A 62-year-old Ukrainian man presented with facial swelling, chest wall varices, and a large mediastinal mass. He underwent core biopsy that demonstrated a mixed thymoma. Nine years previously, the patient had undergone an anterior thoracotomy and excisional biopsy of a mediastinal mass demonstrating necrotic tissue and no definitive diagnosis was made.
 |
 |
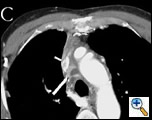
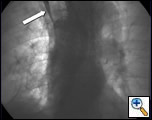
| Figure 1A Pre chemotherapy CT showing tumor at the confluence of the innominate veins (see arrows). | Figure 1B Pre chemotherapy CT showing tumor extending down into the right atrium (arrow). |
His physical examination was significant for head and upper extremity swelling, jugular venous distention without A or V waves, and superficial varices over the thorax. A computerized tomography (CT) scan (Figures 1A and 1B) demonstrated a mass in the mediastinum involving the superior vena cava (SVC) and extending into the right atrium. Echocardiography confirmed the intracardiac component. The patient was started on neoadjuvant therapy consisting of cisplatin, cyclophosphamide, and doxorubicin with plans for postoperative radiation therapy. A post chemotherapy CT scan demonstrated shrinkage of the mass (Figures 1C and 1D). A preoperative venogram confirmed the occluded SVC and well formed collaterals (Figure 2).
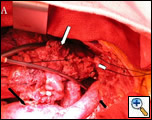
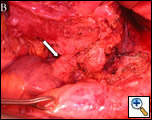
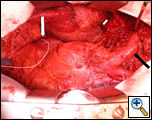
The patient was taken to the operating room and sternotomy performed after division of several large collateral chest wall veins. The pericardium was opened and resection of all thymic tissue was undertaken starting at the diaphragm (Figure 3). The SVC was transected at the confluence of the right subclavian and jugular veins and found to be filled with fibrotic tissue (Figure 4A). Frozen section examination of the luminal contents identified benign fibrotic tissue. The SVC was mobilized to the level of the right atrium en-bloc with the tumor, the azygos vein was divided, and a wedge resection of the medial aspect of the right upper lobe was performed. At this point, the tumor had been completely mobilized except for an intravascular extension through the SVC into the right atrium (Figure 4B).
The patient was placed on cardiopulmonary bypass via the aorta and inferior vena cava. The SVC was resected with the atrium and the tumor removed en-bloc (Figures 5-7). The atrium was closed and the patient weaned off cardiopulmonary bypass. The patient was extubated on postoperative day 2 and discharged home on postoperative day 7. Final pathology revealed a malignant thymoma with vascular and lung invasion.
Discussion
Thymomas are the most common tumor of the anterior mediastinum [1]. A widely accepted staging system, proposed by Masaoka and colleagues, is based on degree of invasiveness (Table 1) [2,3]. The WHO classification is a second staging system based on histology and has also been used [3]. This patient’s tumor was a Masaoka stage III tumor with an expected 10 year survival of approximately 50% [1,3,4]. However, the most important prognostic factor in stage III tumors has been shown to be invasion of the great vessels with 20 year survival of less than 30% in patients with stage III disease and great vessel involvement [4]. A phase II trial of neoadjuvant chemotherapy in Masaoka clinical stage III and IV thymoma was recently reported [5]; 14% of patients had a complete response and 63% had a partial response to preoperative chemotherapy. Complete resection was obtained in 76%. Survival was 95% at 5 years. These results show that long term survival is frequently achievable even in advanced tumors and that aggressive surgical resection and neoadjuvant therapy can benefit these patients.
While thymomas rarely present with a superior vena caval syndrome it has been reported [6-9]. Many of these instances include tumor extension into the right atrium or even the right ventricle. Neoadjuvant therapy may improve resectability and complete resection can require cardiopulmonary bypass. When the superior vena cava is chronically occluded with well-formed collaterals, reconstruction is not required and, as evidenced by this case, patients tolerate superior vena caval resection without difficulty [10].
References
- Johnson SB, Eng TY, Giaccone G, and Thomas CR, Jr. Thymoma: update for the new millennium. Oncologist 2001;6:239-46.
- Masaoka A, Monden Y, Nakahara K, and Tanioka T. Follow-up study of thymomas with special reference to their clinical stages. Cancer 1981;48:2485-92.
- Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer 2002;94:624-32.
- Okumura M, Miyoshi S, Takeuchi Y, et al. Results of surgical treatment of thymomas with special reference to the involved organs. J Thorac Cardiovasc Surg 1999;117:605-13.
- Kim ES, Putnam JB, Komaki R, et al. Phase II study of a multidisciplinary approach with induction chemotherapy, followed by surgical resection, radiation therapy, and consolidation chemotherapy for unresectable malignant thymomas: final report. Lung Cancer 2004;44:369-79.
- Gill K, Ettles DF, and Nicholson AA. Recurrent superior vena caval obstruction due to invasion by malignant thymoma: treatment using a stent-graft. Br J Radiol 2000;73:1015-7.
- Mineo TC, Ambrogi V, Nofroni I, and Pistolese C. Mediastinoscopy in superior vena cava obstruction: analysis of 80 consecutive patients. Ann Thorac Surg 1999;68:223-6.
- Terada Y, Ono N, Noguchi T, et al. A case of thymoma protruding into the superior vena cava through the thymic vein. Ann Thorac Surg 2004;77:1088-90.
- Tseng YL, Wang ST, Wu MH, et al. Thymic carcinoma: involvement of great vessels indicates poor prognosis. Ann Thorac Surg 2003;76:1041-5.
- Venuta F, Rendina EA, and Coloni GF. Surgery of the Superior Vena Cava: Resection and Reconstruction. CTSNet: Thoracic Techniques, 2003.