bronchial suture line. | Figure 9: Pericardial fat pad in place. |
Tips & Pitfalls
• Use a headlight
• For retraction use a sponge stick or a hand
• Set the cautery to 10 or 20.
• When dissecting the anterior margin of the fat pad keep the internal mammary artery in view.
• When dissecting the posterior margin of the fat pad protect the phrenic nerve.
• While mobilizing the inferior margin clip any visible blood vessels.
• Before suturing the fat pad to the bronchus, ensure it is not twisted or under excess tension.
• If there is insufficient bulk to the fat pad do not use it.
Results
The pericardial fat pad flap is a reliable and versatile buttress for a bronchial, tracheal or esophageal staple line [7]. The technique used to harvest the flap is well described and easily reproduced [2]. Inclusion of the pericardiophrenic vessels and the pericardium further add to the efficacy of the fat pad as a buttress [2, 4]. Its use in protecting the bronchial staple or suture line has been shown valuable particularly in patients who have received neoadjuvant therapy or postoperative radiation [3, 4]. In those patients undergoing a pneumonectomy it decreases the incidence of bronchopleural fistula and therefore the mortality of the procedure [4, 8]. It may also prevent bronchial stump breakdown in those patients who have to be ventilated after surgery [4].
Video 1
Video 2
Video 3
Video 4
Video 5
References
1. Anderson TM, Miller JI, Jr. Use of pleura, azygos vein, pericardium, and muscle flaps in tracheobronchial surgery. Ann Thorac Surg 1995;60:729-33.
2. Anderson TM, Miller JI, Jr. Surgical technique and application of pericardial fat pad and pericardiophrenic grafts. Ann Thorac Surg 1995;59:1590-1.
3. Greason KL, Miller DL, Clay RP, et al. Management of the irradiated bronchus after lobectomy for lung cancer. Ann Thorac Surg 2003;76:180-5.
4. Taghavi S, Marta GM, Lang G, et al. Bronchial stump coverage with a pedicled pericardial flap: an effective method for prevention of postpneumonectomy bronchopleural fistula. Ann Thorac Surg 2005;79:284-8.
5. Takeda S, Nakahara K, Fujii Y, Minami M, and Matsuda H. Plication of paralyzed hemidiaphragm after right sleeve pneumonectomy. Ann Thorac Surg, 1994;58:1755-7.
6. Goldstraw P and Jiao X. Pericardial repair after extensive resection: another use for the pedicled diaphragmatic flap. Ann Thorac Surg 1996;61:1112-4.
7. Brewer LA, 3rd, King EL, Lilly LJ, and Bai AF. Bronchial closure in pulmonary resection: a clinical and experimental study using a pedicled pericardial fat graft reinforcement. J Thorac Surg 1953;26:507-32.
8. Klepetko W, Taghavi S, Pereszlenyi A, et al. Impact of different coverage techniques on incidence of postpneumonectomy stump fistula. Eur J Cardiothorac Surg 1999;15:758-63.




